Posttraumatic stress disorder (PTSD) is an anxiety disorder that may develop after exposure to extreme trauma (
1) and is common among persons with substance use disorders (
2,
3). The Australian National Survey of Mental Health and Wellbeing (NSMHWB) found that one-third of persons with an opioid use disorder met criteria for current PTSD, compared with 1 percent of the general population. The prevalence of PTSD was higher among individuals with an opioid use disorder than among those with disorders involving all other drug classes (
4).
PTSD places a significant burden on persons with heroin dependence and presents a significant challenge to treatment providers. In a large Australian cohort of heroin users (the Australian Treatment Outcome Study), individuals with PTSD were found to present with a more severe clinical profile than those without PTSD (
5). Specifically, individuals with PTSD were less likely to be employed, had more extensive polydrug use histories, were more likely to have a history of overdose, and reported poorer general physical health and greater psychopathology (
5).
Given this clinical profile, it is not surprising that PTSD has consistently been associated with poorer substance abuse treatment outcomes, including higher relapse and readmission rates and more ongoing drug use (
6,
7,
8). Moreover, it appears that these poorer treatment outcomes are specific to PTSD rather than to greater psychopathology in general (
9). Consequently, persons with comorbid opiate dependence and PTSD have been found to consume more treatment services (
10,
11). The only study to establish cost values for these differences in service use estimated that patients with both a substance use disorder and PTSD incurred an average cost of $4,042 (U.S. dollars) during a six-month period, compared with $780 for patients with a substance use disorder alone (
10,
11).
Information about the use and costs of services is crucial for understanding the overall impact of comorbid PTSD on the health care system and may be used by health policy makers and planners to determine the allocation of resources. However, these studies of service use and cost have been limited in that they have not used prospective longitudinal designs and have measured only the use of inpatient programs. Such designs may miss observations in which treatment is merely diverted to another unmeasured setting, such as maintenance therapy, thus underestimating service use and the associated costs (
12). In addition, no studies have examined the costs of treatment as they relate to treatment outcome.
Using data collected as part of the New South Wales component of the Australian Treatment Outcome Study (ATOS) (
13), a naturalistic longitudinal study of treatment outcomes for heroin dependence, we compared the use of opiate treatment over 12 months among persons with heroin dependence and PTSD and those with heroin dependence alone; the cost of treatment received over 12 months for persons with heroin dependence and PTSD and those with heroin dependence alone; and the treatment outcomes for persons with heroin dependence and PTSD and those with heroin dependence alone.
Methods
Participants were recruited from 19 agencies that treated heroin dependence in the greater Sydney region from February 2001 to August 2002. The agencies were randomly selected from within treatment modality (for example, maintenance therapies, detoxification, and residential rehabilitation) and stratified by regional health area. The agencies represent the major treatment modalities: methadone or buprenorphine maintenance, residential rehabilitation, and detoxification. Heroin users who were not currently in treatment were recruited from needle and syringe programs in the regional health areas from which treatment entrants were recruited. (Under the Australian health care system, heroin users are given access to free, clean needles and syringes to discourage use of dirty needles.) Ethical approval was granted by the human ethics review committees of all participating area health services and the University of New South Wales.
The total baseline sample consisted of 615 heroin users: 201 who were entering maintenance therapies, 201 who were entering detoxification, 133 who were entering residential rehabilitation, and 80 who were not receiving treatment. Participants were reinterviewed 12 months after they entered treatment. All participants provided written informed consent were paid $20 (Australian dollars) for completing each interview. Further details of the recruitment procedure can be found elsewhere (
13).
Structured interview
A structured interview was administered to participants at baseline and at 12-month follow-up. Lifetime
DSM-IV diagnoses of PTSD were obtained at baseline by using the version of the Composite International Diagnostic Interview (CIDI) used in the NSMHWB (
2). Drug use over the month preceding the interview was measured by using the Opiate Treatment Index (OTI) (
14). The OTI measures drug use in the previous 28 days. Average use over that period (in the form of a Q score) is calculated on the basis of recent consumption and the intervals between consumption. Q scores may be interpreted as follows: 0, abstinence; .01 to .13, once a week or less; .14 to .99, more than once a week; 1.00 to 1.99, daily; and 2.00 or more, more than once a day.
DSM-IV diagnoses of current major depression (in the preceding month) and
ICD-10 diagnoses of borderline personality disorder were obtained by using a modified version of the CIDI used in the NSMHWB (
2). Diagnoses of antisocial personality disorder were obtained by using a version of the Diagnostic Interview Schedule modified to obtain
DSM-IV diagnoses. General physical and mental health were assessed by using the Short Form-12 (SF-12), on which lower scores indicate poorer health (
15).
The 12-month interview was an abbreviated form of the baseline interview and included sections on treatment history, drug use history, heroin overdose history, general physical and mental health, and current major depression, using the instruments described above. Information elicited on treatment history included the number of times participants had started different types of treatment over the follow-up period and the duration of each treatment episode.
Assessment of opiate treatment costs
Costs to the government were estimated for all opiate treatment services used by ATOS participants. Total treatment costs included participants' total stay in their index treatment and their use of other opiate treatment services during the 12-month follow-up period. Total treatment costs were the sum of the number of days in each treatment type multiplied by the appropriate unit cost. Time in index treatment was obtained through file audits, and information about subsequent treatment episodes was based on participants' self-reported data collected through structured interviews at follow-up.
The unit costs applied to these measured amounts of opiate treatment were drawn from a variety of published national sources (
16,
17,
18,
19). In cases in which a standard price per treatment episode was not available, cost information from treatment providers was used. Because the study was conducted over a period of several years, all costs were standardized to 2002 Australian dollars by using the Consumer Health Price Index (
20). Full details of the unit costs for each treatment type have been reported by Shanahan and colleagues (
21) and may be obtained from the authors.
Statistical analysis
For continuous data, t tests were used. For dichotomous categorical variables, odds ratios (ORs) with 95 percent confidence intervals (CIs) are reported. Differences between baseline and follow-up were examined by using generalized estimating equations (
22), controlling for the proportion of time spent in treatment, the number of treatment episodes, and the interaction between time and PTSD. In cases in which the interaction effect was not significant, the effect was removed from the model.
The median costs of opiate treatment for the 12-month follow-up period are presented in addition to means and standard deviations because of highly skewed distributions. Because cost data were highly skewed, the data were analyzed with use of a two-part model (
23). In the first part of this procedure, logistic regression was used to derive ORs of the probability of having used any opiate treatment—that is, the probability of having nonzero costs. The second part of the model examined the expected cost of opiate treatment use for participants with nonzero costs. Ordinary least squares regression was conducted on the log cost of treatment. This transformation was necessary to satisfy the conditions of normality and homoscedasticity. A cost ratio of the estimated opiate treatment cost was obtained by multiplying the probability of having used opiate treatment by the expected cost conditional on being a user.
Results
Sample characteristics
A total of 495 study participants (80 percent) were successfully reinterviewed at 12-month follow-up: 167 in maintenance therapy (84 percent), 171 undergoing detoxification (85 percent), 104 undergoing residential rehabilitation (78 percent), and 53 in the nontreatment group (66 percent). A further 32 individuals (5 percent) were known to be incarcerated, and five (.8 percent) were known to be deceased. The mean±SD duration to follow-up was 362.5±51.3 days.
At baseline, the mean age of the study participants was 29.2±7.8 years (range, 18 to 56), and 321 participants (65 percent) were men. The sample had completed a mean of 10.1±1.7 years of education (range, 2 to 12); 154 (31 percent) had completed a trade or technical course, and 31 (6 percent) had completed a university degree. A total of 182 individuals (37 percent) had a prison history. The main sources of income were government allowances (N=222, or 45 percent), criminal activity (N=113, or 23 percent), and wage or salary (N=93, or 19 percent).
The mean age of first intoxication was 13.7±3.3 years, and the mean age for first use of heroin was 19.6±5.2 years. The mean lifetime duration of heroin use was 9.6±7.6 years. The median OTI heroin use score was 2.0 (range, .04 to 33.3). The sample had used a mean of 9.1±1.7 drug classes over their lifetimes (range, 2 to 11) and a mean of 4.8±1.7 drug classes in the preceding month. A total of 126 individuals (26 percent) met criteria for current major depression, 206 (42 percent) met criteria for PTSD, 221 (45 percent) screened positive for borderline personality disorder, and 349 (71 percent) met criteria for antisocial personality disorder. Overall, the demographic characteristics, drug use histories, and polydrug use of the sample are typical of both Australian and international study samples of heroin users (
24,
25,
26).
Study participants who were reinterviewed and those who were lost to follow-up did not differ significantly in terms of age, gender, treatment history, heroin use at baseline, suicide history, major depression at baseline, PTSD, or the presence or absence of a personality disorder. The only notable difference between the reinterviewed sample and the participants who were lost to follow-up was that participants in the treatment groups were more likely to be followed up than those in the nontreatment group (442, or 82 percent, compared with 53, or 66 percent; OR=2.42, CI=1.45 to 4.05). Thus the sample of participants who were reinterviewed at 12-month follow-up was broadly representative of the initial sample.
Treatment exposure
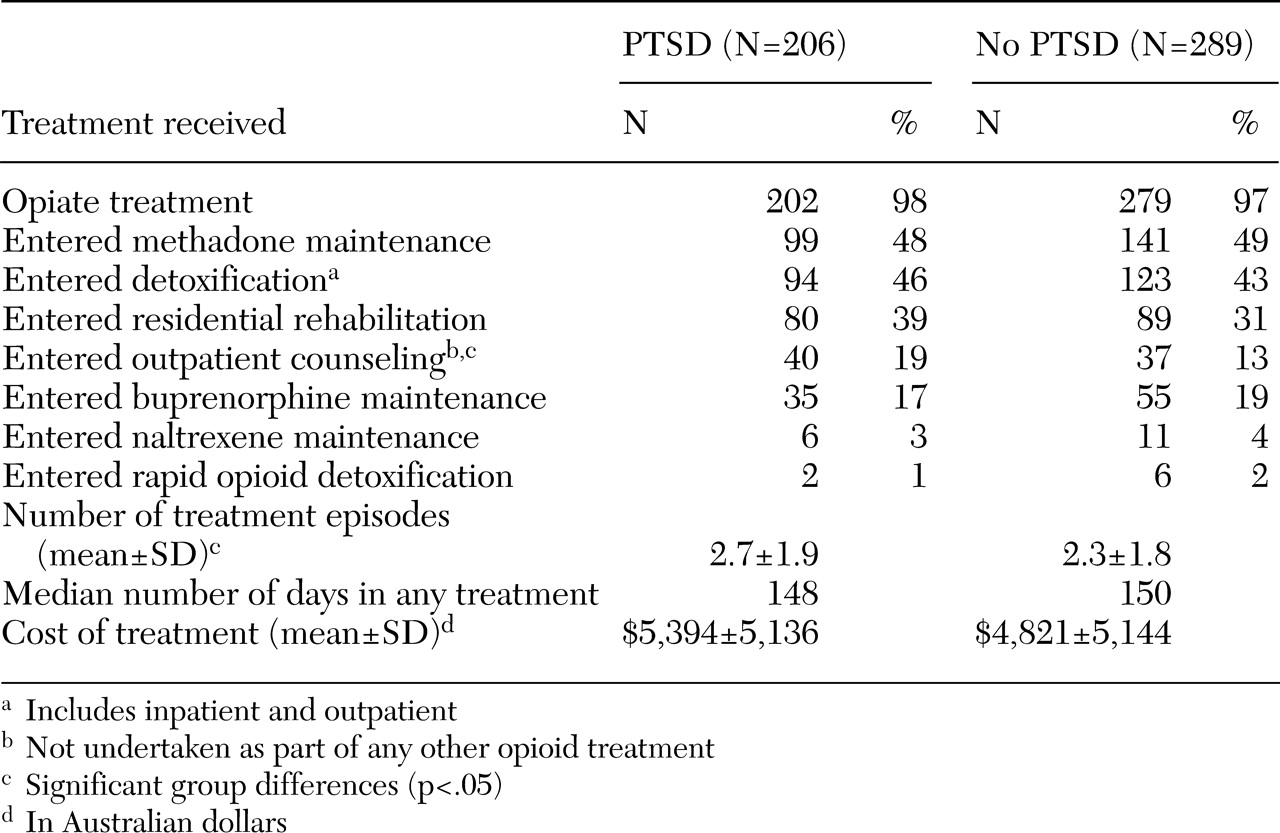
Fifty-nine percent of participants both with and without PTSD (N=122 and N=171, respectively) were enrolled in a treatment program at 12-month follow-up (
Table 1). Over the 12-month follow-up period, 202 persons with PTSD (98 percent) and 279 (97 percent) without PTSD had entered formal treatment for their heroin dependence (inclusive of their current treatment episode) (
Table 1). Persons with and without PTSD were equally as likely to have entered methadone maintenance, buprenorphine maintenance, detoxification, residential rehabilitation, rapid opioid detoxification, or naltrexone maintenance. However, persons with PTSD were more likely to have undergone outpatient counseling for their heroin dependence (OR=1.64, CI=1.10 to 2.67). Although persons with PTSD underwent a greater number of treatment episodes compared with those without PTSD (t=-2.22, df=493, p<.05), the median number of days in treatment over the follow-up period was the same for persons with and without PTSD.
Cost of opiate treatment
The total cost of opiate treatment over the 12-month follow-up period for individuals with and without PTSD was $1,111,118 and $1,393,181, respectively, for an average of $5,394±$5,136 (median=$3,881) per person with PTSD compared with $4,821±$5,144 (median=$3,431) per person without PTSD (
Table 1). However, the difference in costs between the two groups was not significant (cost ratio=1.52, 95 percent CI=.48 to 4.76).
Treatment outcomes
Occupational functioning. The proportion of study participants with PTSD who endorsed employment as their main source of income increased significantly between baseline and the 12-month follow-up (β=.54, CI=.01 to 1.08) (
Table 2). Nonetheless, persons with PTSD were less likely to endorse employment as their main source of income at both baseline and follow-up (β=-.94, CI=-1.41 to -.46). No change was noted in the proportion of participants who endorsed employment as their main source of income among those who did not have PTSD.
Heroin use and other drug use. Study participants with and without PTSD demonstrated significant improvements in their drug use from baseline to 12-month follow-up (
Table 2). Thirty-one persons with PTSD (15 percent) and 37 (13 percent) without PTSD had been abstinent from heroin for the entire 12-month follow-up period. Although a majority of persons with and without PTSD had used heroin in the month preceding the baseline interview, only 92 (45 percent) and 113 (39 percent) of each group had used it in the month preceding their 12-month follow-up interview (β=-4.41, CI=-5.20 to -3.61). Both groups also exhibited significant reductions in the number of drug classes used in the preceding month (β=-1.53, CI=-1.87 to -1.19). No significant differences were noted in the number of drug classes used between individuals with and without PTSD at baseline or at 12-month follow-up. Individuals with and without PTSD made improvements in the prevalence of 12-month nonfatal overdose (β=-1.27, CI=-1.51 to -1.03). However, individuals with PTSD were more likely to have overdosed in the preceding 12 months at both baseline and follow-up (β=.43, CI=.10 to .77).
General physical and mental health. Significant improvements were demonstrated in the level of general physical health reported by persons with and without PTSD (β=5.38, CI=3.27 to 7.48) (
Table 2). Similar improvements were seen in both groups' general mental health (β=9.77, CI=7.46 to 12.08). However, at baseline and 12-month follow-up the physical and mental health of persons with PTSD was still significantly poorer than that of those without PTSD (physical: β=-3.09, CI=-4.41 to -1.78; mental: β=-4.48, 95 percent CI=-5.96 to -3.01).
Major depression and attempted suicide. Over the 12-month follow-up period the prevalence of major depression decreased among study participants with and without PTSD (β=-1.01, CI=-1.59 to -.43). However, compared with those without PTSD, individuals with PTSD were more likely to have a diagnosis of major depression at baseline and 12 months (β=.85, CI=.52 to 1.19). The proportion of participants who had attempted suicide in the preceding 12 months decreased slightly for both groups from baseline to 12 month follow-up (β=-.72, CI=.33 to -.09). Persons with PTSD were more likely to have attempted suicide in the preceding 12 months at both baseline and 12-month follow-up (β=.61, CI=.20 to 1.02).
Discussion
The findings of this study demonstrate that persons with PTSD have significant contact with opiate treatment services over the course of 12 months. Use of a succession of different treatments and modalities over time is a common finding in the literature (
27,
28) and demonstrates the importance of conducting naturalistic studies. Unlike U.S. studies, our study in Australia showed that individuals with and without PTSD spent a similar amount of time in treatment over the follow-up period. This discrepancy may result from differences in treatment measurement—that is, single versus multiple modalities. However, it is more likely to derive from differences in access to opiate treatment between the two countries, with access being considerably more restrictive in the United States in terms of its cost, number of placements, and attendance requirements (
29). For example, in the United States methadone maintenance treatment is available for approximately 15 percent of individuals with opiate dependence, whereas methadone maintenance is available for approximately 40 percent of Australians with opiate dependence (
30,
31,
32,
33). The finding that individuals with PTSD had enrolled in a significantly greater total number of treatment episodes is of concern, because reduced treatment stability has been associated with poorer treatment outcomes (
27,
34).
Over the 12-month follow-up period, the cost of opiate treatment for persons with PTSD was on average $573 higher than the costs for those with heroin dependence alone (Australian dollars; approximately $292 in U.S. dollars). This difference was not significant and was far smaller than that reported by Brown and colleagues ($3,262, in U.S. dollars) (
11). This nonsignificant finding was surprising given the poorer clinical presentation of persons with comorbid heroin dependence and PTSD (
5). The disparity between Australian and U.S. estimates may be due to differences in health care delivery between the two countries, with health care in Australia being more accessible and considerably less expensive than in the United States (
35). The disparity also highlights the inability of results of cost analyses from either country to be extrapolated to the other.
Alternatively, the method we used to cost resource use in our study may not have been sensitive enough to detect differences between groups. For example, although individuals with PTSD may have been in treatment for the same number of days, they may have received more intensive treatment during that time. Given that this study applied an average unit cost across all participants, such features would not have been captured.
The amount spent on opiate treatment for persons with and without PTSD needs to be considered in the context of these individuals' treatment outcomes. Consistent with previous research (
6,
7,
8), PTSD continued to be associated with poorer occupational functioning, overdose, and poorer physical and mental health at follow-up. Therefore, although persons with PTSD did not pose an increased cost to the health care system, the economic burden of comorbid heroin dependence and PTSD is likely to be much greater given the substantial cost of unemployment and of physical and mental illness to society (
36). Nevertheless, it should be noted that a great deal of improvement was achieved among persons with PTSD for a rather modest investment ($5,394 Australian, $2,751 U.S.) considering the level of disability associated with the disorder.
Conclusions
Although the same amount was invested in opiate treatment for persons with and without PTSD, those with PTSD continued to perform poorly in many domains at follow-up. A well-designed intervention that targets both heroin dependence and PTSD may help improve the outcomes of persons with PTSD. Although implementing such a program in substance abuse treatment settings may be costly, this cost may be offset through a decreased amount of future care required and an increased level of functioning among individuals in society (
12). Future research should examine the cost benefit and cost-effectiveness of combined therapies for comorbid substance use disorders and PTSD.
Acknowledgments
The Australian Treatment Outcome Study (ATOS) was funded by the National Health and Medical Research Council (National Illicit Drugs Strategy) and the Commonwealth Department of Health and Ageing. The authors thank Anna Williamson, B.Sc.(Psych.), Kate Hetherington, B.Sc.(Psych.), Evelyn Wilhelm, B.Sc.(Psych.), Sandra Fairbairn, B.Sc. (Psych.), Alys Havard, B.Sc.(Psych.), and Stuart Gilmour, M.P.H.