Many variables have been associated with psychiatric length of stay, but study findings have deemed the variables equivocal. These variables include gender, age, diagnosis, comorbid disorders, type of treatment received, and psychosocial factors.
Hopko and colleagues (
1) analyzed "alternate data, such as those obtained during the initial assessment in the hospital" to predict which patients would use inpatient mental health services for an extended period of time. These researchers found that three factors—the patient's resistance to treatment, positive symptoms, and psychological discomfort—of the anchored version of the Brief Psychiatric Rating Scale (BPRS-A) (
2) were helpful in predicting length of stay. Although there is substantial research that suggests assessment data may be beneficial in identifying patients who require longer hospitalization and additional referrals (
1,
3,
4,
5), it was not certain whether the expanded version of the Brief Psychiatric Rating Scale (BPRS-E) (
6) would provide such data. In addition, it was not clear whether assessment data would be useful in predicting length of stay among patients with the severe and persistent mental illness that is characteristic of patients in Utah State Hospital and other long-term psychiatric institutions.
The study reported here adds to the existing literature in that few studies include long-stay psychiatric patients as subjects of investigation. To date, most research has focused on acute hospitalizations and placement thereafter. This study offers professionals a more longitudinal view of psychiatric admissions.
We hypothesized that BPRS-E data from Utah State Hospital patients would produce a model with four or five factors resembling factors found by Hopko and colleagues (
1) and that only the resistance factor they identified would be predictive of length of stay. We hypothesized that only the resistance factor would attribute to more long-term hospitalizations because it continues to be present following acute care. Because severe and persistent mental illness was characteristic of the sample we studied, we hypothesized that psychological discomfort and positive symptoms would resolve easily and quickly with medication management and, therefore, would not be predictive of length of stay.
Methods
A total of 222 adult psychiatric inpatients participated in this study (116 men and 106 women, mean±SD age= 42.7±12.3 years). Eligible participants were referred to the hospital for a first admission between January 1, 1998, and December 31, 2001; had completed the BPRS-E within 72 hours of admission; were discharged at the time of data analyses; and were not transferred to the forensic unit census. Analyses of the data occurred in May 2002.
The BPRS-E is a 24-item, semistructured interview that rates psychopathological symptoms that were present during the previous two weeks on a Likert scale from 1, not present, to 7, extremely severe. Anchor points and a manual are provided for scoring discernment (
6). Symptoms measured by the BPRS-E are somatic concerns, anxiety, depression, suicidality, guilt, hostility, elevated mood, grandiosity, suspiciousness, hallucinations, unusual thought content, bizarre behavior, self-neglect, disorientation, conceptual disorganization, blunted affect, emotional withdrawal, motor retardation, tension, uncooperativeness, excitement, distractibility, motor hyperactivity, and mannerisms and posturing.
Following Utah State Hospital's human subjects review board approval, the BPRS-E was administered to participants within 72 hours after their admission to the hospital. Interviews were conducted by the hospital's psychology staff members who had completed competency scoring training and demonstrated an interrater and intrarater reliability of at least .80. BPRS-E scoring depended on the interview, behavioral observations, psychiatric records, and staff report. Demographic information, BPRS-E data, diagnosis, and length of stay were systemically indexed into a database and analyzed by using spreadsheet and SPSS statistical software.
Results
Descriptive statistics for the total sample indicated that the mean length of stay was 118.4±88.6 days. The ethnic composition of the group was 90 percent Caucasian (N=199), 8 percent Hispanic (N=17), and 2 percent Native American (N=4), with African Americans (N=1) and Asian Americans (N=1) each accounting for less than 1 percent of the sample.
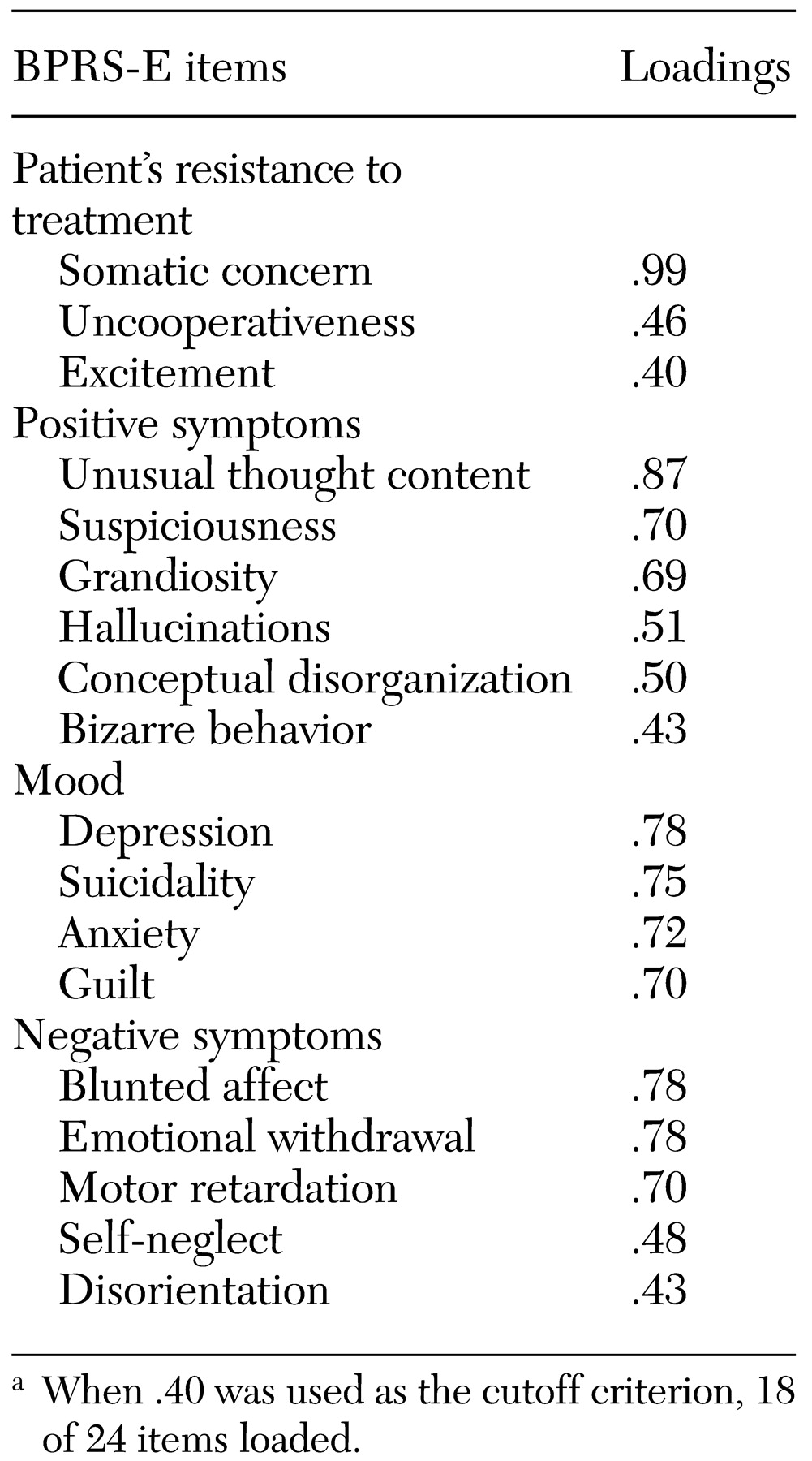
Principal components analysis, with varimax rotation, was used to find a solution that fit the collected data. As shown in
Table 1, the analysis produced a model with four factors: patient's resistance to treatment, positive symptoms, mood, and negative symptoms. Eighteen items loaded on the factors, which accounted for 68 percent of the variance, with the negative symptoms factor solely accounting for 42 percent.
Regression methods were used to analyze the 24 individual items of the BPRS-E to determine whether any item or subset of items would be able to sufficiently predict length of stay. Motor retardation was the most predictive item, accounting for 13 percent of the variance (F=8.62, df=23, 221, p<.004) followed by blunted affect (9 percent) and disorientation (6 percent). All of these items loaded on the negative symptoms factor. A second regression analysis was conducted on the four factors and found that the positive symptoms factor was most predictive, but this factor accounted for only 5 percent of the variance (F=11.07, df=3, 221, p<.001). Because all 24 items of the BPRS-E accounted for only 14 percent of the variance and because regression analyses of the factors had a substantial amount of unexplained error, further analyses were conducted.
Discriminant analysis was conducted on the factors to explore differences between patients who were hospitalized longer than the mean and patients who were below or at the mean. Results indicated that the negative symptoms factor correctly classified 94 percent (N=208) of the sample (F=28.17, df=1, 207, p<.001).
Discussion
The purpose of this study was to examine the usefulness of the BPRS-E in predicting inpatient length of stay. Findings of factor regressions were discrepant from all previous studies; this may be due to the fact that only the 18 items loading were included in our model. BPRS-E data yielded four factors as hypothesized. Discriminant analysis of the four factors derived from our study indicated that the negative symptoms factor accurately predicted whether length of stay would exceed the mean in 94 percent of cases (N=208). Furthermore, items loading on the negative symptoms factor accounted for 13 percent of the variance.
These findings suggest that the negative symptoms exhibited by patients may be helpful in predicting length of stay in a long-stay population. Total BPRS-E item scores and regression of the factors did not explain as much of the variance as did the symptoms that loaded on the negative factor. Therefore, clinicians may opt to examine negative symptoms when making predictions about the length of stay of patients with severe and persistent mental illness. Negative symptoms tend to be more treatment resistant than other symptoms and syndromes measured by the BPRS-E. Therefore, use of negative symptoms as predictors of length of stay for the Utah State Hospital population is feasible.
Other variables that should be examined in future studies of state hospital populations include number of previous hospitalizations, marital status, and socioeconomic status. In addition, a larger, more heterogeneous sample would allow greater generalizability of the results.
Overall, the BPRS-E demonstrated sufficient predictive validity for inpatient length of stay. Therefore, Utah State Hospital will incorporate intake assessment information in treatment and discharge planning, as well as analyze future financial expenditures associated with length of stay to confirm the utility of the BPRS-E in this area.