The prevalence of posttraumatic stress disorder (PTSD) is estimated to range from 9 to 12 percent in the general population (
1,
2). These figures likely underestimate the prevalence among residents of urban, economically disadvantaged areas, because this population is at higher risk than the general population of exposure to traumatic events. This greater risk of victimization among urban residents can be attributed to a variety of factors, including low socioeconomic status and high rates of violence in the inner city. Despite the potential high rate of PTSD in the urban population, trauma is likely underrecognized and PTSD is often underdiagnosed (
3,
4). These findings are compounded by the possibility that mental illness, particularly affective disorders, tends to be underdiagnosed in the African-American community (
5).
In this study, we used a survey design to examine whether the rates of trauma and PTSD among low-income African-American mental health patients from an urban area were higher than the rates that have been reported for the general population. We examined whether PTSD was underdiagnosed in our study population. We also examined whether persons with PTSD were more likely than those without PTSD to have worse clinical and quality-of-life characteristics. Finally, we examined whether persons with PTSD were more likely than those without PTSD to be at higher risk of developing comorbid psychiatric diagnoses.
Methods
African-American patients were recruited from an urban outpatient mental health clinic in Atlanta, Georgia, during an 18-month period from 2001 to 2002. Patients were recruited if they presented for treatment that was not focused on a crisis. The study was limited to African Americans because no studies have specifically examined PTSD among African Americans in the inner city, this group is understudied, and the vast majority of patients at this clinic are African American. We approached 200 patients, and 184 completed our survey. Patients were eligible for our study if they were aged 18 to 75 years, were able to understand English, and had been active patients in the clinic for two or more years. Patients were excluded from our study if they were mentally retarded, scored under 24 on the Mini-Mental State Exam, or were not able to give valid informed consent. This study was approved by the institutional review board of Emory University and the research oversight committee of Grady Health System. We obtained informed consent from all patients.
The initial survey included demographic information; the Mini-Mental State Exam; the traumatic events inventory, which is a 13-question self-report that assesses traumatic events, frequency of events, age at worst incident, and feelings of terror, horror, and helplessness (unpublished scale, Rothbaum BO, Davidson JR, 2000); and the PTSD Symptom Scale (PSS), which is a 17-item self-report that mirrors
DSM-IV criteria for PTSD and has good psychometric properties (
6).
A master's-level research assistant administered all measures aloud because of low literacy rates. Patients in the waiting room were approached every day of the week and all hours of clinic operation to prevent bias in the timing of survey completion. A total of 184 patients completed the interview and were included in the analysis. The average number of monthly visits among participants was 1.2, which is comparable to the average for the entire clinic of 1.0 visit each month. This finding suggests that the sample population was similar to the overall clinic population. Seventy-two of the surveyed patients were then chosen at random from a list of participants to undergo the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), which was conducted by a trained interviewer who was blind to initial data. These patients' psychiatric charts were then reviewed to obtain chart diagnoses.
Data were maintained in SPSS version 12.0 for personal computers. Categorical variables were analyzed with chi square statistics. Continuous variables were examined with analysis of variance.
Results
Sixty-six of the participants (36 percent) were men and 118 (64 percent) were women. The mean±SD age was 45.1±11.4 years, ranging from 21 to 72 years. A majority of the sample was impoverished: 78 (42 percent) took home less than $500 each month, 81 (44 percent) took home between $500 and $1,000 each month, and 23 (13 percent) were currently homeless. A total of 102 (55 percent) had experienced a potentially lethal attack, 89 (48 percent) had experienced a serious accident or injury, and 53 females (45 percent of the females) had experienced a sexual assault. A total of 72 participants (39 percent) acknowledged past or present substance abuse or dependence: 70 (38 percent) in the past and 12 (7 percent) in the present. A total of 153 participants (83 percent) experienced a traumatic event at some point in their lifetime that was a criterion A stressor for PTSD, as defined in DSM-IV.
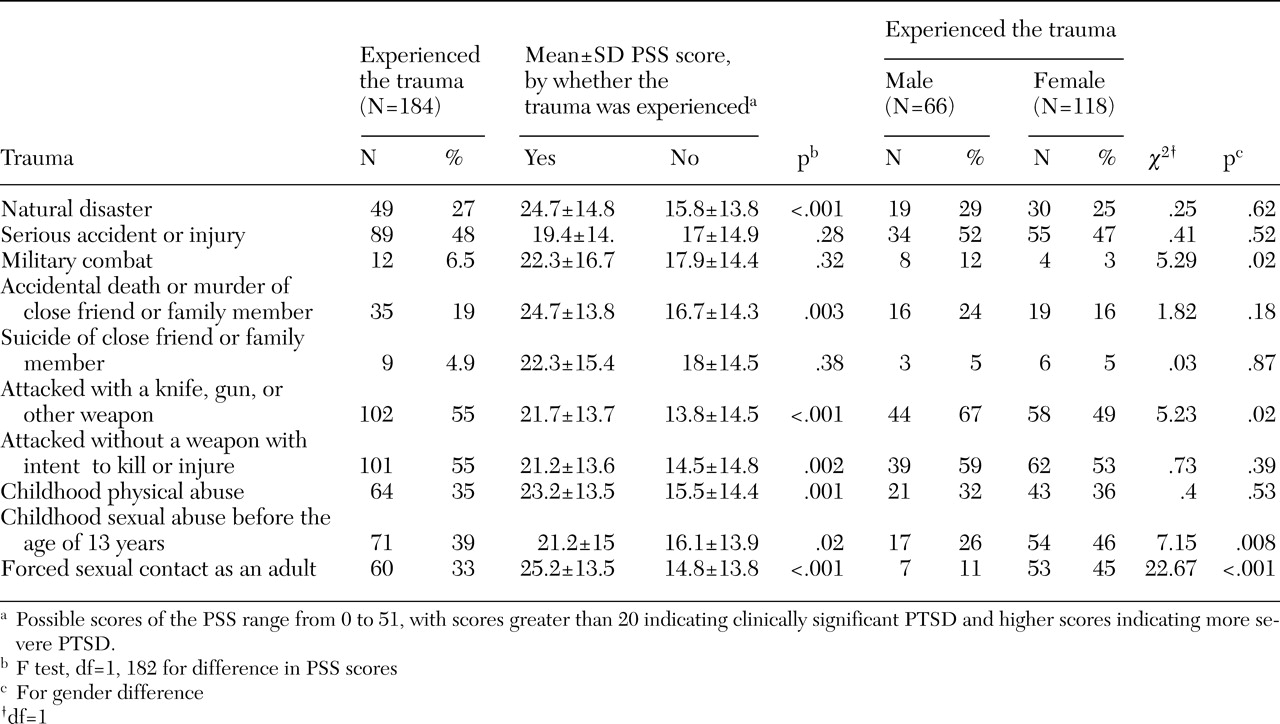
Twenty-eight participants (15 percent) had experienced one potentially traumatic event, 29 (16 percent) had experienced two events, 35 (19 percent) had experienced three events, 33 (18 percent) had experienced four events, and 47 (26 percent) had experienced five or more events. As shown in
Table 1, women were significantly more likely than men to experience sexual assaults across their lifespan, and men were more likely than women to experience military combat or to be attacked with a weapon.
When combined with the traumatic events inventory, the PSS provides a full diagnostic screen for the DSM-IV diagnosis of PTSD. Among the 184 participants in our study, 80 (43 percent) met criteria for PTSD, as measured by the PSS. Among the 72 participants who completed the SCID-I, 29 (40 percent) met criteria for PTSD, as measured by the SCID-I. Those with a SCID-based diagnosis of PTSD had significantly higher scores on the PSS than those without such a diagnosis (mean score of 30.9± 12.19 compared with 12.9± 13.08; F=34.4, df=1, 70, p<.001). Possible PSS scores range from 0 to 51, with higher scores indicating higher severity of symptoms.
We examined whether there was a relationship between type or frequency of trauma and the presence of PTSD symptoms.
Table 1 shows that a majority of the specific traumatic experiences were related to a statistically significant difference in PSS total score. Because of the large numbers of patients who reported more than one type of trauma, we examined the relationship between the number of types of traumatic experiences and traumatic symptom severity (PSS score) and found a significant correlation (r=.43, p<.001).
Among the 72 participants who were interviewed by use of the SCID-I, we found that patients with substance use disorders, either current (F=9.64, df=1, 182, p<.001) or past (F=7.89, df=1, 182, p<.01), had more PTSD symptoms and were more likely to have a SCID-based diagnosis of PTSD than patients who did not have a substance use disorder (χ2=5.37, df=1, p=.02). Also, among these 72 participants, those with a reported history of attempting suicide had significantly more PTSD symptoms (F=12.6, df=1, 182, p<.001) and were significantly more likely to have a SCID-based diagnosis of PTSD (χ2= 5.46, df=1, p=.02). Additionally, those who were currently homeless had more PTSD symptoms, although this trend was not statistically significant.
Among these 72 participants, participants who met SCID criteria for PTSD had more comorbid psychiatric diagnoses, as measured by the SCID-I (mean=3.3±1.2) than those who did not (mean=1.7±1.l; F=30.9, df=1, 70, p<.001). Patients with PTSD were more likely than those without PTSD to meet SCID criteria for major depression (χ2= 6.5, df=1, p=.01) and for nonschizophrenic psychotic disorders (χ2=4.8, df=1, p=.03).
Consistent with other data that suggested that early childhood trauma and abuse correlates with adult PTSD, we found that participants who reported an unstable childhood family environment were more likely to have a SCID-based diagnosis of PTSD (χ2=14.28, df=1, p<.001) and higher PSS scores (F=24.8, df=1, 182, p<.001).
The clinic charts were requested for all 72 patients who were interviewed with the SCID-I. Twenty-nine of these participants (40 percent) had PTSD, as diagnosed by the SCID-I. A total of 66 patients' charts were available for examination, and 26 of these patients (39 percent) had PTSD as diagnosed by the SCID-I. The most common chart diagnosis for those with a SCID-based diagnosis of PTSD were depression (19 participants, or 73 percent) and psychotic disorders other than schizophrenia (12 participants, or 46 percent). PTSD was vastly underdiagnosed. Although we found that 39 percent of the patients who were interviewed with the SCID-I met criteria for PTSD, these rates were not reflected in the clinic charts. Among the 66 charts reviewed, only four charts (6 percent) listed a diagnosis of PTSD. Furthermore, of the 26 participants who met SCID-I criteria for PTSD, only three charts (11 percent) listed a diagnosis of PTSD.
Discussion
In this study, we found that African Americans with low socioeconomic status who went to an urban mental health clinic were at very high risk of having experienced violence and traumatic events. We found high rates of severe trauma (83 percent) and PTSD (44 percent). We also found that the extent of previous trauma significantly correlated with PTSD symptom severity. Participants with PTSD were more likely than those without PTSD to have multiple comorbidities, primarily nonschizophrenic psychosis and depression. Compared with participants without PTSD, those with PTSD were more likely to have attempted suicide and to have a history of substance use disorders.
Despite these high rates of trauma and PTSD, this population is not currently identified as being in need of treatment, as reflected by our finding that only 11 percent of those with a SCID-based diagnosis of PTSD had a chart diagnosis of PTSD. We believe that the underdiagnosis of PTSD is the case not only in our mental health center but also nationally. In several studies that examined prevalence of PTSD among patients with severe mental illness, similar high rates of PTSD have been reported (
3,
4). However, our data and data from these previous studies had significant differences: our participants were from a racial minority group, we found that PTSD was associated with higher rates of suicide attempts and comorbid substance use disorders, and we compared chart diagnosis with a SCID-based diagnosis of PTSD. Furthermore, our study included all patients in the clinic, not just those who met criteria for severe mental illness.
This study is consistent with previous work that examined the frequency and impact of violence on impoverished, inner-city communities (
7,
8). Our data suggest that because of the heterogeneous nature of PTSD, it may be the underlying diagnosis among patients with a variety of clinical presentations (
4,
9). Individuals who seek psychiatric services, especially in inner-city areas with high rates of violence, may be experiencing residual effects of exposure to traumatic events. Failure to diagnose and treat PTSD may prolong the total duration of psychiatric treatment and may result in poorer treatment outcomes (
10).
This study had several limitations. We were unable to determine if the rates of PTSD and trauma we report are applicable to all African Americans with low socioeconomic status who live in an urban area or if these rates are specific to those who seek treatment for mental illness. Further studies are needed to directly address the rates of PTSD among residents of inner-city areas with high rates of violence who do not seek treatment for mental illness.