Much variation appears to exist in physicians' prescribing patterns for a wide range of clinical conditions (
1,
2,
3). Existing research indicates that some physicians are more inclined than others to follow the best available evidence (
1). However, the characteristics of such physicians are not well understood.
The purpose of the study reported here was to identify relationships between psychiatrists' characteristics and their self-reported adherence to evidence-based recommendations regarding antipsychotic use for patients with schizophrenia. Many recent studies of physicians' prescribing practices have used medical charts, insurance claims, or prescription drug records as key data sources. However, such data sources are often incomplete or are inaccurate in terms of patients' medication history and are expensive to use (
4,
5). Thus our study used self-reported information, which is a relatively inexpensive data source for investigating determinants of physicians' adherence to evidence-based prescribing practices. We used the PRECEDE model (Predisposing, Reinforcing, and Enabling Causes in Educational Diagnosis and Evaluation) (
1,
6) as a conceptual framework for selecting psychiatrists' characteristics as predictors of adherence.
Methods
We focused on two prescribing practices that had been presented in previous studies and policy statements as reflecting the best available evidence (
7,
8,
9). The first of these was prescribing antipsychotics within the dosage ranges recommended by such groups as the American Psychiatric Association and the Schizophrenia Patient Outcomes Research Team (PORT). The second was prescribing second-generation antipsychotics before first-generation agents for patients experiencing a first episode of schizophrenia or for patients for whom there is no available history concerning response to antipsychotics.
The study population consisted of psychiatrists who were affiliated with the Veterans Health Administration of the Department of Veterans Affairs (VA). The VA system provides care to approximately 100,000 patients each year who have been given a diagnosis of schizophrenia. To identify psychiatrists for the study sample, we obtained a data file of all psychiatrists who devoted at least one-eighth of their professional time to the VA system. The total number of psychiatrists in the study population was 1,757. Identifiers were used only for the purposes of tracking nonresponse.
To obtain information about adherence, the study questionnaire asked respondents to estimate from among predefined ranges (between 100 and 95 percent, between 94 and 85 percent, between 84 and 75 percent, and so on) the proportion of their eligible patients for whom they followed each of the two prescribing practices. The questionnaire also asked respondents to report—again, in accordance with predefined ranges or categories—their demographic characteristics, education and training, and clinical and academic arrangements. In addition, respondents were asked to indicate along 4-point scales the extent to which they used different sources of information for staying current with scientific developments in psychopharmacology. The survey was conducted between June and August of 2003. We secured approval for the study from a VA institutional review board.
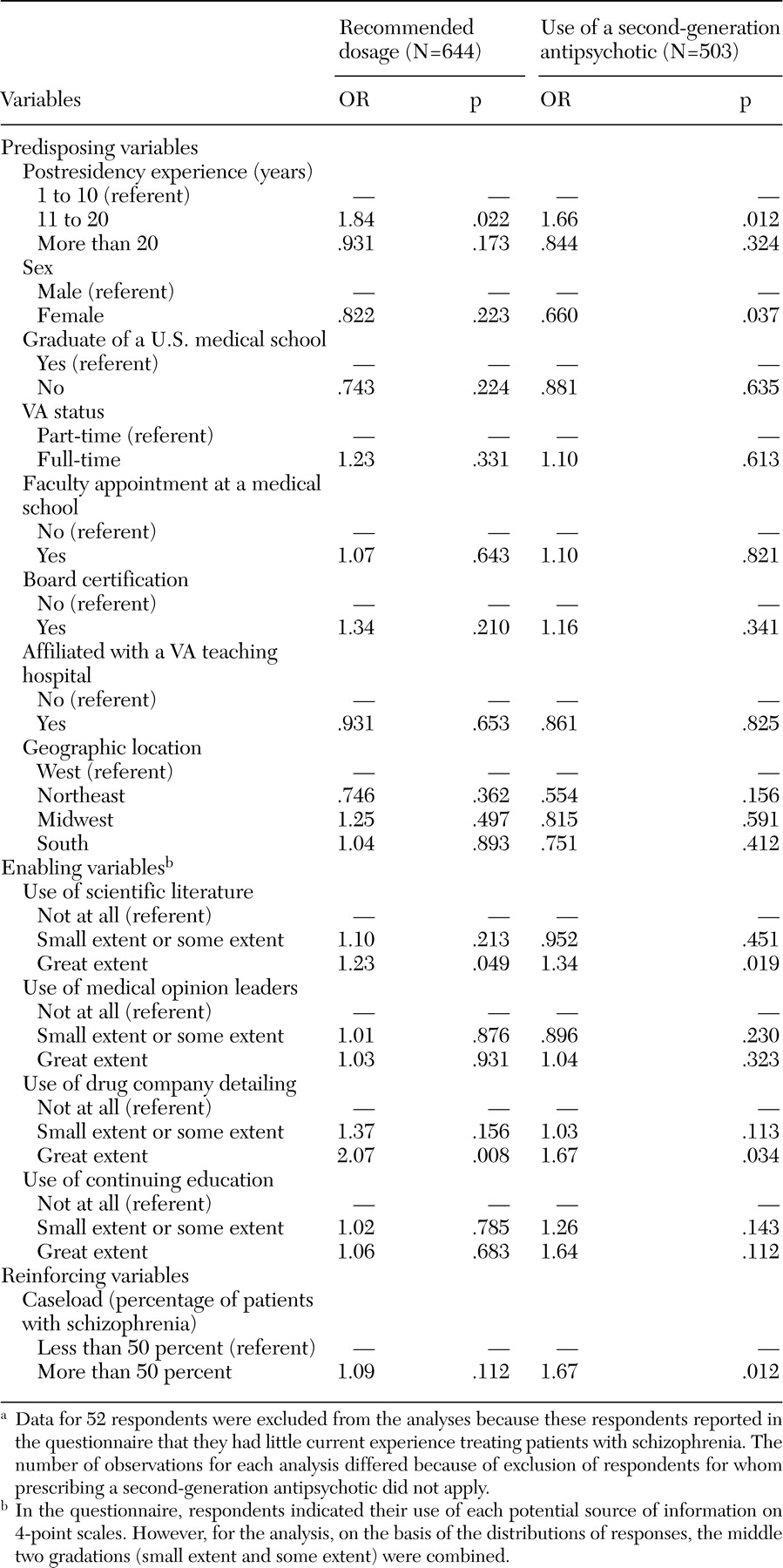
For the purposes of the study, we specified adherence as a dichotomous variable: whether or not the psychiatrist reported following the practice for at least 75 percent of his or her patients who were eligible for the practice. We chose the 75 percent threshold, after discussions with experts in the field, because it recognizes the need for some degree of deviation from each prescribing practice to account for individual patient characteristics but also acknowledges the growing consensus that these practices should apply in the vast majority of cases. We used other data from the survey to assess physician-level characteristics that were classified as predisposing, enabling, or reinforcing variables in reference to the PRECEDE model (
Table 1).
To identify psychiatrists' characteristics associated with adherence, we estimated a regression model that included adherence as a dependent variable and physician-level characteristics as independent variables. Two separate models were estimated, one for each of the two prescribing practices. We used random-effects regression models that accounted for the nesting of psychiatrists who were on staff at the same VA hospital and thus did not represent entirely independent observations.
Results
The survey response rate was approximately 40 percent (696 responses out of 1,757 psychiatrists surveyed). To assess response bias, we compared respondents with nonrespondents in terms of sex, age, duration of VA affiliation, practice setting (teaching or nonteaching), and medical school (non-U.S. or U.S.). Only one significant difference was observed: respondents were somewhat more likely to be women (p<.05). In addition, response rates by hospital and by geographic region were comparable across the VA system.
Among the psychiatrists in the sample, approximately two-thirds had more than ten years of postresidency experience (471 psychiatrists, or 68 percent), and almost one-third (228 psychiatrists, or 33 percent) had graduated from medical schools outside the United States. Almost 28 percent (192 psychiatrists) were women. Approximately 25 percent of the psychiatrists (N=175) were less than full-time VA employees and thus were likely to be seeing some of their patients in clinical settings outside the VA system. A majority of psychiatrists in the study sample had some connection to academic medicine through either a faculty appointment at a medical school or an affiliation with a VA teaching hospital (364 psychiatrists, or 52 percent). Approximately one-third of the psychiatrists (N=323, or 32 percent) were located in the South, with the remainder appearing in roughly equal numbers the Northeast (N=146, or 21 percent), the West (N=161, or 23 percent), and the Midwest (N=166, or 24 percent). Approximately 20 percent of the psychiatrists (N=134) reported that patients with schizophrenia accounted for more than half their caseload.
For the sample as a whole, the self-reported rate of adherence to practice recommendations, as previously defined, was approximately 81 percent (564 psychiatrists) for dosage and 78.5 percent (395 psychiatrists) for use of a second-generation antipsychotic. Odds ratios from the regression analyses are reported in
Table 1. Variables pertaining to postresidency experience, respondents' sex, use of scientific literature, use of drug company reports, and caseload were statistically significant (p<.05) in either one or both models.
Discussion and conclusions
A combination of variables appears to be associated with adherence. In terms of predisposing factors, a somewhat curvilinear pattern was observed for postresidency experience—self-reported adherence was highest for psychiatrists who were in midcareer compared with those who were more junior or more senior. These physicians may be at an optimal point in their careers in terms of both motivation and resources for staying current with recommended prescribing practices. In addition, we observed lower levels of self-reported adherence for female psychiatrists for one of the two prescribing practices. Previous research has also pointed to prescribing differences between male and female physicians, indicating, in particular, that female physicians are less inclined to prescribe new drugs (
1).
Our results also point to the role of information sources in enabling psychiatrists to adhere to evidence-based practices. Although some physicians may be more predisposed than others to search for information about best practices, our results suggest that relatively greater use of information that is available from published scientific literature and from drug company detailing promotes adherence. Finally, specialization may help reinforce adherence to evidence-based practices, given that self-reported adherence was higher for psychiatrists whose caseloads consisted of a relatively large proportion (more than 50 percent) of patients with schizophrenia.
The study's major limitation is that its results are based on self-reported data, which are potentially subject to both recall bias and social desirability bias. The 40 percent response rate is another limitation, although our comparison of respondents and nonrespondents did not suggest any substantial source of bias.
In sum, we identified several physician-level characteristics that may affect adherence to evidence-based prescribing practices. Additional research is necessary to determine the generalizability of these findings and to better understand the mechanisms underlying these relationships.
Acknowledgments
Financial support for this study was provided by the Health Services Research and Development Service of the Department of Veterans Affairs.