Research shows that compared with persons with different types of general medical disorders, those with mental disorders have the strongest stigma rankings, lowest employability rankings, and largest productivity-adjusted wage differentials (
1). Evidence on employer hiring practices is consistent: among the 117 businesses interviewed in a recent survey, 68 percent made an effort to hire persons from minority groups and 41 percent made an effort to hire persons with general medical disorders but only 33 percent made an effort to hire persons with mental disorders (
2).
A central stereotype about persons with mental illness is the belief that because of the symptoms and functional limitations associated with their illness, they are less capable members of the workforce. Even though new treatments are available that effectively control symptoms for many persons, employers with this view are potentially less likely to reward workers with mental illness because of the biased belief that the workers' productivity is limited (
3,
4,
5). Still, despite such stigma, thousands of persons with serious mental illness are working in the competitive workforce, but they receive some of the lowest productivity-adjusted wages (
1). The relationship between the low wages and potential discriminatory behavior on the part of their employers is unknown.
Economists have developed techniques to quantify the relative contribution of stigma in determining wages for minority groups. By applying these methods to persons with serious mental illness, recent research has shown that the functional limitations associated with mental disorders explain only part of the differences in mean wages between persons with mental disorders and those without such disorders (unpublished manuscript, Baldwin ML, Marcus SC, 2005). Because the largest unexplained wage differences were noted for persons with psychotic disorders, the subgroup of mental illness arguably subject to the strongest stigma, it is possible that a large portion of the unexplained differences may be attributed to stigma and discrimination.
What is lacking in the research is evidence of an association between stigmatizing treatment in the labor market and econometric measures of wage discrimination. To address this gap, we used data from a large, nationally representative sample to compare productivity-adjusted wage rates for workers with serious mental illness who reported that they had experienced stigma at work and those who had not experienced such stigma.
Methods
Data
Data were from the 1994-1995 National Health Interview Survey—Disability Supplement (NHIS-D). The NHIS-D was administered in two phases. The primary screening question asked individuals whether they were currently "unable or limited in ability to participate in a major activity, including work and household responsibilities." Each respondent who answered yes was asked to identify up to two contributory conditions, which were subsequently coded by using
ICD-9 criteria. Using the
ICD-9 codes, we identified persons who had the following serious mental illnesses: mood disorders (
ICD-9 codes 296, 300.4, and 311), psychotic disorders (
ICD-9 codes 295, 297-299, and 780.1), and anxiety disorders (
ICD-9 code 300). Multiple
ICD-9 codes are possible, so some persons with serious mental illness were included in more than one diagnostic subgroup. Self-reports are not as ideal as physicians' diagnoses for defining study groups, but Spitzer and colleagues (
6) showed exceedingly high correspondence between self-reported mental health symptoms and physicians' diagnoses in a large clinical sample.
We restricted the sample to persons aged 18 to 65 years who worked during the month preceding the interview. Our study groups included 1,139 workers with a serious mental illness and a comparison group of 66,341 workers with no reported limitations in major life activities. We selected this "pure" comparison group to ensure that these participants were not subject to any disability-related discrimination. In the sample, 30,964 (46 percent) were female and 55,089 (82 percent) were white. A total of 10,473 participants (16 percent) were aged 18 to 24 years, and 38,621 (57 percent) were aged 25 to 44 years. Among those with serious mental illness, 914 persons had a mood disorder, 86 had a psychotic disorder, and 703 had an anxiety disorder.
Questions on the work history section of the NHIS-D asked persons who were currently working and reported that a chronic health condition limited the kind or amount of work they could do whether in the past five years, because of the condition, they had been refused employment, a promotion, a transfer, or access to training programs. Additionally, persons were asked whether the condition made it difficult to change jobs, made it difficult to advance in their current job, or ever caused them to lose a job. For analysis, we disaggregated workers with serious mental illness into two groups, according to whether they reported any of these experiences of job-related stigma.
Analyses
Econometric estimates of stigma were computed by using multivariate ordinary least squares regressions with the natural log of the hourly wage rate of each worker as the dependent variable and mental illness status as the primary independent variable, controlling for worker productivity and other worker characteristics. Separate models were run for each diagnosis (mood, psychotic, and anxiety disorders and all mental health disorders) for each stigma-reporting group, with workers without mental illness used as the reference. The coefficient of the mental illness variable in each wage model represents the effect of stigma against workers with mental illness. Taking the exponential of this coefficient, the transformed coefficient can be interpreted as the ratio of mean productivity-adjusted wages for workers with serious mental illness relative to workers with no mental illness. We hypothesized that the productivity-adjusted wage ratios would be significantly smaller (that is, lower mean adjusted wages) for workers who reported stigmatizing experiences compared with those who did not.
The rich set of control variables available on the NHIS-D is an important advantage of the study. The regression models included productivity-related characteristics of workers with and without mental illness, including differences in human capital investments, job characteristics, and functional limitations. We controlled for human capital investments in education (years of schooling), work experience (years of experience in the current job and age, as a proxy for potential work experience outside the current job), and health (whether the worker had a comorbid chronic physical disability or substance use disorder). Measures of job characteristics described the industrial and occupational classifications of the worker's current job. Measures of functional limitations identified workers who needed help with activities of daily living (including bathing, dressing, eating, and getting in and out of bed); instrumental activities of daily living (including preparing meals, shopping, managing money, using the telephone, and cleaning); or who had social or cognitive limitations (had a lot of trouble making or keeping friendships, getting along in a social setting, or concentrating long enough to complete tasks or were frequently confused, disoriented, or forgetful). The models also controlled for workers' race and gender.
All analyses were conducted with SUDAAN to account for the complex sample design and weighting of the NHIS-D (
7).
Results
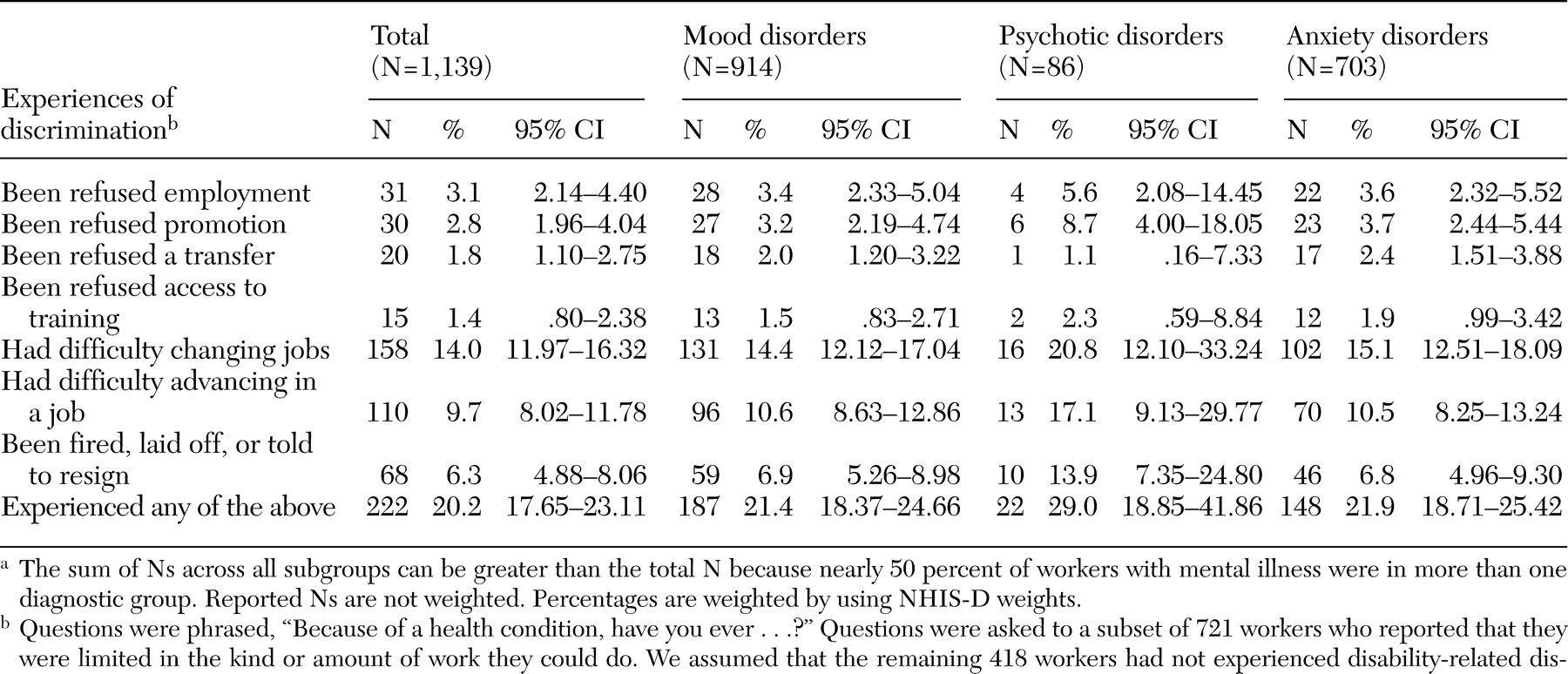
Table 1 shows the weighted percentage of workers with serious mental illness who reported various types of job-related stigma attributed to their illness. Overall, 222 workers with mental illness (20 percent) reported that they had experienced some type of job-related stigma. Among the workers with mental illness, 31 (3.1 percent) reported being refused employment, 30 (2.8 percent) reported being refused a promotion, 20 (1.8 percent) reported being refused a transfer, and 15 (1.4 percent) reported being refused access to job training. Additionally, 158 (14.0 percent) had difficulty changing jobs, 110 (9.7 percent) had difficulty advancing in a job, and 68 (6.3 percent) had been fired, laid off, or told to resign from a job. Overall, workers with psychotic disorders were more likely to report experiences of job-related stigma (22 workers, or 29 percent) than workers with either mood disorders (187 workers, or 21 percent) or anxiety disorders (148 workers, or 22 percent), but these differences were not statistically significant.
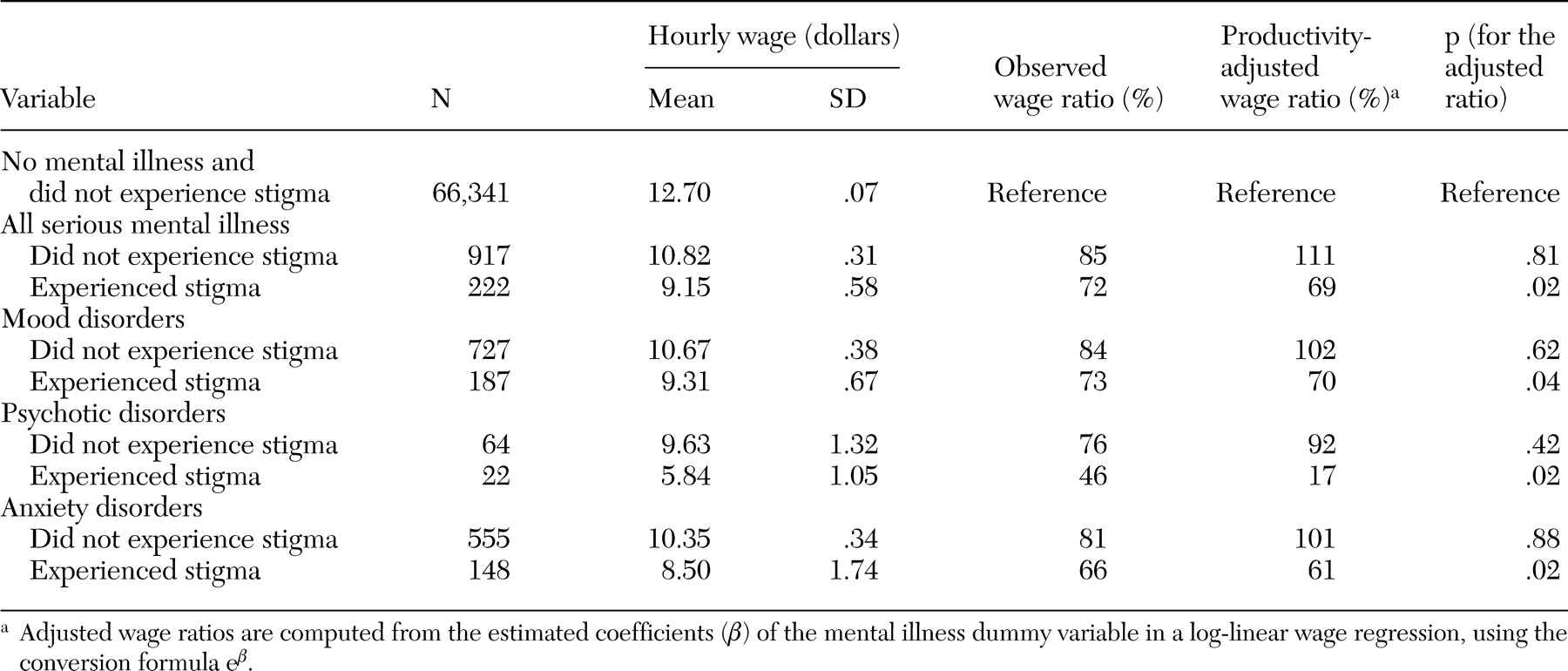
Table 2 presents ratios of mean wages (observed wage ratios) for workers with mental illness (both those who reported and those who did not report stigmatizing experiences in the workplace) relative to those with no mental illness. Among workers with serious mental illness, those who did not report experiencing stigma had an observed wage ratio of 85 percent and those who reported experiencing stigma had a ratio of 72 percent. Similarly, among workers with mood disorders, the observed wage ratio was 84 percent for those who did not report experiencing stigma and 73 percent for those who did. Among workers with anxiety disorders, the wage ratios are 81 percent for those who did not report experiencing stigma and 66 percent for those who did. The lowest wage ratios, by far, were observed for workers with psychotic disorders: 76 percent for those who did not report experiencing stigma and 46 percent for those who did.
The wage differences surely reflect, at least in part, productivity-related differences between the study groups and controls. Fortunately, our data set contains an extensive array of variables that allowed us to examine and subsequently control for these differences. Most important of these is likely the association between mental disorders and deficits in the higher-order social and cognitive skills that are particularly important for success in the workplace (
8).
Workers with serious mental illness were more likely than those with no mental illness to report all types of functional limitations (results not shown). Among workers with mental illness, those who reported stigmatizing experiences were more likely to report functional limitations than those who did not experience stigma. For example, only 169 workers with no mental illness (.3 percent) reported that they were frequently confused, disoriented, or forgetful, compared with 162 workers with mental illness who did not report experiencing stigma (18 percent) and 74 workers who reported experiencing stigma (33 percent). Persons with psychotic disorders reported the highest rates of functional limitations across most categories of limitations, reflecting the relatively severe nature of the disorders and the disabling effects of common symptoms.
The wage differentials between workers with mental illness and those with no mental illness, and between workers with mental illness who reported experiencing stigma and those who did not, can also be partly explained by characteristics of the groups with mental illness and their jobs, which are associated with lower wages. For example, in our sample workers with serious mental illness were more likely than those with no mental illness to be female, to work in a service industry, and to work in service occupations. Workers with mental illness who reported experiencing stigma had higher rates of comorbid physical disorders than those with mental illness who did not report experiencing stigma.
Table 2 also reports productivity-adjusted wage ratios, estimated from the coefficient of the mental illness dummy variable in wage regressions that controlled for differences in human capital investments, job characteristics, and functional limitations. As shown in
Table 2, workers with serious mental illness who did not report stigmatizing experiences in the labor market did not have any significant adjusted wage differential associated with mental illness. The adjusted wage ratio was close to one, and the underlying regression coefficient was not significantly different from zero (p=.81). In other words, the observed wage difference between workers with mental illness who did not report stigmatizing experiences and workers with no mental illness is entirely explained by differences in functional limitations and other characteristics. In contrast, the adjusted wage ratio comparing workers with mental illness who reported stigmatizing experiences with those with no mental illness is 69 percent, a result that is large and significant (t=-2.31, df=373, p=.02). The results imply that the wage difference between workers with mental illness who report stigmatizing experiences and workers with no mental illness cannot be explained by differences in functional limitations and other measured productivity-related characteristics. Hence, the econometric measure of stigma is consistent with workers' self-reports of their experiences in the labor market.
Turning to the productivity-adjusted wage ratios for different diagnoses of mental illness, the results are uniformly consistent with the results for serious mental illness overall, although the magnitudes of the ratios vary across subgroups (
Table 2). Within each diagnostic category, the adjusted wage ratio is close to one, and the underlying coefficient of the mental illness dummy variable is insignificant when workers who did not report stigmatizing experiences were compared with those with no mental illness. However, the productivity-adjusted wage ratios are less than one and the underlying coefficients are significant (p<.05) when the group that reported stigmatizing experiences was compared with the control group. The adjusted wage ratio was smallest (17 percent) for workers with psychotic disorders who reported stigmatizing experiences, suggesting that stigma may be an important factor contributing to their significantly lower wages.
Our diagnostic groups contained persons with multiple mental disorders, which could potentially bias the estimated discrimination coefficients. To test the sensitivity of our results to the inclusion of multiple disorders, we reran the multivariate models, controlling for all diagnoses, and found no substantive differences in either the magnitude or direction of our findings.
Discussion
Our results indicate that workers' self-reports of stigmatizing experiences in the labor market are consistent with econometric measures of the effect of stigma on wages. After comparing workers with serious mental illness who did not report experiencing stigma with workers with no mental illness, we found no significant between-group differences in adjusted wages (the analyses controlled for functional limitations and other productivity-related characteristics). However, when we compared workers who reported experiencing stigma with those with no mental illness, the results showed adjusted wages that were about two-thirds as large. The results strongly suggest that workers know when they are being discriminated against.
What is less clear is why some workers with serious mental illness experienced stigma in the labor market while others did not. Our descriptive results suggest some hypotheses. Workers who reported experiencing stigma also reported higher rates of functional limitations compared with those who did not. Because workers with mental illness are often reluctant to disclose their diagnoses in the workplace, the presence of functional limitations may make mental illness more visible to employers and coworkers. In other words, employers may not know about a mental disorder unless there are observable signs, such as functional limitations. Clearly, employers cannot discriminate against a person with mental illness if they are unaware of the illness, so the presence of functional limitations may be a trigger for discrimination.
On the other hand, some persons with serious mental illness may have highly visible impairments that trigger stigma but are not associated with any loss of functional capacity. For example, tardive dyskinesia, an uncontrollable tic or twitching of the facial muscles, is a common side effect of some first-generation antipsychotics. Although the tic is annoying and acts as a negative label, a person with this condition may have no functional limitations if the symptoms of mental illness are controlled effectively with medication. If he or she is subject to stigma that affects wages, the effects will be detected as unexplained wage differentials in the econometric measures of discrimination.
Although we found more people with serious mental illness working than one might expect, and relatively small wage differentials between persons with and without mental illness, we may be observing a selected sample of persons with mental illness who have above-average functional capacities. Once in the labor market these persons do fairly well, within the occupations and industries where they have obtained jobs. The importance of functional capacities is further supported by the gradations we were able to observe across diagnostic categories. The most severely disabled group (as measured by reported functional limitations) was persons with psychotic disorders, who were both less likely to work in white-collar jobs and subject to the largest wage differences. As possible supporting evidence, Hallock and colleagues (
9) did not find a strong association between worker perceptions of disability-related discrimination and econometric measures in a sample of workers with disabilities drawn from graduates of a major mid-Western university.
The research has some important limitations. A worker's self-report of experiencing stigma may be exaggerated if the worker does not acknowledge the effects of functional limitations associated with mental illness. Econometric measures of discrimination may be biased if the data do not record all relevant functional limitations that affect worker productivity. Although we do not have good measures of productivity in the data, we do have fairly complete measures of the social and cognitive limitations often associated with mental illness, including the ability to concentrate. Our results must be interpreted with the caveats that we assumed that workers' self-reports are accurate and that our controls for functional limitations (and other aspects of worker productivity) were reasonably complete.
Other potential limitations are related to the wording of the stigma questions on the NHIS-D. The questions ask whether respondents have ever experienced stigmatizing behaviors in the workplace because of any health condition. Therefore, we cannot distinguish stigma attributed to mental or physical disorders nor can we be certain that the stigmatizing experiences occurred on the current job. However, when we controlled for comorbid physical conditions among the workers with serious mental illness, the effect of mental illness dominated. We believe that the responses are a reasonable proxy for persons who have had problems with mental illness stigma in the workplace, and we assume that these problems continue in the current job.
Another limitation is the small sample of workers with psychotic disorders, the group subject to the greatest stigma. The small sample reflects both lower prevalence rates and lower employment rates for psychotic disorders relative to other mental disorders. In fact, employment rates for persons with psychotic disorders are so much lower, it is likely that the differentials are, in part, associated with the intense stigma against psychotic disorders. The stigma may translate to discrimination in hiring and firing decisions, which is exactly the point of this study.
Conclusions
Even after passage of the Americans With Disabilities Act of 1990, negative attitudes toward persons with mental illness have changed little over the past three decades (
10,
11,
12). According to the President's New Freedom Commission on Mental Health, workplace stigma is an important contributing factor in the underemployment of many persons with mental illness (
13). Our research, showing a strong relationship between workers' self-reports of experiencing stigma in the workplace and economic estimates of wage discrimination, establishes an important link between stigmatizing attitudes and low wages.
We hope that this research will eventually lead to interventions that can reduce stigma against persons with mental illness in the competitive workplace. Effective interventions are likely to be different from the interventions common in supported employment programs (for example, job coaches), because the populations are different. As our study shows, many persons with serious mental illness are capable of working independently in the competitive labor market, although they may have functional limitations associated with their mental disorders. For this group, the problem is not the workers but their work environment. The interventions called for to combat the stigma of mental illness in competitive jobs involve, for example, educating employers, changing employment policies, providing sensitivity awareness training for supervisors and coworkers, and instituting employment practices that tolerate diversity. The interventions must bring about fundamental changes in the workplace culture, with the objective of providing fairer treatment for persons with mental illness in the workplace.
Acknowledgment
This research was supported by grant RO3-MH-067087-01 from the National Institute of Mental Health.