Transference interpretation (TI) has traditionally been considered key to stable change in psychotherapy (
1–
4). In both traditional psychoanalysis and psychodynamic psychotherapy, emphasis has been placed on the change-inducing effect of analysis of the current relationship to the therapist (
5,
6). As described by Strachey (
7) in his classic article on mutative interpretation, patients’ problems play out in the therapy situation. Reactions based on experience with parents and important others gradually develop toward the therapist. How they are met in the present is considered to be of crucial significance. Strachey explained how transference must gradually be interpreted so that patients can become aware of the contrast between their feelings and the real nature of the therapist.
Use or nonuse of TI and its effect on outcome was the focus of a randomized clinical trial using a dismantling design, the First Experimental Study of Transference Interpretation (FEST;
8). The group who received TI and the group who did not improved equally. However, the study found that within the subgroup of women with poor object relations (N=22), the specific effect of transference work was large (
9). In the transference group (N=11), 55% of the patients recovered, whereas in the comparison group (N=11), none recovered. TI obviously has strong potential to improve outcome in this subgroup, but still 45% did not recover. Marble et al. (
10) found that patients with low pretreatment motivation who received TI experienced deterioration of their ability to self-protect, which may be a partial explanation for why some people did not recover. In the current study, to investigate differences between recovery and nonrecovery, we selected two patients; both were women with poor object relations who received TI. At three-year follow-up, one had achieved clinically significant change (recovery) on all outcome measures; the other was somewhat improved but had not recovered on any outcome variable.
Both patients were given TI by the same male therapist. In addition to having poor quality of object relations, both women had obsessive-compulsive personality disorder, mixed anxiety, and depression. However, additional factors distinguished them and are described in greater detail in the “Patients” section.
The differences between them likely contributed to their differences in communication style—direct and open versus scattered and evasive. Their different communication styles and the therapist’s response to them may have been central to their different outcomes. For example, Henry et al. (
11) found that low-change (poorer outcome on Structural Analysis of Social Behavior [SASB] Intrex) patients were less disclosing and more deferential than high-change (better outcome on SASB Intrex) patients. Communication problems have been emphasized by Kiesler (
12), who stated that patients’ ingrained pattern of communication and the way the therapist responds to it is key to outcome. Caston (
13) suggested something similar, describing the patient’s unconscious plan to overcome difficulties and need for the therapist’s help to disconfirm pathogenic beliefs that are played out in therapy rather than respond to them as did the original caregivers.
Many others have emphasized the quality of therapist-patient interaction. Svartberg and Stiles (
14) found that a friendly, noncontrolling focus on the patient by both patient and therapist was a better predictor of outcome than therapist competence. Maintaining and exploring the relationship are primary, according to Henry et al. (
11), who found that in high-change cases, based on the self-reported amount and direction of change on SASB Intrex, both patient and therapist focused on the patient in a friendly and noncontrolling way. High-change patients had therapists who were more helping and affirming than the therapists of low-change patients. Therapists of low-change patients were also significantly more blaming than therapists of high-change patients. Najavits and Strupp (
15) also found that effective therapists receive more affiliative codings from raters. Closely related to communication is the therapist’s countertransference (CT). The concept of CT was originally defined by Freud (
16), who considered it to be a limitation of the therapist—negative reactions to the patient that should not occur. Others, for example object relations theorists such as Heimann (
17), expanded the definition to include all of the therapist’s reactions, positive and negative, conscious and unconscious. Heimann pointed out that therapist responses could be used to better understand patients’ feelings and unconscious mental life. Ogden (
18) has described in depth a special form of CT related to projective identification, a defense mechanism that can produce dramatic emotions in the therapist that seemingly have no reasonable explanation. He described in detail how unacceptable feelings can be forced into another person who may then either process them and make them acceptable or not tolerate them and act them out in some way. Therapist understanding of CT in general, and his or her own specific tendencies in particular, are essential to create an optimal therapy experience for the patient. Dahl et al. (
19) found that therapists’ positive CT in the form of feeling confident was significantly correlated with patients’ experience of being helped and understood. Therapists’ feelings of inadequacy in the CT were negatively correlated with patients’ experience of being helped and understood.
Another factor that has traditionally been considered central to positive change throughout the history of psychoanalysis (
20) is insight, that is, increased understanding of the self, behavioral patterns, and motivations. According to psychoanalytic theory, interpretation of transference may increase insight, which may in turn lead to better interpersonal functioning (
7,
21–
23). Insight gained through the therapist’s interpretation of transference may contribute to integration of intellectual and emotional self-understanding (
7,
23,
24). Johansson et al. (
25) reported that insight developed during the course of therapy was a mediator of the specific long-term effect of TI among patients with low quality of object relations. Insight increased dramatically during treatment when patients received TI, but less so during treatment without TI.
Finally, the mental image (introject) of the therapist after therapy is thought to be a factor that maintains change, as when a child learns how to treat the self through interaction with the parents (
26). The introject is thought to be central in recurrent maladaptive relationship patterns; that is, the patient behaves as though others are like the parent, and this behavior elicits the feared behavior. Henry et al. (
27) suggested how the therapist may be cast in the role of the critical parent to confirm the patient’s existing critical introject and may be pulled into a negative pattern with the patient. Von der Lippe et al. (
28) have described a similar interaction.
Research Hypotheses
On the basis of limited empirical literature we have described, we postulated the following contributions to outcome.
Therapist Factors
Therapist affiliation and CT are likely to affect outcome. Higher levels of therapist affiliation and positive CT will produce a better outcome, and lower levels of therapist affiliation and more negative CT will produce a poorer outcome.
Interaction Factors
The quality of collaboration between patient and therapist will affect outcome. Therapist and patient focused on the patient in a friendly, noncontrolling way will produce a better outcome; therapist and patient focused on the patient in a less friendly, less autonomous way will produce a poorer outcome.
Patient Factors
Productive patient participation is likely to be based on high motivation, insight, affiliation with the therapist, and openness and less deference. High levels of these qualities will likely characterize the patient with the best outcome, whereas lower levels of the same factors will characterize the patient with the poorer outcome. The patient’s internal representation of the therapist (introject) will be stronger when the outcome is more favorable.
Methods
The methodology used in the FEST study has been extensively described elsewhere (
8,
29) and is briefly restated here. One hundred patients were randomized to dynamic psychotherapy with or without TI (52 with TI, 48 without TI). They had weekly 45-minute sessions for one year, and all sessions were audiorecorded. The Regional Ethics Committee for health region 1 in Norway approved the study protocol. A treatment manual was used (
30). Manuals in dynamic psychotherapy are manuals of principles rather than step-by-step procedure. Treatment was focused on affects; exploration of warded-off material; current and past relationships; the therapeutic relationship; interpretations of wishes, needs, and motives; and repeatedly working through central themes, as well as the principles outlined by Sifneos (
5) and Malan and Osimo (
31). The Quality of Object Relations Scale (
32,
33) was the preselected primary moderator in the study protocol. This scale measures the patient’s life-long tendency to establish certain kinds of relationships with others, from mature to primitive. Quality of object relations represents a personality style associated with the capacity to establish and maintain a collaborative relationship, for instance with the therapist, based on mutuality and autonomy. A low Quality of Object Relations Scale score (less than 5) indicates a history of less gratifying relationships characterized by a need for dependency or overcontrol.
Outcome Measures
Four outcome measures were used to assess patients before, during, and after therapy: the Psychodynamic Functioning Scales (PFS), the Global Assessment of Functioning (GAF), the Inventory of Interpersonal Problems–Circumplex Version (IIP-C), and the Symptom Checklist–90 (SCL-90).
The PFS (
34–
36) were developed to measure psychological capacities and capture clinician-rated psychodynamic changes and interpersonal functioning over the previous three months. The six scales—Quality of Family Relationships, Quality of Friendships, Quality of Romantic/Sexual Relationships, Tolerance for Affects, Insight, and Problem Solving Capacities—have the same format as the GAF. The GAF (from
DSM-III) is a clinician-rated measure that captures symptoms and functioning. The IIP-C (
37) is a self-report questionnaire that was developed to represent a comprehensive list of interpersonal problems reported by patients who seek outpatient psychotherapy. We chose this instrument because it is well validated and one of the most widely used self-report instruments in psychotherapy research. The SCL-90 (
38) is a well-validated, 90-item self-report measure of psychiatric symptoms and distress. The measure of self-reported symptom distress was the Global Severity Index (GSI) of the SCL-90.
There are no normative data for the PFS and GAF, but a score of 71 or higher on a scale from 1 to 100 is defined in the descriptive levels of the scales as normal functioning. Patients whose scores increase or decrease more than measurement error and cross the cutoff scores into the distribution of nonclinical samples are considered to have changed to a clinically significant degree. To be rated as recovered in this study, the PFS score must increase from ≤70 to ≥71 (at least 4.2 points), and the GAF score must increase from ≤70 to ≥71 (≥5.8 points). The IIP-C score, based on a scale from –3 to 3, must decrease by more than .37 (cutoff .77), and the SCL-90 score must decrease by more than .40 (GSI cutoff .51) (
39).
Therapist, Patient, and Interaction Measures
Some of these measures affect outcome through a moderator effect (influence on the direction or strength of the outcome) or a mediator effect (changes of a patient characteristic during treatment that later account for change in outcome). Some measures simply elucidate process. Transcripts demonstrate what was said in selected sessions that were used to score process. The Feeling Word Checklist (FWC-58;
40) is a registration of the feelings awakened in the therapist during the sessions (i.e., CT). CT is a moderator of outcome (
19). The Therapist Representation Inventory (TRI;
41) is a self-report measure of the patient’s internalized representations of the psychotherapist and the psychotherapeutic relationship. The Motivation Scale (
42) is a clinician-rated measure of the patient based on several of Sifneos’ (
5) criteria for motivation. It consists of four 8-point Osgood scales: an awareness that symptoms are psychological, a desire for self-understanding, a desire for change, and reasonable expectations. Motivation is a moderator of outcome (
10). The PFS Insight subscale is a clinician-rated measure of the patient that emphasizes cognitive and emotional understanding of inner conflicts, personal patterns, and their connection to past experience. It is a mediator of outcome (
25).
Outside raters evaluated both patients and therapist with the SASB (
43–
48), which produces fine-grained analyses of the interaction between patient and therapist when used as a process measure aimed at assessing emotional and unconscious aspects of therapeutic interaction. With the SASB, it is also possible to measure separately the therapist’s affiliation toward and emancipation of the patient as well as the patient’s affiliation toward therapist and experience of autonomy.
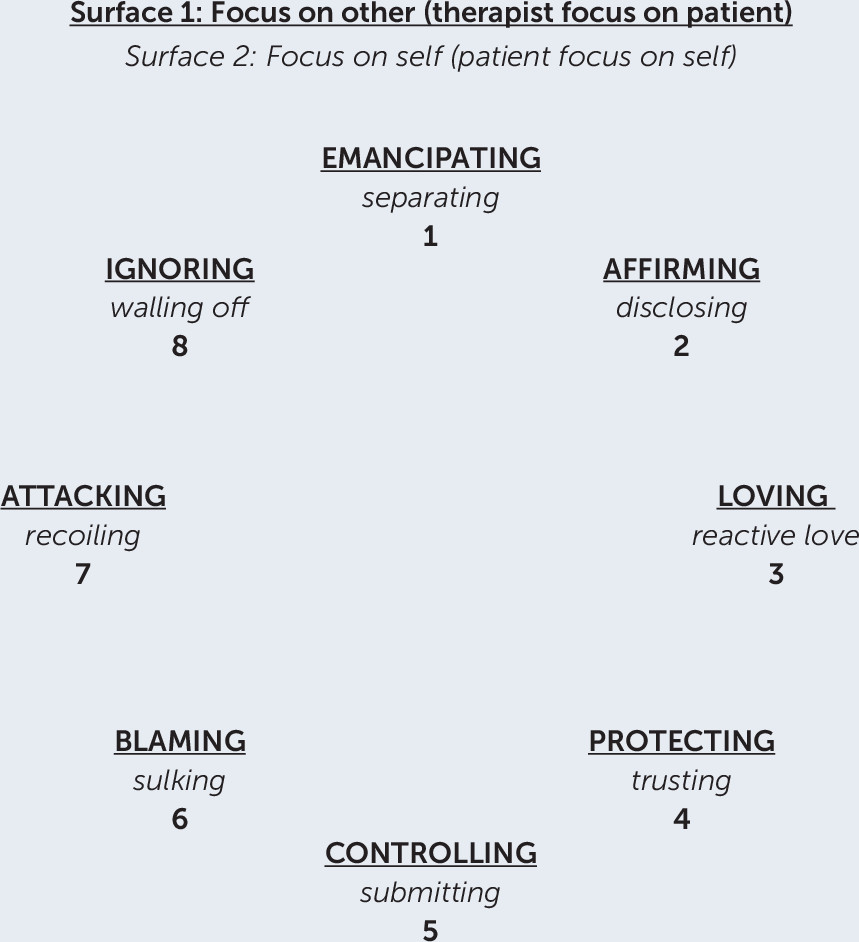
SASB graphs show the degree to which the focus of both therapist and patient was on the patient (complementary interaction). One can also see from the clusters what kind of complementary interaction occurred—for example, patient discloses and therapist affirms (Cluster 2), patient trusts and therapist interprets (Cluster 4), patient submits and therapist controls (Cluster 5)—and how much of each kind of cluster activity occurred in the segment scored (
Figure 1).
Transcripts of all SASB-scored TI and some interchanges without TI from three sessions (early phase, midphase, late phase) illustrate the quality of collaboration, that is, how well the patient-therapist dyad worked toward constructive change.
Frequency of Measurement
SASB.
Three sessions, each representing a phase of treatment, were scored with the SASB: session 7 (beginning of treatment), session 16 (mid-treatment), and a session randomly chosen from the late phase.
Questionnaires.
The FWC-58 was completed after every session. The IIP-C and SCL-90 were administered five times: before therapy, after session 16, at the end of therapy, and at the two follow-up interviews, one year and three years after therapy ended. The PFS and GAF were administered four times: at the start of therapy, at the end of therapy, and at the two follow-up interviews. The TRI was administered three times: after the last session and at the two follow-up interviews.
Patients and Case Formulation
The patients were two women in their late 30s, Anne Solo and Jayne Payne (both pseudonyms). Both women had been educated beyond secondary school. Both had been rated as having obsessive-compulsive personality disorder on the Structured Clinical Interview for DSM Disorders. Both were troubled by pervasive, dysphoric feelings that they attributed to childhood experiences; both were rated low (scores less than five on a scale of 1-8) on the Quality of Object Relations Scale. They were rated as similar on clinician-rated outcome measures, but as different on self-rated outcome measures—Jayne had more symptoms and interpersonal problems than Anne (
Table 1).
Both patients expressed an interest in understanding themselves and a desire to change, which resulted in an PFS Insight score of 62 on a scale from 1 to 100 for both of them. On a scale from 1 to 8, Anne had a high motivation score (6.17), and Jayne had a relatively low motivation score (4.75). A low score (<5) indicates dependency on external help, a desire for magic solutions, or exaggerated pessimism; higher scores are associated with an understanding that change requires active work by the patient. Jayne also had three subthreshold personality disorder scores, and she came from a chaotic family background and had poor, uneducated parents. Anne came from a stable, academic family and had also been in therapy before. Both patients were on sick leave for most of the therapy.
Anne Solo
Background.
Anne Solo was a self-referred, single woman in her late 30s. Her current circumstances were that her mother had died after a long illness. She reexperienced a longing for the mothering she had never received and anger toward her distant mother. Anne was a small, slender, stylishly dressed woman who had a rather masculine, self-contained quality. Her goal for therapy was to be able to express vulnerability and the need for help and understanding. She was ashamed that she could not use her good reasoning skills to get herself to be more confident and express wishes and needs in her relationships.
She felt that the reason for her inability to express her needs was that there was no encouragement in her family to recognize or talk about feelings and that there were too many children close in age for any of them to get much individual attention and nurturing. Achievement was valued above everything else in the family, and parental acceptance was contingent on being clever.
At the time of her initial interview, Anne was about to begin a new, high-level teaching position but said she was worn out from her last job, at which she had some problems with coworkers. Some years earlier, she had one year of group therapy and two years of individual therapy after she had been left by the only man she had been involved with romantically. He had continually doubted his feelings for her and finally left her for someone else.
She had grown up in a large family, the second of six children, with parents who had little time for them. Although she had many positive memories of her parents, she described her father as an idealistic sociologist and Marxist who was focused on the welfare of the masses rather than on the welfare of Anne and his other children. Her mother was completely dedicated to helping him with his many projects and had no energy or possibly no understanding of her children’s emotional needs. All of Anne’s siblings had major emotional problems, and only one had married. While she was growing up, the family had moved every three to five years; she always had trouble finding friends and felt no one wanted to spend time with her if anyone else was available. Her kind but distant parents made her feel emotionally abandoned. She was anorectic for two years in her adolescence.
Case formulation.
Kind but distant and politically dedicated parents indirectly communicated the demand that Anne adapt to their needs, cope well, and not make problems for them. She learned to subordinate her true feelings to the family ideal of being clever and strong. Uncertain of her own worth as friend or marital partner, she was reluctant to show a wish for intimacy and a nurturing relationship and was depressed about what was missing in her life. Anne’s ability to express herself directly in therapy and respond well to the therapist, who was her only close relationship, set the stage for a positive relationship with him.
Jayne Payne
Background.
Jayne Payne was an attractive woman with a flamboyant style of dressing. She was also in her late 30s, had been married for 15 years, and had two children in primary school. She was referred by her general practitioner after a severe panic attack while at work the previous month. Since the attack, she had been constantly anxious and depressed. She was able to care for her children but avoided socializing outside the home and felt unable to return to work and interact with her coworkers because it quickly depleted her. Her family doctor had put her on sick leave. In addition to depression and chronic fatigue, she described a range of symptoms ranging from irritable bowel to insomnia to chronic pain in several organ systems. However, she tried not to dwell on these problems, saw a doctor only three to five times a year, and coped by living a well-regulated life and exercising often.
She primarily wanted help to deal with her anxiety and the increase in pain accompanying it. She felt it was caused by the combined effects of stress at work and at home over time. She felt she was not able to get her needs met, and in her written description of her primary problems she described a sense of “being in a centrifuge all the time.” She wanted to get more control over her life and felt her lack of self-confidence and early life experiences needed to be addressed for change to occur, but she also wrote that she did not want to spend a lot of time in treatment.
She had a good job as a photographer but had become tired of it even before the panic attack occurred, and she remained on sick leave for much of the time she was in therapy. She had no previous psychotherapy as an adult but had been referred for treatment as a child because of obsessive rituals and fainting spells. She could not remember how long this therapy lasted. Her early memories of both parents were primarily negative, particularly those of her abusive, drug-addicted, criminal father. Her mother divorced him when Jayne was a toddler, but he continued to turn up unexpectedly and create turmoil. He did not harm Jayne physically, but he beat her mother, yelled, and smashed things. Whether present or not, he was a terrifying specter for her until his death several years before the therapy began. Her mother used Jayne’s fear of the father’s sudden appearances to make Jayne obey her. It is unclear how often he actually visited them; Jayne’s mother’s frequent threats and her dramatic behavior may have been more difficult for Jayne than her sometimes slapping or spanking Jayne. Her mother’s unpredictable emotions and general inability to nurture Jayne were the major components of Jayne’s everyday life. Jayne felt she constantly had to be hyperalert to what her mother needed and wanted. Currently, she felt tired all the time and told of a need to perform obsessive cleaning rituals and constantly organize at home.
Case formulation.
A chaotic childhood with unpredictable parents who were emotionally and sometimes physically abusive led to an exaggerated need for control. Jayne had no models to identify with or help her learn how to recognize and express feelings. Punishment was extreme, mostly in the form of rejection, shaming, and humiliation, and given on the basis of the mother’s moods rather than Jayne’s behavior. Jayne had to bottle up her feelings or channel them into physical symptoms. Increasing demands of motherhood, work, and married life paired with an inability to recognize or express her needs led to panic and withdrawal from social activity and her job. Jayne’s tendency to fear authority figures and become paralyzed or avoidant when challenged decreased the possibility of a positive relationship with the rigorous therapist.
Therapy Transcripts
Anne Solo
Anne Solo had 36 hours of weekly psychotherapy. All the recorded TIs in the seven-minute SASB-scored segments from sessions 7 (beginning), 16 (middle), and 23 (end) of therapy are included, as well as illustrative extratransference work. Sessions 7 and 16 were chosen because they were preselected points of measurement and represented the beginning and middle of therapy. A third session was randomly chosen from the last phase of therapy.
Session 7.
[Mid-session; the patient has been speaking about her only romantic relationship]
T: What was good and what was bad about the relationship?
P: I liked to talk to him, discuss things, get his viewpoints. The physical relationship was good, but there was a lot I couldn’t say to him and then there was the problem that he didn’t think he had the right feelings for me.
T: Can you say more about the needs you wished he could understand?
P: I wanted him to convince me he cared about me and he was afraid to say anything that would commit him. That and I have always wondered. . . .
P: If we both had the same feelings, if he would have described them in a very different way than I do, if he had more stringent definitions of different feelings. Do you know what I mean?
T: No, not exactly. I do understand that he had reservations that must have hurt you.
P: Yes, of course it did.
Session 16.
[Beginning of session]
P: Last time I got the feeling I often get in other situations, that you felt, as I do, that I just flounder around and bore everyone around me.
T: That I was tired of listening to you talk about “on the one hand, on the other hand.”
P: Yes, then I just want to withdraw
T: It’s not your fault that you flounder.
P: Yes, it is. I generate these feelings, I can’t cope with my reactions in a way that isn’t clumsy.
T: I don’t think clumsy is the right word.
P: I don’t know what the right word is.
T: Your chronic self-doubt can be wearing for those around you.
P: Yes, I know, but. . . .
T: And what lies behind the doubt and what purpose does it serve? I don’t know if we can say we are agreed on that.
[Mid-session]
T: Partly what makes you angry, or maybe not angry but hurt and wanting to withdraw is when I point out some problem you have.
P: Yes, and as I said. . . .
P: You hit the mark, and I feel even more weak.
T: Something you are aware of, so why should I rub it in.
P: Yes, because what I want is to be convinced that it isn’t so awful, cheered on in a way to accept it, deal with it.
Session 23.
Up to this time the patient has had sick leave arranged by the therapist and now feels able to begin work again.
[End of session; the patient dreads the upcoming end of therapy in four months]
T: You are afraid already. You have also said that you think I find you tiresome, but not so much that I can’t stand it.
T: Because you find the thought of the coming separation so painful.
P: Yes, or yes and no, you have helped me with my feelings in a way, I feel you understand because of how you come back to things and how you ask and that you say if you don’t understand, but it’s how I so often experience things, that I don’t have this in daily life, I need to be understood, right? At the same time, I think. . . .
T: You feel some of your needs are met here?
P: Yes, it’s not just, “Okay, I don’t get you, let’s talk about something else,” here at least it’s a point to figure out what is going on in me.
T: You notice that I am interested in understanding you and want you understand yourself.
T: And listen somewhat attentively in a way that doesn’t occur otherwise. . . .
T: Then I would say—oh, I see the time is almost up. I would say that if you feel your personal needs are satisfied by being here, it is through your own openness and taking emotional risks that it happens.
T: There isn’t anything special about me, so if you feel this here, you can feel it other places too, but you lack the belief that it could happen. You are so used to defining yourself as the one who is not chosen and uncertain if you really matter in certain emotional arenas.
P: Sometimes I think I can learn to believe in myself more.
Jayne Payne
Jayne Payne had 39 hours of therapy. All the recorded TIs from beginning, middle, and end phase of therapy are included, as well as illustrative extratransference interpretations and summaries of therapist notes from other sessions.
Session 7.
[Beginning of the session; the patient is skeptical about using medicine]
T: And you think maybe I am skeptical too, but I don’t say what I think.
T: You want more advice and direct feedback from me.
T: When it’s up to you to make decisions, you are unsure.
P: Yes, but when you talk about looking up side effects, I think you are less concerned than the pharmacist I use who always stresses various dangers. I know I’m not careless about using medicine.
P: Otherwise, after the children are in bed, I feel pretty good, I maybe told you I am interested in interior design and keep the house looking nice.
[End of session; the therapist points out the patient’s reservations regarding therapy sessions]
T: You are happy on the days when you are completely free, but on the days you come here you are annoyed that it takes time and. . . .
P: Mm, I like it well enough when I first get here, I combine it with shopping before I come.
T: Yes, but does it disturb you that you have to quit shopping and come here?
T: It also disturbs you when your neighbor wants to chat.
P: Yes, but that’s different.
T: I’m just saying you have an emotional reaction in both cases.
P: But that time you were sick and called to cancel I thought, “Not today when I had so much to talk about!” Then the next time I felt like it would be fine if you weren’t here, but as soon as I knew you were coming it was okay.
P: Today I was glad to come.
T: But you also have clearly begun to feel better and can enjoy some things more even though you are still afraid to go back to work. You have a conflict between bringing in income and taking care of your feelings
T: And you find it difficult that you are expected to take the initiative on your own behalf here. You would like more advice and feedback from me. But the point here is that you say what is important for you even if you feel it is foolish.
Session 16.
[Mid-session]
T: In marital conflicts like those you describe it is easy to find allies for either side. But this is between the two of you and there is a constant conflict. You nag and talk to him like he was a child, do this, do that. . . .
P: No, that is what I should do. I should have given him two empty buckets and told him to fetch water.
T: But he feels he is on vacation and doesn’t have to do things like that.
P: No. I can’t explain it. I heard him tell his parents what a great holiday we had at the cabin.
P: No. There were several situations where it would have been natural for him to help the children but he left it all up to me. [Gives detailed description.] It just sounds ridiculous, I know. You had to be there.
T: Then I could have been the judge of it all.
P: Right. I think you would have given up on him.
T: I thought you said before that work was evenly divided between you.
P: It might be that I’m changing and seeing things differently.
[End of session]
T: I wonder if what you are telling me about your cousin says something about how you feel about coming here.
T: About getting affirmation or not getting it.
P: I don’t really get any, why should you . . . what is in my mind is that I’m totally out of the routine I had for years. Something happened at work.
P: And it has had consequences for how I am, how I see myself and you really don’t know anything about me other than what I tell you. And that is a lot of strange stuff. Like you are some kind of marital counselor or. . . .
P: It drives me crazy that I use all my time here talking about my husband. Last time I said I wanted to go back to school, and when I told my husband he said it was 20 years too late.
T: But what about the affirmation you want here? Is that disappointing?
T: You feel it’s not pleasant, that my style is such that you have to begin. It’s hard.
T: Several times you have said you feel tired when you leave.
T: That you obsess. You get performance anxiety when you come here.
T: You feel you have important things to say but when you say them out loud you are afraid to sound. . . . It seems like you get no relief from coming here, more like mixed feelings with some positive expectations but a lot of disappointment and a sense of getting worn out.
P: Yes, it’s all so banal what I say. I think afterward why didn’t I talk about what bothers me, but I don’t remember it when I’m here.
T: It’s tiring and frustrating.
T: Last time you wanted to quit but I advised you to go this month too and think about it. Did anything occur to you while you were on holiday?
P: No, it was just good to get away.
Session 30.
[Beginning of session; the patient complains about her job and that she cannot face going back]
T: You were glad when your daughter got sick so you got a postponement. You feel I am pressuring you to go back.
T: And I am. You have to do something. Either go back to work or apply for an extension of sick leave. What’s your reaction to this? That I continually remind you, you can’t put this off. I have to say things like now it’s time to apply, you have to get an application form, etc.
P: But it’s not quite the same because. . . .
T: No, I had to say it, and you put off and put off.
T: Procrastinate and “luckily” your daughter gets sick so you can procrastinate some more. You want a way out so you can have a month’s vacation more.
T: It really isn’t that much time.
P: No, it’s like when I see the tram coming and it’s exciting to run across the tracks. I know I can do it, but I might trip. I don’t know . . . about the sick leave. I feel bad when I think about it, but that doesn’t have to mean I will feel bad forever.
T: No, but the longer you wait, the harder it will be to go back, that’s what generally happens. The question is, does what generally happens apply to you? I feel I have to remind you of that. What I’m saying is nothing new. You’ve said it yourself. It’s one of the things you are in conflict about.
T: How do you feel? Is it painful to talk about? Do you get a headache when I remind you about your problems?
P: Yes, something like that. My mind goes blank. I feel embarrassed and my mind goes blank. I feel it’s so wrong to act like this. It’s not right to be like this.
T: Or is it the way I am that it isn’t right to be? Nag you. . . .
P: Yes it is, it’s your job . . . or . . . it’s okay.
T: But you forgive me because it’s my job.
P: I’m not saying you don’t mean it, but it is a part of your job, I would think.
T: But you don’t react when I say it, so you don’t react the same way as when your husband says it and you get furious.
[End of session; the same issues are still being discussed]
T: No, all the things I say to you, you know, right?
T: So I sit here telling you what you already know but can’t deal with.
T: You get irritated if someone close to you says something, but you aren’t able to mobilize any anger toward me because therapists are supposed to be like this.
[Final minutes of session]
T: Mm. But first you need to think what you need in this job. I assume if you go back you won’t work full time, maybe 50%, that you can’t stand more than that. Is that about right?
P: Yes, for now, because you say so.
P: I think that would be ideal, but don’t know. Before sick leave, I thought about working less because I was starting to get mixed up, didn’t know the entry codes for my apartment building and things. I wasn’t myself.
T: You were overtired, worn out.
P: I would forget I had passed the kindergarten when I was picking up my son.
P: I did a lot of strange things. People wondered what was going on with me all the time.
Results
Table 1 shows that at the three-year follow-up, Anne fulfilled the requirements for significant clinical change or recovery on all measures. Jayne had improved, but she was still struggling with symptoms and interpersonal problems (most clearly exemplified by her score on the IIP-C Exploitable/Low Self Assertion subscale); she was also in the clinical range on the other measures.
Research Hypotheses
Hypothesis 1: therapist CT, affiliation, and control.
CT experienced by the therapist and the rater-scored therapist affiliation and interdependence are in the expected direction (
Table 2,
Table 3). In Anne’s therapy, positive CT consistently outweighs negative CT (scores are +13/−0, +13/−2, and +10/−2 for session 7, session 16, and the final session, respectively). Therapist affiliation scores for Anne are also high and fairly stable (56.2, 44.1, and 52.5 for the three sessions). In Jayne’s therapy, positive and negative CT are evenly balanced from beginning to mid-therapy, and negative CT is dominant at the end phase of therapy (scores are +8/−8, +10/−10, and +6/−14 for session 7, session 16, and the final session, respectively). Therapist affiliation for Jayne continually declines (50.8, 46.2, 28.9, and as it declines, therapist control increases (−24.3, −33.7, −44.1). In Anne’s therapy, control is more variable (−2.1, −43.0, −29.7).
Hypothesis 2: patient-therapist collaboration developed in the expected direction.
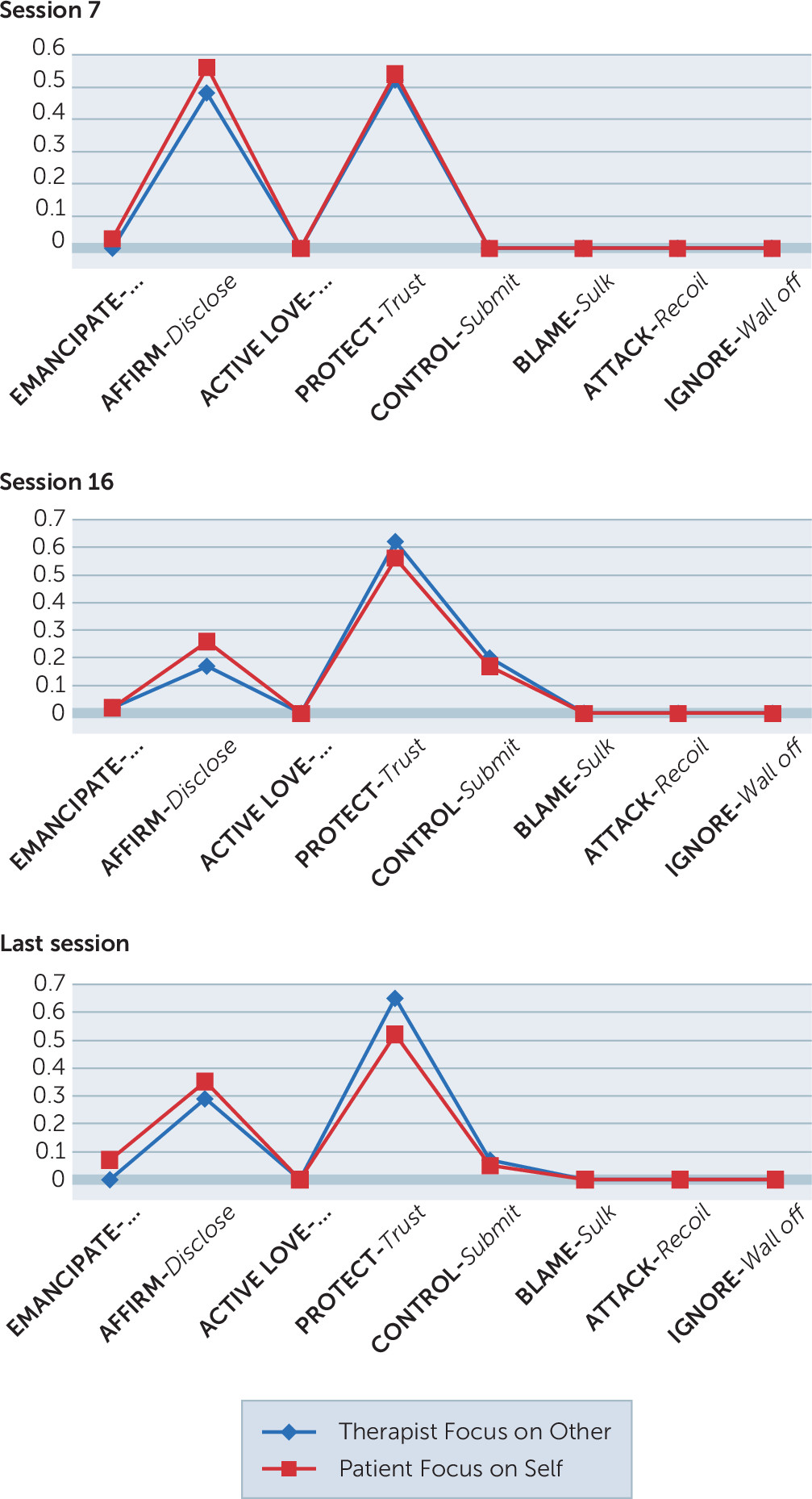
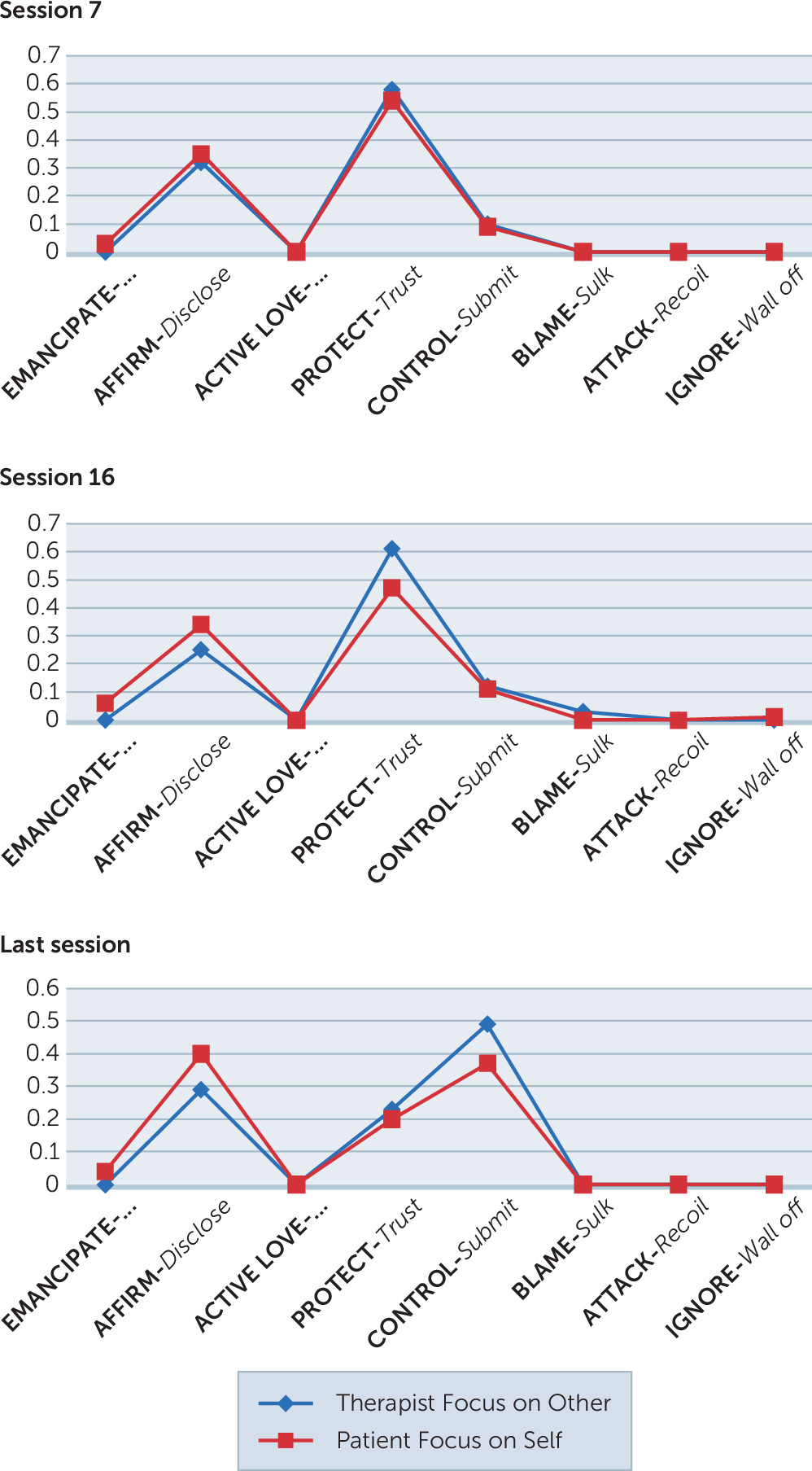
The interaction profiles for Anne and Jayne (
Figure 2,
Figure 3) are both characterized by complementarity (the focus of the patient and the therapist is the patient, with patient and therapist in the same cluster), but there is more disclosure and less control in Anne’s therapy and less disclosure and more submission and control in Jayne’s therapy. Both therapies include considerable cluster 4 activity, but it is important to note that activity between therapist and two different patients is not necessarily alike even if it is in the same cluster. The SASB system is structured such that each cluster shades into the cluster that precedes and follows it. Cluster 4 can range from more friendly guidance that the patient trusts to less friendly interpretation or confrontation that the patient defers to. Transcript analysis of the two therapies leaves a subjective impression of more confrontation and submission in Jayne’s therapy and more guidance and trust in Anne’s therapy.
Table 3 shows a stable, positive affiliation between Anne and the therapist and consistently decreasing affiliation between Jayne and the therapist.
Hypothesis 3: quality of patient participation was also as expected.
Anne’s therapy was characterized by more disclosure (compare
Figures 2 and
3), more affiliation, and less submission (
Table 3), and Anne’s affiliation scores (54.9, 45.9, 47.4) were generally higher than Jayne’s scores (49.6, 45.4, 33.5), which progressively declined. Interdependence scores were not consistently in the expected direction for either patient. Anne was more autonomous at the start of therapy (+10.3), more deferential at mid-therapy (−31.4), and less deferential as therapy was ending (−8.3). Jayne’s interdependence scores were the opposite of Anne’s. There was more deference at start (−16.7) and less at mid-therapy (−7.7); most occurred at the end of therapy (−21.10), and Jayne’s scores did not vary as much as Anne’s. We do not know what is optimal, but some deference during therapy may be necessary for change to occur. Anne’s mid-therapy deference along with her fairly stable, high affiliation may be an indication that the therapy was progressing well and she could allow the therapist to influence her. Patterns of deference and autonomy may also be important, particularly in combination with level of affiliation. Jayne’s deference throughout therapy, together with declining affiliation, suggest a form of insecurity or resistance. Her lower pretreatment motivation score may also capture pessimism or resistance that were not present for Anne, who was highly motivated. Other noteworthy differences are that at the three-year follow-up, Anne no longer fulfilled the criteria for a personality disorder; Jayne was unchanged. Anne’s insight increased substantially (from 62 to 80); Jayne’s increased little (from 62 to 65).
Hypothesis 4: the therapist introject did not develop in the expected direction for Jayne.
Jayne had a high score on continuing dialogue with the therapist (7.2 compared with a mean of 3.6 for the whole group). She also had a high score for mourning the loss of the therapist (5; group mean=1.9) and for experiencing the therapy as a failure (4.3; group mean=2.1). Anne’s scores were 6.2 for dialogue, 3 for mourning, and 1 for failure, which seemed more compatible with her therapy experience. It seems reasonable that she would miss the therapist, continue the dialogue, and not feel the therapy failed. It is harder to reconcile that Jayne mourned loss of the therapist, felt the therapy failed, and mentally continued the dialogue with the therapist.
Discussion
Before treatment, Anne and Jayne were similar on several measures, as noted earlier. They differed with regard to personal problems, symptoms, and motivation. They also had contrasting family backgrounds; Anne’s was more secure and Jayne’s was more chaotic. These factors were the first indications that Jayne might require a different approach than Anne.
After seven weeks of treatment, more negative factors began to appear. The therapist experienced as much negative CT as positive CT for Jayne, and by 16 weeks his affiliation fell as his control increased. Her affiliation fell correspondingly. These trends continued and worsened until the end of therapy. The opposite was true for Anne’s therapy. Roth and Fonagy (
49) have underlined several characteristics of patients who have a poorer than average response to therapy: avoidant and paranoid personality disorders and the combination of axis I depression and obsessive-compulsive disorder (OCD) symptoms together with low motivation, poor alliance, and greater duration of OCD symptoms. Jayne had subthreshold paranoid personality disorder and all the other listed characteristics except avoidant personality disorder. Anne had no avoidant or paranoid personality disorder, her motivation was high, alliance was good, and she had no early OCD symptoms. Roth and Fonagy recommended stepped care—that is, a change of treatment when response is poor—and, because relapse is so common (75% after one year), that maintenance therapy should be considered, based on how chronic the problem is and the age of onset (Jayne was first treated for OCD rituals in childhood). They have also recommended cognitive-behavioral therapy for panic (Jayne’s reason for referral) and for OCD symptoms. In addition, they pointed out that married people (Jayne) do better with cognitive-behavioral therapy and single people (Anne) do better with interpersonal therapy.
Detailed examination of alternative interventions is outside the scope of this article and the FEST project, which was based on dynamic therapy delivered as usual, the only variation being TI or no TI. However, the different responses of these two patients illustrate how important it is for therapists to be aware of the need to tailor interventions to patients. Many dynamic therapists would argue that Jayne could have been treated more successfully within the parameters of dynamic therapy.
As Caston (
13) has pointed out, a successful intervention leads to constructive responses characterized by flexibility, boldness, and relaxation; expansion on the theme introduced by the therapist; and more ability to explore and confront the self. The therapist’s direct and interpretive approach did lead to this result with Anne. She was consistently able to explore and confront herself and work with the therapeutic relationship, whereas Jayne consistently showed resistance to reflecting about problems and the relationship with the therapist. Anne and the therapist seemed to be on the same wavelength, and they constructed a joint understanding. With Jayne, the therapist’s use of provocative statements or questions led to confusion. Some of the best examples from both therapies are found in session 16.
When the therapist says to Anne in mid-session 16, “Partly what makes you angry, or maybe not angry but hurt and wanting to withdraw is when I point out some problem you have,” it leads to a mutual exchange, ending with Anne confirming “yes”; expanding on this by saying, “You hit the mark”; and becoming more bold and self-confrontive, saying, “I feel even more weak.” Her willingness to explore the relationship and express her feelings gives meaning and intensity to the session. Anne’s responses indicate that therapist interventions were effective for her. They possibly allayed the fear of neglect that her distanced caregivers created and alleviated her ingrained tendency to obsess.
In contrast, when the therapist says to Jayne at the end of session 16, “But what about the affirmation you want here? . . . My style is such that you have to begin. It’s hard. . . . You obsess. You get performance anxiety when you come here,” Jayne is only able to answer with a submissive and noncommittal “errr” or “mm.” Her paralysis seems to affect the therapist, too. He never helps her think about why she finds it difficult to talk about their relationship or investigate the “strange stuff” she refers to in this session. Jayne’s inchoate responses suggest that her probable fear of negative reactions based on early experiences was provoked, and her ingrained tendencies to submit, become confused, or distract were mobilized and reinforced. The therapist seemed to be unable to adjust his interventions with her.
As his feelings of being worn out, embarrassed, distant, sad, tired of the patient, resigned, and angry increased, the therapist could have broadened his choice of intervention had he understood his reactions as products of projective identification, that is feelings that Jayne was experiencing while not fully being aware of them. She was unable to express them, and they remained unattended to; the therapist was left with the unresolved problems of his diminishing affiliation as well as his increasing desire to instruct and control Jayne.
Possibly in response to the increasing tension between herself and the therapist, Jayne sometimes complained about the cost and time required by therapy, illustrating the pull of hostility described by Von der Lippe et al. (
28). Her ambivalence and inability to use the therapy could have been addressed with motivation-enhancing interventions. Rollnick and Miller (
50) have described well the directive style of communication that produces anger and defensiveness as opposed to a more collaborative approach that encourages interest in change. Unfortunately, the therapist used more confrontation and interpretation, a tendency described by Høglend and Gabbard (
51) as an attempt to overcome resistance. They found a negative correlation between too many early TIs in the low quality of object relations group and positive outcome (r=−.40). In Jayne’s case, the intensified transference work led to more submission and evasion. The therapist then became more frustrated and less supportive, and a negative cycle became more and more entrenched.
A comparison of the two patients’ background stories adds to an understanding of their different responses. Anne seemed more likely to trust an authority figure or therapist and be interested in achievement in therapy. She grew up with well-educated, ambitious parents who, although they were emotionally distant, created a safe environment. Jayne, whose parents had no advanced education and were far from safe and predictable, might have been expected to be more skeptical and avoidant and less achievement oriented. These characteristics may not only affect the patient-therapist interaction, they may also influence the development of insight, which is necessary for change to occur. It seems not unlikely that the patient who is skeptical and avoidant might miss out on therapist input that could lead to insight, whereas the one who trusts and wants to achieve will do the opposite.
Jayne’s unstable, punitive parents may have created a predominant fear of abandonment and loss, whereas Anne’s distant, achievement-oriented parents may have created a predominantly perfectionistic and self-critical style, as described by Blatt (
52). The latter group responds better to TI. Blatt said that one reason may be that TI relieves the perfectionistic self-critic but provokes the fears of those who dread abandonment and loss. This did seem to be the case with Anne, who responded to TI with strong, appropriate feelings and reflections, whereas Jayne tended to retreat in fear, echoing what the therapist said or responding with one-word replies or just sounds, as though the wrong response would lead to catastrophe. A difficult task in therapy is respecting the limitations of both patients and therapists while taking up the challenge to produce better outcomes.
Jayne’s pretreatment description of feeling as though she was in a centrifuge, together with her several subthreshold personality disorders, suggests a lack of coherent self. She had multiple somatic complaints, possibly as a result of chronic tension from many unresolved, unconscious issues. The fragmented self, the tendency to somatize difficult feelings, and the probable lack of trust after years of emotional abuse and neglect may have been difficult to address with 39 hours of therapy, even had the therapist had been more supportive. Anne, however, had previous therapy experience that may have helped her understand how to use the therapy optimally. She seemed to react to challenge from the therapist as though to the attention she longed for from her parents. It seemed to enhance her confidence and led to constructive responses that allowed her to develop and use her insight well.
Anne’s therapist representation at the end of therapy was as expected. She was not disappointed; she missed the therapist and continued the dialogue with him. Jayne’s therapist representation was possibly a combination of what was actually the case (she experienced the therapy as disappointing) and what she thought she should say (that she missed the therapist). The continuing dialogue could have been negative rumination or attempts to remember and do what she thought was expected.
Conclusions
Anne disclosed more than Jayne and received more affirmation and less control. She not only responded to interventions exploring the therapist-patient relationship and central problems that were defined before therapy, she also often took the initiative in both areas. Jayne held back and took a more deferential, uncertain, or, possibly at times, passive-aggressive role. She was not able to work with TI interventions or central problems defined before therapy began, and the therapist was unable to find a way to help her get on track. He gave her less affirmation and used more control than he did with Anne. Therapist CT was more positive toward Anne than toward Jayne. His negative reactions to Jayne could have been used to better understand her and use more suitable techniques. Both patients made use of continued dialogue with the therapist to a greater degree than did the patient group as a whole. Both patients mourned the loss of the therapist more than did the patient group as a whole. It is likely that they did not experience dialogue and mourning in the same way, given the disparate outcomes. Anne did not experience the therapy as a failure, but Jayne did.
These cases illustrate the importance of recognizing the limitations of both patient and therapist early on and planning how to deal with them to produce optimal outcomes.