Studies have found that people with schizophrenia and other severe mental illnesses experience challenges in the ability to reflect on their own and others’ mental activities and in thinking about specific psychological problems in their lives (
1–
3). The types of difficulties these clients have involve a deficit in the capacity to “think about thinking” and “know about knowing”—a deficit in what is broadly conceptualized as metacognition (
4). Various definitions of metacognition exist in the literature. For example, Wells and Purdon (
5) define metacognition as a multifaceted function responsible for the various roles of information processing “that monitors, interprets, evaluates, and regulates the contents and processes of its organization.” Carcione and Falcone (
6) propose that metacognition consists solely of the ability to understand mental states for the purpose of using them to cope with problems that are a source of subjective distress. A more recent definition defines metacognition as including a wide range of abilities that enable one to perform an ongoing construction of integrative and holistic representations of the self and other (
7,
8).
Accordingly, metacognition is viewed as including a wide range of activities, ranging from discrete activities, in which a person creates an idea about a specific thought or emotion, to more synthetic activities, in which a person forms these distinct thoughts into a complex representation of her- or himself or another person (
8,
9). Studies that assess metacognition according to this definition typically use the Metacognition Assessment Scale-Abbreviated (MAS-A), which includes measures of self-reflectivity, understanding the mind of the other, decentration, and mastery, as discussed later (
10–
12).
In schizophrenia spectrum disorder, these deficits in metacognition are described as being stable over time and are assumed to be traitlike (
13). However, studies have demonstrated that the degree to which these deficits are experienced varies across situations depending on the cognitive and emotional demands of each situation (
14,
15). Moreover, these deficits have been linked to a greater level of psychosocial deficits (
7), pose a risk factor for negative symptoms (
16), are associated with increased positive symptoms (
17), and are linked to impaired social and vocational functions (
18,
19). Deficits in metacognitive abilities may also cause social alienation by making it more difficult for people to form social bonds or seek support from others (
20,
21).
As the interest in conceptualizing and studying metacognition has grown, several psychotherapies targeting metacognition have grown out of their respective therapeutic orientations. For instance, metacognitive therapy (
22) and social cognition and interaction training (unpublished 2006 manuscript by Roberts, Penn, and Combs) approach metacognition from a more cognitive-behavioral framework, using sessions to reframe clients’ thinking about their own thoughts and associated problems, whereas mentalization-based treatment (
23) has a distinct psychodynamic overtone. Relevant in this context may be the claim that people who are exploring their own difficulties and accepting them with self-compassion may benefit from refining their metacognitive abilities (
24,
25). The tendency to accept one’s own difficulties and to be understanding toward oneself when faced with personal failures is conceptualized as self-compassion. It consists of three core components: self-kindness, common humanity, and mindfulness (
26). The literature regarding self-compassion has found associations between this construct and psychological well-being; individuals with higher levels of self-compassion have lower levels of stress and psychopathological symptoms (
27–
29). Among people with schizophrenia spectrum disorder, higher self-compassion scores were associated with fewer negative and positive symptoms (
30). Similarly relevant in this context may be that more integrative forms of cognitive-behavioral therapy for persons diagnosed as having a psychotic disorder have started to include elements from frameworks such as acceptance and commitment therapy (
31). The hope is that with increased self-reflectivity (i.e., meta-cognitive ability), individuals will develop a richer view of themselves that will include more self-compassion.
Although several existing psychotherapies draw strongly on a certain theoretical orientation of the therapist, MERIT is an attempt at an integrative psychotherapy that can be incorporated by clinicians into their existing practice via eight elements (discussed later). Using these eight elements, the therapist assists persons diagnosed as having a psychotic disorder or other serious mental illness to reflect on their own mind and those of others in an attempt to pave the way for a more synthesized understanding of mental states (
32). One therapy goal is to enhance the ability to deal with life challenges using such mental state inferences. Several case studies have illustrated that MERIT is accepted by clients, that it may enhance metacognitive abilities, and that it may improve functioning (
32,
33), even among clients with symptoms that are typically difficult to treat, such as severe disorganization (
34) and negative symptoms (
35). A randomized controlled trial of MERIT is currently underway in the Netherlands (
36).
In this article, we present two case studies in which psychotherapy incorporated MERIT, and we explore the link among metacognitive abilities, global distress, and self-compassion. The assessments of global distress and self-compassion were performed using objective self-report measures taken before and after treatment. Metacognitive abilities were coded at five time points throughout therapy, in equal intervals for each client, to track changes throughout treatment.
Case Studies
Clients and Treatment
The two clients described in this article were recruited from a pool at a community university clinic at Bar-Ilan University, Ramat-Gan, Israel. Therapy was conducted between November 2015 and July 2016, according to the academic schedule, so that the therapy endpoint was predetermined. These clients were chosen for this study from a larger sample of clients according to the criteria of a diagnosis of schizoaffective disorder, according to the
DSM-IV-TR, and treatment length of 25–35 sessions. The study procedures and test battery were part of usual care in the clinic for both clinical and research purposes. Individual psychotherapy consisted of weekly sessions that lasted 50 minutes each. Treatment was based on the MERIT protocol, which was applied in an integrative psychotherapy that included dynamic exploration and the implementation of cognitive-behavioral therapy techniques when needed. This integrative approach is based on recent recommendations for the treatment of schizophrenia (
37). Therapists (NAR and RB) were doctoral students in the clinical rehabilitation program of the Bar-Ilan University psychology department. Each therapist received one hour of individual supervision every two weeks and two hours per week of group supervision. All therapy sessions were audiotaped for use in supervision. The supervisor was a senior psychologist (IHO), and the examination of treatment vignettes was structured to provide specific and direct feedback to supervisees. The study was approved by the university ethics committee.
MERIT Elements
MERIT involves eight elements, each of which facilitates a different type of metacognitive reflection. The first element is the client’s agenda, “attending to the client’s immediate wishes and desires.” The therapist should be attuned to what clients may be seeking and help them develop a greater awareness of their wishes and intentions. Second is the introduction of the therapist’s thoughts in ongoing dialogue; taking care not to override the client’s agenda, the therapist shares his or her thoughts about and perceptions of the client’s activities and behaviors during the session. Next is narrative focus, in which the therapist and client explore concrete examples from the client’s life in the form of narrative descriptions of events. The therapist attempts to facilitate a greater awareness of (changes in) the client’s mental states.
The fourth element is the psychological problem, “attending to [the client’s] sense of the psychological and social challenges [he or she faces].” In this element, the psychotherapist and client recognize the psychological difficulties experienced by the client and work together on the client’s development of awareness of him- or herself as confronted with specific emotional distress. Fifth is the element of reflection on interpersonal processes, or “attending to the clients’ sense of how they are relating to the therapist.” The therapist encourages the client to reflect on her or his relationship with the therapist and to develop a greater awareness of how the client is relating to the therapist. The sixth element, perceptions of change, involves “the therapist attending to the [client’s] sense of what [he or she is] experiencing as it is happening within the session.” Reflection on the sessions should help the client develop a greater awareness of the client’s own experience of progress (or lack thereof) in therapy.
The seventh element is optimal stimulation of reflections about self and others. Using the anchor points of the MAS-A (a metacognitive coding system described in the next section), the therapist ensures the intervention matches the client’s metacognitive capacity to stimulate the client’s attainment of the next level of metacognitive functioning: optimal stimulation of metacognitive mastery, in which the therapist attends “to the client’s use of sense of self and others to recognize and respond to psychological and social challenges.” By using interventions that are appropriate to the client’s current metacognitive capacity, the client will develop an increasing ability to use metacognitive knowledge when responding to psychological and social challenges (
38).
Outcome Measures
Outcome Questionnaire-45.
Outcome Questionnaire-45 (OQ-45;
39) is a 45-item self-report questionnaire designed to measure changes among clients over the course of mental health treatment. Clients are asked to rate their functioning over the past week on a five-point Likert scale ranging from 0, never, to 4, almost always. The OQ-45 possesses adequate test-retest reliability (0.84) and high internal consistency (0.93;
40,
41). In this study, analyses revealed high internal consistency both before (α=0.92) and after (α=0.79) treatment in the original sample of 110 participants. Concurrent validity has been demonstrated with a wide variety of self-report scales (e.g., the Beck Depression Inventory). The OQ-45 is widely used in mental health centers. The total distress score has been shown to be sensitive to change (
42).
Metacognition Assessment Scale-Abbreviated.
The MAS-A (
17) is a coding system for different types of transcripts that enables assessment of metacognitive abilities. It traces the ability to produce a rich and integrative narrative of self and others. The assessment is done using four subscales: self-reflectivity, understanding the mind of the other, decentration, and mastery. Self-reflectivity and understanding the mind of the other measure the capacity to form increasingly complex representations of oneself or others. Decentration measures the ability to take a nonegocentric view of the mind of others and recognize that others’ mental state is influenced by a range of factors. Mastery measures the ability to recognize problematic internal states (e.g., distress) and to respond and cope with psychological problems using increasingly complex metacognitive knowledge (
38). The MAS-A scale is widely used to assess metacognitive abilities; it has been found to be reliable and valid (
13,
18,
17), and scores have been shown to differentiate between persons given a diagnosis on the psychosis spectrum and persons who have no psychiatric diagnosis (
43).
In this study, a doctoral student (NAR) in the clinical rehabilitation program of Bar-Ilan University’s psychology department, who was one of the therapists, coded the therapy sessions after attaining satisfactory interrater reliability. The rating was performed as in other case studies in which therapist ratings were used (
33,
44). The MAS-A reliability and validity have been demonstrated (
17). For each case study, five sessions were chosen and coded. The first and last sessions were coded as a measure of metacognitive levels before and after treatment. Three more sessions were chosen at even intervals throughout the psychotherapy to track metacognitive changes.
Self-Compassion Scale.
The Self-Compassion Scale (SCS;
26) is a 26-item scale that assesses six aspects of self-compassion: self-kindness, self-judgment, common humanity, isolation, mindfulness, and overidentification. Responses are given on a five-point scale ranging from 1, almost never, to 5, almost always. The SCS has an appropriate factor structure, with a single overarching factor of self-compassion, and has demonstrated predictive, convergent, and discriminant validity (
26).
Procedure
Clients and therapists were asked to sign consent forms if they agreed to participate in this voluntary study, and the clients were told they could terminate their participation in the study at any time without jeopardizing their treatment. The OQ-45 and the SCS were administered to clients as part of the intake procedure (i.e., before treatment) and as part of the end-of-treatment procedure (i.e., after treatment). Sessions were audiotaped, transcribed, and then rated using the MAS-A.
Two Case Presentations
Danny
Danny is a single man in his 50s, with a 20-year history of schizoaffective disorder. At the time psychotherapy began, he worked weekends in a coffee shop. He had a limited social network and received rehabilitation services in his home; these services involved a social worker, a psychiatrist, and an employment guide. He was prescribed a routine dose of antipsychotic medication and was symptomatically stable. This was his third year in therapy and his first exposure to the MERIT protocol.
History.
Danny described his childhood as difficult; his family was of low socioeconomic status, and he experienced severe deprivation. His father used physical and verbal violence toward him and his family. He described his relationship with his mother as symbiotic. His mother died five years ago, and he described her death as traumatic for him. Danny described his relationship with his father as distant, and he still views him as a violent and abusive man. Danny has two sisters, and his relationships with both are ambivalent; on one hand, he wants to be close to them, but on the other hand, his sisters display a lack of interest in his life, which he links to his mental illness. Their concealment of his mental illness makes him feel disappointed, ashamed, and alienated from them.
During elementary school Danny preferred to be alone and avoided socializing with his peers. At age 15, he began to experience psychotic symptoms and voiced concerns to which his family was unresponsive. Only three years later, at age 18, did Danny first receive psychiatric treatment, and he was referred to a psychiatrist who prescribed him appropriate medication. Danny was drafted into military service and met regularly with mental health practitioners. After his term in the Army, he worked various jobs with the hope of becoming financially able to leave his parents’ house and move out on his own. He was motivated to do so by his strong feelings of abandonment and solitude.
At age 30, Danny was hospitalized in a mental health institution, at which point he was diagnosed with schizoaffective disorder. After being hospitalized, Danny moved to a community housing institution for people with severe mental illness, and he was provided with work through a government-run program assisting persons with mental illness to integrate into society. Danny has been hospitalized several times in the past two decades. As in his childhood and adolescence, Danny finds it difficult to create meaningful platonic and romantic relationships in his adult life. His few romantic experiences were a source of disappointment; they left Danny with feelings of shame and remorse. He indicates never having experienced a healthy relationship.
Metacognitive assessment.
At the onset of therapy, Danny was able to recognize that his ideas about himself and the world around him are subjective and subject to change over time. He could recognize that others have autonomous mental functions and that he is not the center of other people’s mental activities. In addition, he was able to describe his psychological challenges, which continue to be a source of stress for him.
Course of treatment.
At the beginning of treatment, Danny expressed his expectations for the upcoming therapy and shared details about previous therapeutic relationships and therapy achievements. The therapist asked questions aimed at helping Danny to develop greater awareness of his wishes. His agenda seemed to be focused on improving his interpersonal relationships as well as finding a partner. When asked to answer questionnaires (as part of routine clinic procedure), Danny found the questions upsetting and felt frustrated with the therapist’s request that he answer them. Danny and the therapist explored his strong reaction to the questionnaires, first discussing the dialogue between them before taking a narrative approach in which they explored other episodes in which he had felt these intense emotions. These reflections on himself and others helped them to discover that Danny had previously felt insulted by assessment; he felt it reduced him to numbers rather than a whole (emotional) person. Together, the therapist and Danny decided to forgo the questionnaires altogether, which increased Danny’s trust significantly and allowed him to open up in following sessions. The use of the second element (therapist’s thoughts in dialogue) in this manner, in which the therapist shared her thoughts and perceptions about Danny’s behaviors during the session, encouraged Danny to reflect and helped him to develop a greater awareness of how he relates to the therapist.
From the onset of therapy, Danny was overwhelmed by interactions in his workplace. Despite his desire to talk about other issues, such as interpersonal relationships, the dialogue tended to shift back to issues regarding work. These sometimes contradicting agendas were confusing for the therapist, who struggled with whether to direct the session to the original agenda (i.e., finding a partner) or to focus on Danny’s current difficulties. By concentrating on the first element of MERIT (agenda), focusing on what Danny was seeking at the present session, and the third element (dialogue), by sharing her confusion in light of Danny’s contradicting agendas, the therapist was able to help Danny develop a greater awareness of his own wishes and intentions.
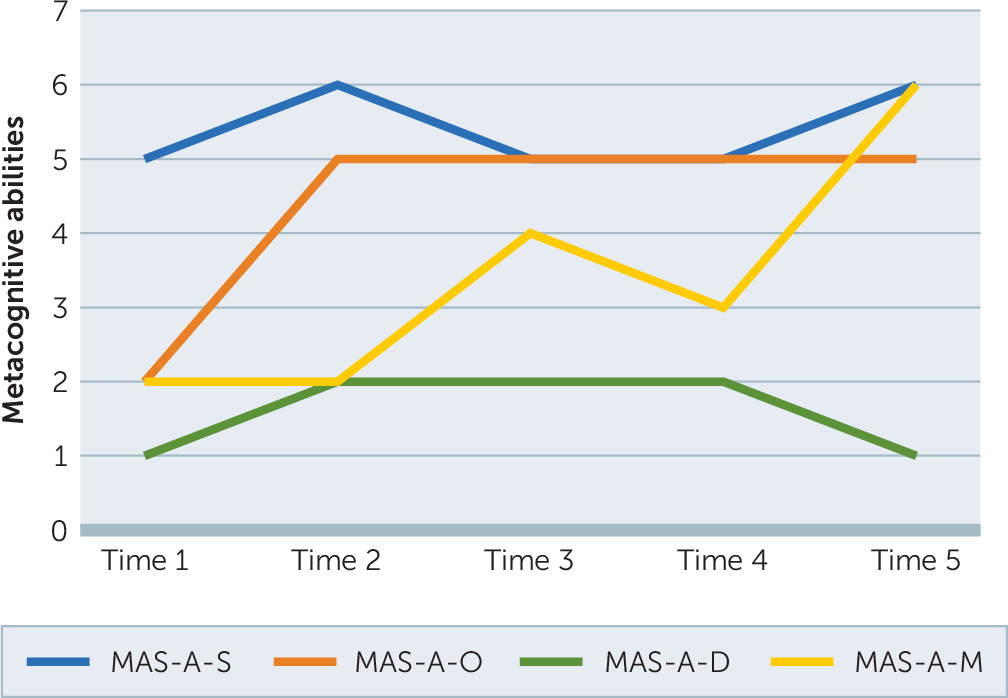
Danny described a significant difference between weekends and weekdays: an intensive overload during weekends and no daily routine during the weekdays. The therapist and Danny discussed the feelings of chaos he experienced at work and the implications of these feelings for his life. During sessions, in a joint effort, the therapist and Danny tried to come to an understanding of which psychological problem underlaid his difficulties at his work. Danny described feelings of social alienation, loneliness, and exploitation. Reflecting on himself and others helped Danny develop a better understanding of the social interactions in his workplace. He came to realize that his expectations might not always match what is possible in reality. He began to understand his difficulties in being aware of his feelings in the present moment and expressing them. Thus, the psychological problem that was discovered was one of emotion recognition and expression within interpersonal relationships. This discovery enabled him to begin to respond to these difficulties by seeking support from others. This enhancement is illustrated in
Figure 1 (time 2, time 3).
The psychological problem element proved instrumental in Danny’s treatment. The joint reflection on and recognition of the psychological difficulties he experienced allowed Danny to further develop his awareness and recognition of his emotional distress. This deeper understanding of the source of his distress made Danny decide to quit his job. Indeed, when Danny announced this recognition, he reported feeling a great sense of relief. This decision seemed to make Danny regain a sense of mastery over his own life that followed his increased self-awareness. After his resignation, Danny’s stress level was reduced significantly, and he felt he was able to focus on his agenda, interpersonal relationships. The use of the first element (agenda) in this manner, in which the therapist was attuned to Danny’s agenda and to the shifts in his agenda between sessions, enabled Danny and his therapist to focus on what Danny was seeking at the current session and helped him to develop a greater awareness that his own wishes and intentions could change. When the therapist assisted him, however, in focusing on this wish, Danny grew concerned, based on his past experiences, that he might get caught up in an abusive relationship. By reflecting on interpersonal processes, the therapist and Danny determined that he did not seem to perceive others as a source of support for him. This perception was also expressed in his apparent lack of interest in being supported and accompanied when he had to have medical tests (routine checkup) performed, which led to feelings of isolation because he felt he had no one to turn to for help.
During this period, Danny reported increased symptoms of social withdrawal, not taking care of his personal and environmental hygiene, and persecutory thoughts and feelings. Joint reflection with the therapist on these experiences led to recognition of Danny’s difficulties in asking for help. To address this issue, Danny contacted his psychiatrist and had his medication adjusted. This change in medication lessened the negative symptoms he was experiencing and provided him with a sense of relief (“I did not realize how much I suffered before”). This example highlights how joint reflections between the therapist and Danny led him to an increased awareness of his own needs, which offered him a stepping-stone to take agency in the form of requesting the medical help he needed.
His medical tests raised fear of loss of independence and concern that he would not be able to take care of himself in the future. By exploring narrative episodes, the therapist and Danny explored together how he felt during previous medical tests, times in which his family supported him, and how this support was experienced. His past negative experiences led Danny to the understanding that he does not want his family to accompany him to medical tests. By attending to Danny’s wishes and desires, the therapist was able to help him develop a greater awareness of his own wishes and intentions. In search of support from persons other than his family, Danny turned to his social worker. To his surprise, his request was accepted. Danny used this exploration of narrative episodes with the therapist (element 3, narrative focuses) to develop a greater awareness of his mental states regarding the support (or lack thereof) he experiences. He then integrated this information and used it to regain a sense of mastery over his life, which in turn reinforced the idea that he could independently find the support he needed. During the course of therapy, intense feelings toward his family arose again. By reflecting on and exploring his emotions with the therapist, Danny was able to understand that when he pushes away his feelings, they tend to intensify. By reflecting about himself and others and on interpersonal processes, Danny was able to recognize and to express his feelings. This expression was new and exciting for him, as he described: “Wow! We are really getting to something here.”
Throughout psychotherapy and by reflection on sessions with the therapist, Danny was able to develop a greater awareness of his own experience. Danny described a social event during which he realized how his point of view of himself and others had changed, noticing how his perspective had changed as a result. Danny then spontaneously revisited the topic of the research questionnaires at the clinic and expressed that he would like to complete them as a means of marking his change and progress in therapy. He felt that answering questions about his thoughts and feelings regarding different aspects of his life would increase his awareness of the changes he was experiencing. This self-awareness also arose in the context of his experience of social interactions and the changes in the feelings he now felt during social interactions throughout the treatment. Perhaps as a result of the narrative focus on his past relationships, he noticed that not only had his views on regular interactions changed, but also his views on romantic relationships.
Danny was not always on time for his sessions and demonstrated great self-criticism when he was late. When, however, he was late for a session toward the end of therapy, Danny broke this habit and demonstrated acceptance and compassion toward himself. He was successful in articulating his growth by using this example to highlight how his perspective had changed in this respect. The topic of separation additionally surfaced as therapy was nearing its ending point. The therapist and Danny discussed the different separations Danny had experienced in his life, and he described that these separations were hard for him and that he used to prefer to simply disappear. Reflecting on this pattern, Danny expressed feeling guilty for abandoning others and wanted to change it. The end of therapy seemed like a good opportunity to experience a new way to separate, and indeed Danny attended every session toward the end of therapy and was able to reflect with his therapist on their mutual feelings during this process.
Assessment of metacognitive progress and outcome.
Danny’s metacognitive abilities varied throughout psychotherapy (
Figure 1). During the final stages of therapy, Danny was able to reflect on the sessions, and he demonstrated a greater awareness of his own experience of progress. Specifically, he was able to pinpoint how his point of view had changed over time. It was apparent that Danny had developed increased flexibility in contemplating difficult life events. Although he had previously viewed past relationships as entirely negative and even abusive, he was now able to see the potential for a healthy, nonabusive relationship in his future. Moreover, the fear he felt about having a relationship with a woman somewhat decreased. At the same time, Danny expressed his disappointment that he was not currently in a romantic relationship despite all these changes, but said he felt closer to fulfilling his wish.
Samantha
Samantha is a single woman in her 50s with a diagnosis of schizoaffective disorder. At the time psychotherapy began, she worked in administration. She had limited social networks and received rehabilitation services in her home that consisted of a social worker and psychiatrist follow-ups. In terms of medication, she had been prescribed a routine dose and was symptomatically stable. This was not her first exposure to therapy, but it was her first experience in therapy using the MERIT protocol.
History.
Samantha described herself as a quiet child, isolated and very imaginative. She had significant learning difficulties at school that did not receive an adequate response. This lack of responsiveness from her environment increased her feelings of isolation and led her to feel a lack of support. Samantha grew up with her parents and two sisters. She described having a good relationship with her father, who died when she was an adolescent. Samantha expressed great longing for her father, a feeling that received no legitimacy from her mother. Samantha described her mother as a manipulative and intrusive woman and their relationship as complex. Regarding her relationships with her sisters, Samantha described caring for them but having experienced rejection from them, and they were not currently in touch. Samantha was drafted into military service and served as an administrator. After her Army service, she moved to her own apartment and started to use substances. During this time, she had her first psychotic episode and was subsequently diagnosed with schizoaffective disorder with significantly disorganized symptoms. She was hospitalized several times in mental health institutions, and since then she has been treated with medication and received rehabilitation services. Currently, Samantha lives alone and has no social relationships.
Metacognitive assessment.
At the beginning of treatment, Samantha was able to recognize that the ideas she has about herself and the world are subjective and subject to change over time. She was able to recognize and distinguish between another person’s different cognitive operations and her own and could recognize that others have autonomous mental functions. Samantha was unable to form a nuanced idea about her affective mental states, nor was she able to recognize her psychological challenges, which are a source of stress for her.
Course of treatment.
During the first couple sessions, Samantha expressed that her loneliness and yearning to find companionship were what consumed her most at that stage in life. To understand what she and the therapist defined as her psychological problem, Samantha and the therapist determined that the difficulty she encountered in her quest to find intimacy was rooted in her struggle to understand herself and others. This problem was evident in the therapy room as Samantha expressed confusion, disorganized speech, and difficulties in reflecting on the therapeutic dialogue. One of the core elements of MERIT is the joint search for the psychological distress the client is experiencing, in a way that can be mutually understood. The understanding of Samantha’s psychological problem became more nuanced through the exploration of her thoughts and by the therapist’s sharing thoughts about Samantha’s behaviors during the session (at Samantha’s level of metacognitive capacity for self-reflectivity). The use of the fourth element (psychological problem), in which the therapist and Samantha focused on Samantha’s struggles, enabled Samantha to be aware of her own emotional distress. This recognition was enabled because her therapist was attuned to what she might be seeking and helped her develop a greater awareness of her wishes and intentions. This enhancement in Samantha’s metacognitive abilities is illustrated in
Figure 2 (time 2).
In the early phase of treatment, when a therapeutic relationship with the therapist was still developing, Samantha spoke freely about past and current issues. She shared her emotional bewilderment with her mother as a child and spoke about relationships in an associative manner. While discussing these issues, it became evident that Samantha experienced great confusion and uncertainty in understanding others. This difficulty was also manifested in the therapeutic relationship; Samantha expressed feeling not understood by the therapist and at the same time seemed to use the therapist’s confusion to feel in control of the session. For example, she repeatedly asked the therapist personal questions about her family status. In response to this, the therapist used element 5 (reflection on interpersonal process) and shared her experience and understanding of the interpersonal exchange (i.e., feeling tense as a result of the personal questions and suggesting that they gave Samantha feelings of control and power). This self-disclosure by the therapist enabled Samantha to reflect on her tendency to enjoy others being afraid of her, led to increased closeness, and facilitated the therapeutic alliance. The use of self-disclosure by the therapist has been suggested by Hasson-Ohayon (
45) as important in improving metacognition and alliance.
Despite the achievement of enhanced dialogue regarding the therapeutic relationship during these stages of therapy, Samantha experienced lack of direction and goals in the therapy and thus frustration. This frustration, combined with the emotional upheaval experienced from discussing life events and the mental energy needed to deal with emergent difficulties, resulted in a brief dip in Samantha’s mastery level (
Figure 2, time 3). Samantha’s lack of direction and goals was also confusing and frustrating for the therapist; she felt that Samantha’s disorganization was an obstacle to treatment. Thus, the therapist decided to work more closely with the protocol, which allowed for a more stable therapeutic environment. Specifically, the therapist began referring to the psychological problem and enabling joint reflection on it. This was done by attuning herself to Samantha’s agenda (what Samantha came to the session for) in a more directive approach, which enabled them to keep on track and sustain a goal-directed manner.
Because of Samantha’s difficulties in piecing together aspects of her life and recalling her personal experience of past events, the therapist was active in helping her chronologically sequence life events and in orienting by applying narrative focus. We previously noted that using a narrative approach to therapy, that is, attempting to discuss concrete life events rather than only abstract thought (e.g., discussing a time when one was angry rather than discussing anger in itself), frequently causes the produced narratives to increase in richness and complexity (
46).
Samantha demonstrated a similar process: As the dyad created order in her recollections of life events, she began to remember more details. Her narratives began to be filled with other persons who were involved and new details about the setting. Consequently, this made it easier for her to contemplate and elaborate on her feelings about and thoughts on the event while reflecting on herself and others, ultimately deepening her sense of mastery and the ramifications of her actions in given past and current events.
During the final stages of therapy, Samantha was able to reflect on the sessions and was more aware of her own experience of progress and lack of progress in therapy. She was able to see how her point of view regarding others had changed and had greater flexibility, which made her feel a sense of accomplishment. Samantha was able to identify and observe her emotions and to integrate her thoughts and actions and see how they interacted. In addition, Samantha had greater flexibility in the way she saw others, especially men. Despite these achievements, Samantha still had difficulty with understanding social cues and, therefore, in dealing with complex situations. She expressed her disappointment that she did not reach her ultimate goal—finding relationships. However, she was able to look forward and see the potential in further treatment in hope of reaching this goal.
Assessment of metacognitive progress and outcome.
Samantha’s metacognitive abilities varied throughout psychotherapy (
Figure 2). As therapy progressed, Samantha became increasingly able to recognize that her self-representation was subjective and that her opinions might change. In particular, Samantha was able to reflect on her new perspective on how she conducts herself in interactions with the opposite sex. She was able to recognize her difficulties in interpreting social cues and the pervasiveness of her overarching generalizations of men. Moreover, she was now able to successfully infer others’ mental states via communicative attitude or behavior in social interactions.
Outcome Evaluation
The MAS-A, OQ-45, and SCS were administered before and after treatment (
Table 1). The reliable change index (RCI) for the MAS-A, OQ-45, and SCS was computed according to Jacobson and Truax (
47), using previous data sets to obtain the standard deviation and a coefficient for each measure. Danny’s and Samantha’s metacognitive ability to understand the other’s mind increased by the end of therapy. The RCI was computed using the standard deviation (1.03) from a sample of clients diagnosed with schizophrenia (
48) and a coefficient (0.82) from another sample of clients diagnosed with schizophrenia spectrum disorder (
18), and it indicated a significant change for both clients. In addition, Danny’s and Samantha’s mastery metacognitive ability, the ability to respond to and cope with psychological problems using increasingly complex metacognitive knowledge, had also increased by the end of therapy. The RCI was computed using the standard deviation (1.19) from a sample of clients diagnosed with schizophrenia (
48) and a coefficient (0.91) from another sample of clients diagnosed with schizophrenia spectrum disorder (
18), and it indicated a significant change for both clients.
The OQ-45 showed that Samantha’s distress levels had decreased. The RCI was calculated using the standard deviation (28.35) and a coefficient (0.934) from a sample of clients with severe mental illnesses in inpatient psychiatric care (
49), and it indicated a significant change. The SCS showed that Danny’s self-compassion levels increased. The RCI was calculated using the standard deviation (0.50) and a coefficient (0.76) from a sample of clients with affective or nonaffective psychotic disorder with a diagnosis of psychotic disorder (
50), and it indicated a significant change.
Discussion
This article presents two case studies of MERIT psychotherapy with persons with schizoaffective disorder. It follows previous case studies in the literature (
32,
33) and a recently reported pilot study on MERIT (
34). It adds to the current literature by adding objective measurements of global distress and self-compassion, as well as five measurements of metacognition throughout the course of psychotherapy. Using multiple time points for assessment allows for an in-depth exploration of the process of change in metacognition. Successful application of the MERIT protocol requires the therapist to attempt to include eight specific therapist activities (elements) in each session and to use an understanding of the client’s metacognitive function that is based on the MAS-A to select appropriate interventions during the session. Because metacognitive capacity fluctuates (upward, in a stair-step manner) during sessions but also between sessions, the therapist flexibly adjusts interventions based on continuous monitoring of the level of functioning. For instance, previously acquired gains in self-reflectivity may not appear in the following session or in a moment when client affect runs high.
Therapy aims, as well as metacognitive abilities, differ among clients, highlighting the varied use of the MERIT protocol and the need to tailor specific interventions to clients’ metacognitive abilities. In the case studies presented here, both clients were preoccupied with interpersonal relationships, and their expressed agenda at the outset of treatment was to form a meaningful romantic relationship. However, the psychological problem underneath each agenda differed; Danny’s focus was on the expression of emotion in interpersonal relationships, and Samantha’s focus was awareness of her own wishes and emotions and understanding her chaotic inner experience. In addition, although the recognition of Danny’s psychological problem occurred in the first therapy sessions, the recognition of Samantha’s psychological problem came later because of her overwhelming emotions and disorganized symptoms. Thus, for the therapist, understanding Samantha was much more of a challenge than understanding Danny. Accordingly, at the beginning of the therapy Samantha’s therapist felt confused and had difficulty adhering to the MERIT elements. However, when therapy progressed, and emotions and thoughts were recognized, confusion decreased.
The differences between the clients can also be seen in their initial metacognition levels. Whereas Danny came to therapy with a high level of self-reflectivity, accompanied by a lower level of awareness of others and recognition of psychological problems, Samantha came with a lower level of self-reflectivity and recognition of psychological problems, but with a higher level of awareness of others. After MERIT, both clients’ ability to understand the other’s mind and to cope with psychological problems using increasingly complex metacognitive knowledge increased beyond the RCI.
The literature regarding change in psychotherapy emphasizes that although change can occur in a gradual and linear way, it can also occur in nonlinear ways, as has been found among clients with differing psychopathologies (
51). Although these patterns were not explored among clients diagnosed as having schizophrenia spectrum disorder, it might explain the nonlinear change in Danny’s and Samantha’s metacognitive abilities, as seen in
Figures 1 and
2. After following a case for more than 32 months, other authors have found a particular stair-step pattern (
52).
Regarding change from pretreatment to posttreatment measures, Danny’s self-compassion increased by the end of treatment. This finding is congruent with the current literature on self-compassion among persons with schizophrenia spectrum disorder, in which associations have been found between higher levels of self-compassion and lower levels of stress and psychopathological symptoms (
30). Although we did not carry out an assessment of symptoms specific to schizophrenia in Danny’s case study, this finding is congruent with Danny’s reports throughout therapy regarding his symptoms and routine medical care.
Another change in scores from pretreatment to posttreatment was seen in Samantha’s global distress level. As reported in other case studies (
32,
33), alongside the enhancement of metacognitive abilities, Samantha’s global distress decreased. In the current case study, this measurement was done using a self-report scale (i.e., the OQ-45). Samantha initially presented as noticeably disorganized, overwhelmed by her own emotions and a chaotic inner experience, for which she was seeking help. After MERIT, her inner experience became less chaotic as she developed a better understanding of herself and others. From the attachment theory perspective, these metacognitive abilities are critical to emotion regulation and self-organization (
23). In addition, it is important to consider the length of therapy. The current case studies lasted for only nine months. Although changes were observed in scores on the OQ-45 and the SCS, as well as on two MAS-A subscales, longer treatment may be needed, and a more comprehensive assessment battery may be needed to see the positive effects of increased awareness and metacognition.
Another important aspect of assessing change throughout psychotherapy is the use of routine outcome monitoring. In the current case studies, the clients were asked to complete questionnaires as part of routine clinic procedure. Danny’s emerging willingness to complete these questionnaires during psychotherapy indicated his wish to increase his awareness of the change he was experiencing. In recent years, using research questionnaires as a part of routine outcome monitoring has become relatively common. As summarized in a meta-analysis, such assessment has several benefits (
53). One advantage is the detection of slight improvements experienced by clients and thus recognition of progress throughout treatment (
54). Although in this study clients and therapists did not receive weekly feedback, by merely answering questions about his thoughts and feelings regarding differing aspects in his life, Danny’s awareness of the change he was experiencing throughout treatment may have increased.
Limitations
The current case studies had several limitations. We described the integration of the MERIT protocol and critical elements in an integrative psychotherapy for two clients with schizoaffective disorder. To provide a further basis for MERIT’s effectiveness, additional studies with more rigorous design, such as a randomized controlled trial, should be carried out. Our case studies were relatively short term, and we did not carry out follow-up measurements regarding metacognitive abilities and symptoms. Therefore, how stable the gains are over time is unclear. In addition, the assessment of symptoms was not specific to schizophrenia. Notably, although the advantage of these case studies is that they used multiple assessment times, longitudinal randomized controlled trials that use additional outcome measures may provide more evidence of MERIT’s effectiveness. In addition, whereas the case studies included multiple times at which metacognitive abilities were assessed, which enabled the tracking of changes throughout treatment, a gap in the self-reflectivity ratings exists in comparison to the case descriptions. Clients’ self-reflectivity ranged wider than captured at the five assessment points throughout therapy. Perhaps more frequent measurements would have better reflected these abilities.
Finally, the role of the therapist and her way of adopting the MERIT protocol and her feelings and thoughts about it were not the focus of these case studies. We assume that the therapist’s reaction to the protocol and countertransference issues played a major role in the therapy process (
55) and, therefore, should be the subject of future exploration.
Clinical Implications
Using the MAS-A to assess the client’s initial metacognitive abilities and deficits provides a starting point at which the therapist can select interventions to match the client’s current metacognitive abilities. Throughout the course of therapy, this assessment can change and, therefore, guide the therapist to adjust to the client’s changing metacognitive abilities and to modify interventions, respectively. Using the MERIT protocol, the therapist helps the client to reflect on his or her own and others’ minds, which subsequently allows the client to form a better understanding of mental states and to respond to challenges in a more flexible and adaptive way. As with any therapy, the therapeutic alliance must be the basis on which the therapist and the client agree on therapeutic goals and develop a good relationship. The therapist and client should explore metacognitive deficits together, and the therapist should attend to the client’s immediate wishes and desires and address the client’s personally defined goals.
Acknowledgments
This article is based on the first author’s doctoral dissertation, Department of Psychology, Bar-Ilan University, Ramat-Gan, Israel. The study was conducted with the support of an internal scholarship. The dissertation was mentored by Dr. Ilanit Hasson-Ohayon and Dr. Dana Atzil-Slonim.