Methods
We conducted a retrospective analysis of secondary data for all patients who had been given a diagnosis of bipolar disorder in fiscal year 2001 (October 1, 2000, through September 30, 2001) and had received care at facilities within the VA Stars and Stripes Integrated Services Network. The network includes facilities in Pennsylvania, Delaware, and areas of West Virginia, Ohio, New Jersey, and New York. We identified all patients with either an inpatient or outpatient diagnosis of bipolar disorder (I, II, or not otherwise specified) or cyclothymia from the VA National Patient Care Database by using
ICD-9 codes 296.0x, 296.1x, 296.4x through 296.8x, and 301.13. We limited the sample to patients with either one inpatient or two separate outpatient visits with a recorded diagnosis of bipolar disorder in order to maximize the specificity of diagnoses and limit diagnoses given to rule out a disorder (
6). This study was reviewed and approved by local institutional review boards of the VA Pittsburgh Healthcare System.
Psychopharmacologic prescription data were ascertained from the VA Pharmacy Benefits Management Database from fiscal year 2001. We ascertained whether patients received a prescription from the date of the index bipolar diagnosis up to 12 months after the index diagnosis for at least one medication from each of the following categories: lithium, mood stabilizers other than lithium, first-generation antipsychotics, second-generation antipsychotics, selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, antidepressants other than SSRIs or tricyclics, and benzodiazepines.
Specifically, other mood stabilizers included divalproex, valproate, carbamazepine, and lamotrigine. First-generation antipsychotics included chlorpromazine, fluphenazine, mesoridazine, thiothixene, perphenazine, thioridazine, trifluoperazine, haloperidol, loxapine, and molindone. Second-generation antipsychotics included clozapine, olanzapine, aripiprazole, quetiapine, risperidone, and ziprasidone. SSRIs included fluoxetine, fluvoxamine, paroxetine, sertraline, and citalopram. Tricyclics included ami-triptyline, amitriptyline pamoate, clomi-pramine, desipramine, doxepin, imipramine, nortriptyline, protriptyline, trimipramine, and amoxapine. Other antidepressants included bupropion, venlafaxine, maprotiline, trazodone, mirtazapine, and nefazodone. Benzodiazepines included alprazolam, chlordiazepoxide, clorazepate, diaze-pam, flurazepam, lorazepam, oxaze-pam, temazepam, and triazolam.
We also determined whether the patient received any mood stabilizer, any antipsychotic, or any antidepressant during the 12-month period. Additional demographic and clinical data on patients who were given a diagnosis of bipolar disorder were collected from the VA National Patient Care Database.
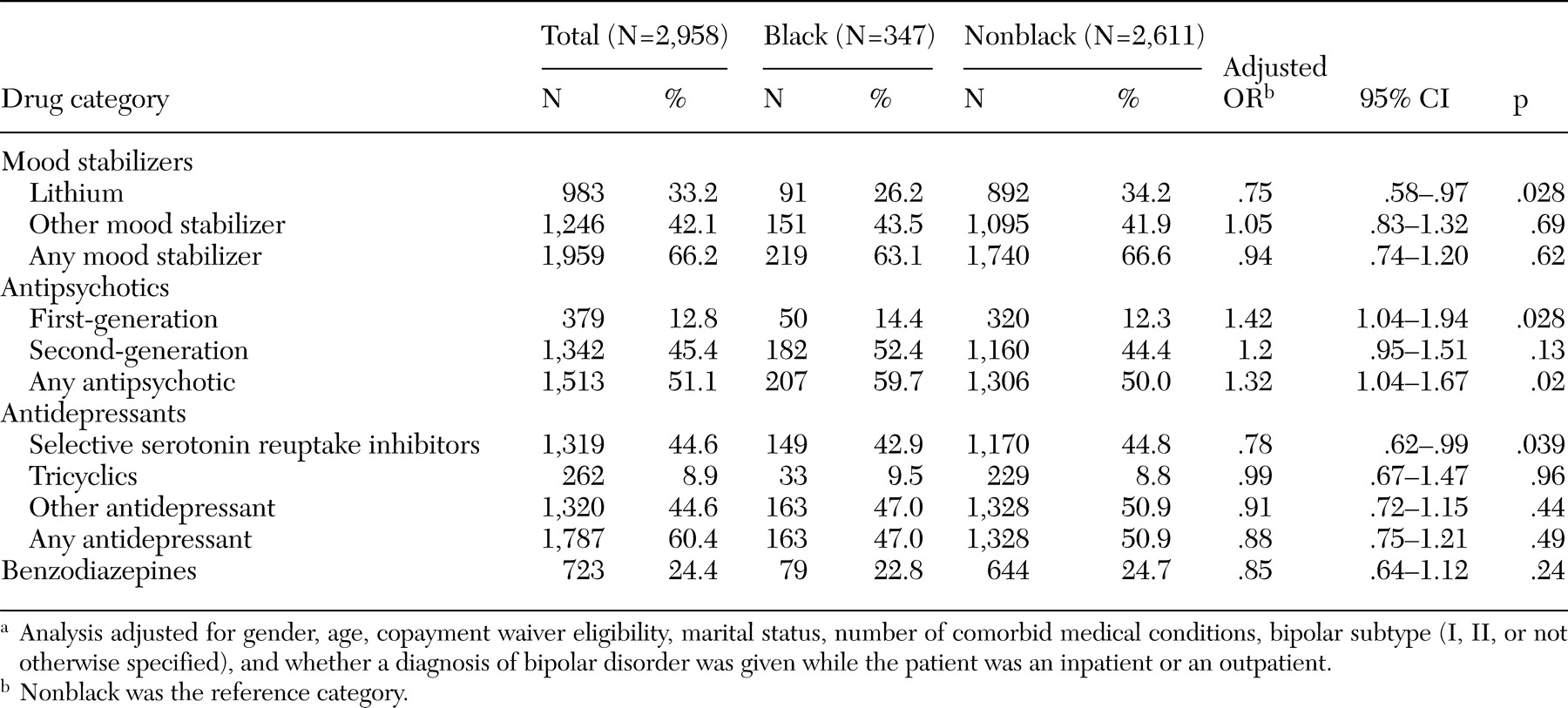
Descriptive statistics were used to estimate the percentage of patients who received at least one medication from each aforementioned drug class. Race was categorized as black or nonblack (defined as white or other race or ethnicity), because relatively few patients (less than 1 percent) were classified as another race or ethnicity. Patients with an unknown race or ethnicity were excluded from the sample (N=368).
We then applied multivariate logistic regression modeling to determine whether differences in the receipt of medication by race remained significant. The analysis controlled for demographic factors, including gender, age, marital status (categorized as married or not married), copayment waiver eligibility, and clinical factors (number of comorbid medical conditions, bipolar subtype, and whether a diagnosis of bipolar disorder was received during an inpatient or outpatient visit). Patients who were eligible for a copayment waiver were considered to have lower income.
The number of medical conditions diagnosed in fiscal year 2001 was based on the clinical classifications of the Agency for Healthcare Research and Quality. Medical conditions included hypertension, congestive heart failure, peripheral vascular disease, stroke, ischemic heart disease, diabetes, hyperlipidemia, pancreatitis, thyroid disorders, obesity, hepatitis C, other hepatitis, lower back pain, arthritis, hip problems, chronic obstructive pulmonary disease, asthma, lung cancer, prostate cancer, skin cancer, spinal cord injury, other accidents or injuries, renal failure, gastric-related disorders, benign prostatic hyperplasia, HIV infection, headache, dementia, Alzheimer's disease, Parkinson's disease, multiple sclerosis, and anemia.
For the multivariate analyses, we conducted sensitivity analyses of pharmacotherapy class categorizations (for example, excluded clozapine) and independent variables (for example, excluded racial and ethnic groups other than black and white). In all cases, similar results were obtained.
Discussion
Overall, 66 percent of patients with a diagnosis of bipolar disorder were given a prescription for any mood stabilizer; 51 percent, any antipsychotic; 60 percent, any antidepressant; and 24 percent, benzodiazepines. After the analysis adjusted for demographic and clinical factors, blacks were more likely than nonblacks to receive first-generation antipsychotics and any antipsychotics. In addition, blacks were less likely than nonblacks to receive lithium and SSRIs.
Our findings on overall mood stabilizer use are similar to previous research among VA patients with a diagnosis of bipolar disorder, which found that among 65,556 veterans, 41 percent were given a prescription for lithium (
7). The racial differences that we observed in our study also reflected trends seen elsewhere. For example, among 13,065 patients who received Medicaid, blacks were less likely than whites to be given a prescription for SSRIs (
4). Also, in a community-based study on 5,032 patient-visits from the National Ambulatory Medical Care Survey, blacks were less likely than whites to be given a prescription for second-generation antipsychotics (
5). However, in our study of patients with bipolar disorder, blacks were no less likely to be prescribed second-generation antipsychotics and were more likely to be prescribed any antipsychotic. Perhaps providers are prone to prescribing antipsychotic medications to black patients because of the perception that black patients are more likely to exhibit psychotic features. Alternatively, in another study of 816 veteran patients, blacks with a diagnosis of bipolar disorder were more likely than whites to receive a concurrent diagnosis of schizophrenia and hence may be more likely to receive antipsychotics (
8).
Our results suggest that a substantial proportion of patients with bipolar disorder are receiving other psychotropic medications along with first-line mood stabilizers, such as antipsychotics, antidepressants, and benzodiazepines. The recent concerns about the safety and toxicity of these commonly used psychotropic medications, such as the increased risk of diabetes associated with antipsychotic medications (
9) and the possible link between SSRI use and suicidal ideation (
10), suggest that careful monitoring of the long-term health risks of psychotropic medication use among patients with bipolar disorder is warranted.
Still, we found that blacks were less likely than nonblacks to be given a prescription for lithium, a medication with substantial research evidence for effectiveness in bipolar disorder that also carries a greater risk of side effects than other mood stabilizers. Blacks were also less likely than nonblacks to receive a prescription for SSRIs, reflecting similar findings (
3). In contrast, blacks were more likely than nonblacks to receive a prescription for first-generation antipsychotics, which may also potentially have more extrapyramidal side effects than second-generation antipsychotics. Several reasons for these findings can be proposed. For example, black patients may be more susceptible to the side effects associated with lithium (
11) and SSRIs and hence may prefer other medications. In contrast, determinants of racial differences in second-generation antipsychotic use are less clear. Perhaps providers are less willing to switch black patients to second-generation antipsychotics because of perceptions that blacks are less likely to comply with these more expensive medications because of co-occurring substance use (
5) or because the providers perceive that the increased risk of metabolic syndromes possibly associated with these medications (
9) may disproportionately affect blacks.
Potential limitations of this study include the use of administrative data rather than more formalized diagnostic procedures to identify patients with bipolar disorder, even though we took steps to eliminate diagnoses given to rule out a disorder. In addition, our sample was primarily male, reflecting the VA population. However, a majority of patients with bipolar disorder receive care from publicly funded providers (for example, VA and Medicaid); hence our sample may reflect an indigent population seen within other publicly funded treatment settings.