Interpersonal psychotherapy (IPT) and cognitive therapy (CT) are the two most studied, empirically validated, and commonly practiced psychological interventions for patients diagnosed as having major depressive disorder (
1,
2). With initial response rates of up to 60%, IPT and CT have been shown to be at least as efficacious as antidepressant medications in the acute phase of the disorder (
3), and both interventions are currently considered psychological treatments of choice. However, there is room for improvement because approximately 40% of patients do not (sufficiently) respond to initial treatment (
4), and even when depression is treated effectively in the acute phase, rates of relapse and recurrence are high (
5).
Improving treatment starts with a full understanding of interventions. Although our knowledge about IPT and CT has increased tremendously during the past few decades, several issues remain unresolved. For instance, it is not clear how the two treatments compare in the long term. This is especially relevant for IPT, because research on its long-term effects is limited. Furthermore, (person-specific) factors that predict and influence (differential) treatment outcomes remain largely unknown. Moreover, little is known about the pathway through which therapeutic change occurs and the mechanisms responsible for this change.
These questions led us to conduct a randomized controlled trial on the acute- and long-term clinical effects and mechanisms of change of individual IPT versus CT for depression. In this overview, the methods, key findings, and conclusions of this trial are summarized. Our earlier publications (
6–
14) contain extensive discussion of the extant literature and details about the study design, participants, procedures, assessment instruments, quality of the interventions, analytical procedures, and outcomes.
Methods
Participants
Participants were 182 adult outpatients (116 women; mean±SD age=40.5±12.2 years) referred to the mood disorder unit of the Maastricht Academic Community Mental Health Centre in the Netherlands. All patients had received a primary diagnosis of major depressive disorder. Patients receiving antidepressant medications or other psychological treatment at intake were excluded from the study, as were those at imminent risk for suicide. Other exclusion criteria were bipolar disorder or highly chronic depression (current episode >5 years), IQ lower than 80, and substance abuse and/or dependence. All participants provided informed consent and completed an extensive baseline assessment. Structured Clinical Interviews for DSM-IV Axis I and 2 Disorders were administered to confirm the depression diagnosis and to map potential comorbid conditions. After that, participants were randomly allocated to CT (N=76), IPT (N=75), or a 2-month waitlist control condition followed by patient’s treatment of choice (N=31).
Interventions
Treatment consisted of 16 to 20 individual 45-minute sessions (mean=17±2.9). The IPT protocol followed the guidelines of Klerman and colleagues (
15). The CT protocol was based on the manual by Beck and colleagues (
16). Sessions were offered weekly, but the protocol allowed flexibility in scheduling appointments less often later on in treatment. Study therapists (five per treatment condition) received additional training by experts in the assigned therapy before treating participants. During the study, therapists and researchers met biweekly in consultation sessions (separate sessions for each treatment condition). All therapy sessions were videotaped. Independent raters evaluated a random subset of these videos (N=106) to assess the therapist’s treatment adherence (content and quality) and competence. The quality of the therapy given was rated as (very) good to excellent, and treatment dropout was low.
Outcome Measures
The primary outcome was depression severity as measured with the Beck Depression Inventory–II (BDI-II) and, in the follow-up phase, also with retrospective ratings on the semistructured Longitudinal Interval Follow-up Evaluation (LIFE). BDI-II scores range from 0 to 63, with higher scores indicating higher levels of depression severity. Secondary clinical outcomes included general psychological distress (measured with the Brief Symptom Inventory), impairment in social functioning (measured with the Work and Social Adjustment Scale) and quality of life (measured with RAND-36 and EuroQol). In addition, various potential (specific and nonspecific) mechanisms of change were assessed. We were interested in the role of dysfunctional attitudes (measured by the Dysfunctional Attitude Scale form A), interpersonal functioning (measured by the Inventory of Interpersonal Problems), self-esteem (measured by the Self-Liking and Self-Competence Scale Revised Version), rumination (measured by the Ruminative Response Scale), and quality of the therapeutic alliance (measured by the shortened, observer-rated version of the Working Alliance Inventory [WAI-O-S]), among other possible mechanisms. Parallel to these outcomes, we collected data on costs and utility of the therapies (not reported in this overview). Details on measurement instruments can be found in various articles (
6,
7,
10,
13).
Procedure
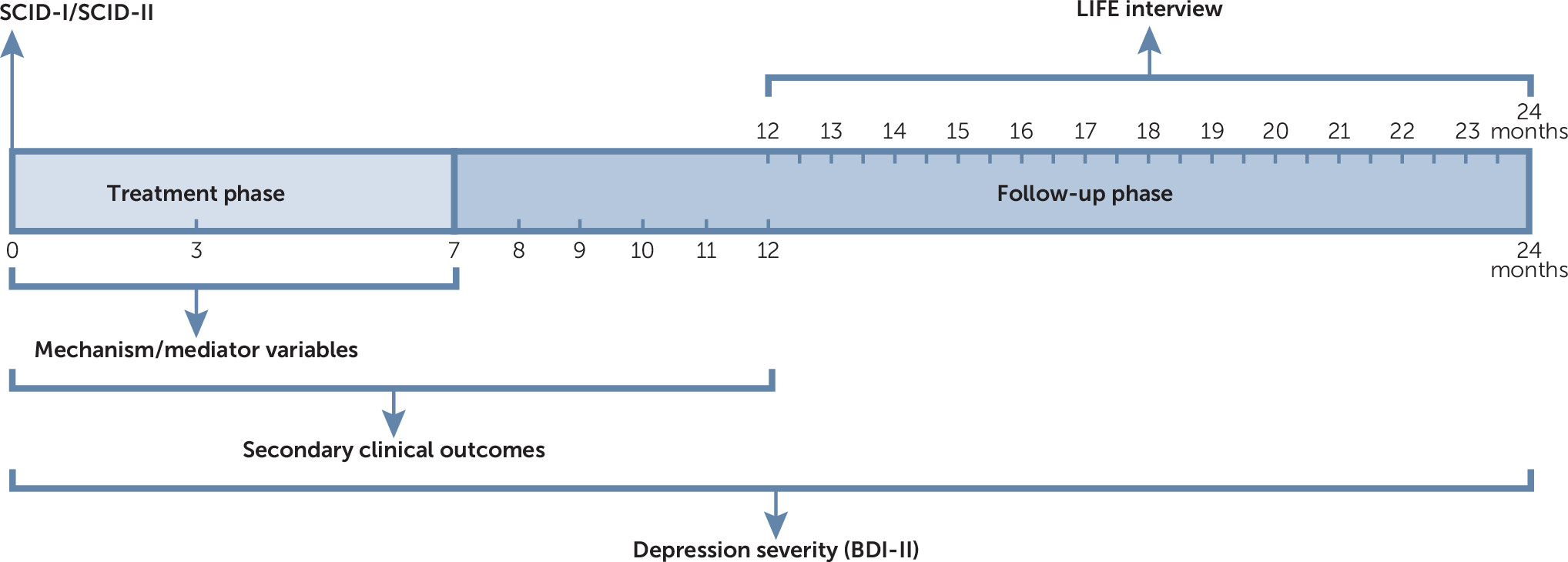
Data were gathered within a 24-month timeframe: 7 months during treatment (treatment phase, months 0–7) and up to 17 months after treatment termination (naturalistic follow-up phase, months 7–24). Recruitment took place from February 2007 to April 2012. Treatment was delivered until December 2012. Follow-up data were complete in June 2014. The main assessment points for the active treatment conditions (IPT and CT) (N=151) were baseline and 3, 7, 9, 12, and 24 months. These assessments were completed, respectively, by 151 (100%), 148 (98%), 134 (89%), 128 (85%), 126 (83%), and 123 (81%) participants. The primary outcome, BDI-II score, was also assessed at 2, 8, 10, and 11 months and prior to each session. The LIFE interview took place after the 24-month assessment and retrospectively addressed the period between 12 and 24 months (
Figure 1). To obtain a measure of therapeutic alliance, we selected three video recordings per patient. These videos were watched and evaluated (with the WAI-O-S) by independent raters. To ensure that the data from the independent raters could be compared with the data from the self-report measures, we selected video recordings of sessions that were closest to the assessment points at baseline and 3 and 7 months. Because of the waiting period of 2 months, study duration for participants assigned to the waitlist control condition was 26 months. Main assessment points for the waitlist control condition (N=31) were baseline and 2 months. These were completed by 31 (100%) and 30 (97%) participants, respectively. Maastricht University’s Ethical Board approved the study protocol, and the study was registered at the Netherlands Trial Register (ISRCTN67561918).
Results
IPT Versus CT: How Well Do They Work and Does One Outperform the Other?
To shed light on the (relative) clinical effectiveness of both interventions, we examined whether the effect of treatment after 2 months was superior to that of waitlist. Furthermore, we tested whether IPT or CT was superior to the other in reducing depressive symptomatology and on a set of secondary clinical outcome measures. By using mixed (multilevel) regression analyses for repeated measurements, we compared interventions in the acute treatment phase (months 0–7) and up to 17 months after treatment termination (months 7–24).
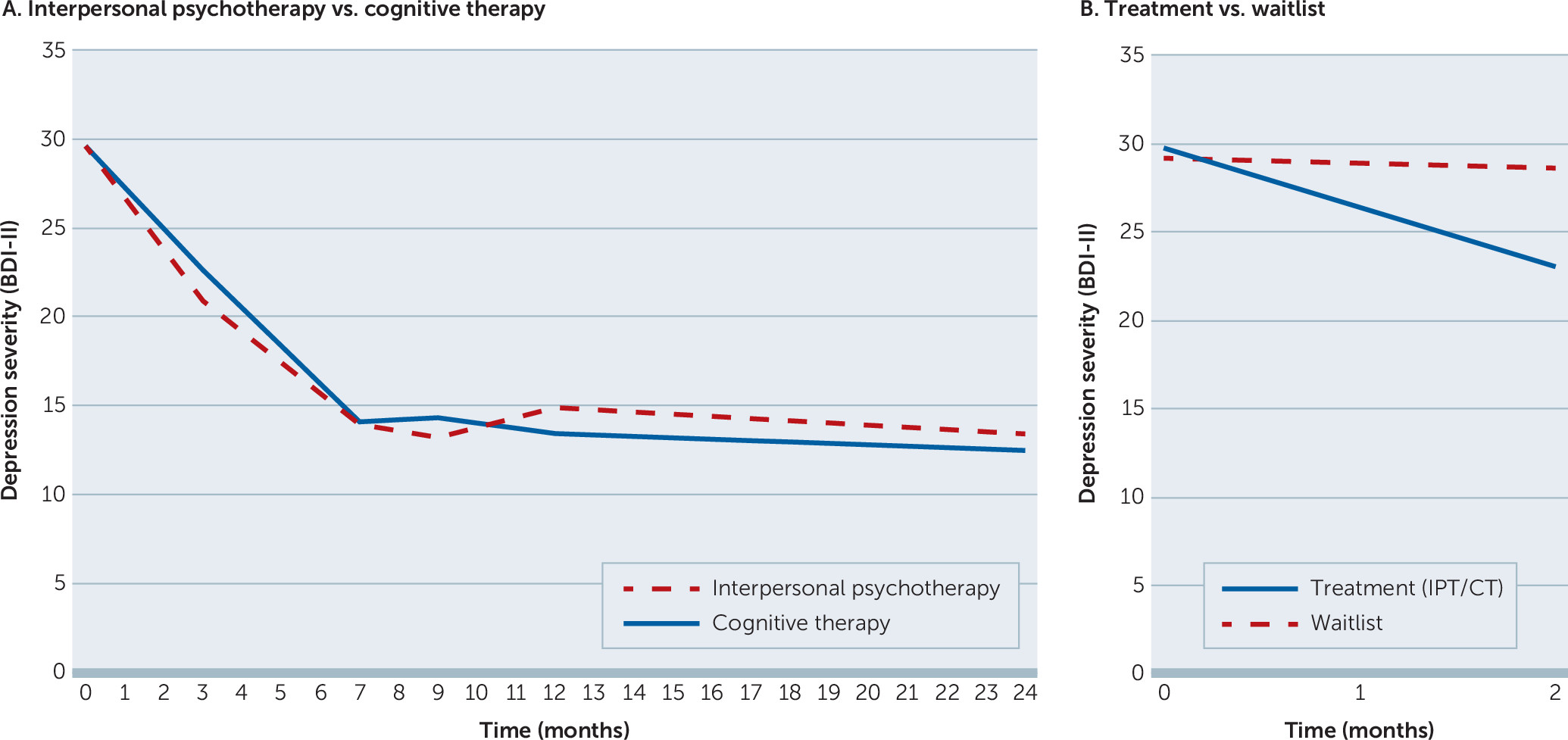
Over the course of treatment, we observed comparable statistically significant and clinically relevant improvements in self-reported depression severity for both IPT and CT (
7). On average, the BDI-II score dropped from 29 (severe depression) at baseline to 14 (mild depression) at treatment termination (pre- to posttreatment effect size Cohen’s d=1.72). A graphic representation of change in depressive symptoms over time stratified by treatment condition is shown in
Figure 2A. At the end of the 7-month treatment phase, two-thirds of patients assigned to one of the active treatment conditions (N=102 of 151, 67%) were classified as treatment responders (decrease of ≥9 BDI-II points over the course of treatment), and 52 of 151 (34%) patients met criteria for remission (posttreatment BDI-II score <10). No therapist effects were found. Response to therapy significantly exceeded response in the waitlist control condition (
Figure 2B), showing that the observed effects were not solely the result of the natural course of depression. Apart from improvements in depressive symptomatology, participants reported considerable and significant improvements in quality of life and social and general psychological functioning (pre- to posttreatment Cohen’s d ranged from 0.68 to 1.01, with no significant differences between IPT and CT). Observed effects were sustained up to 5 months after treatment termination, except for general psychological functioning, which improved further during follow-up.
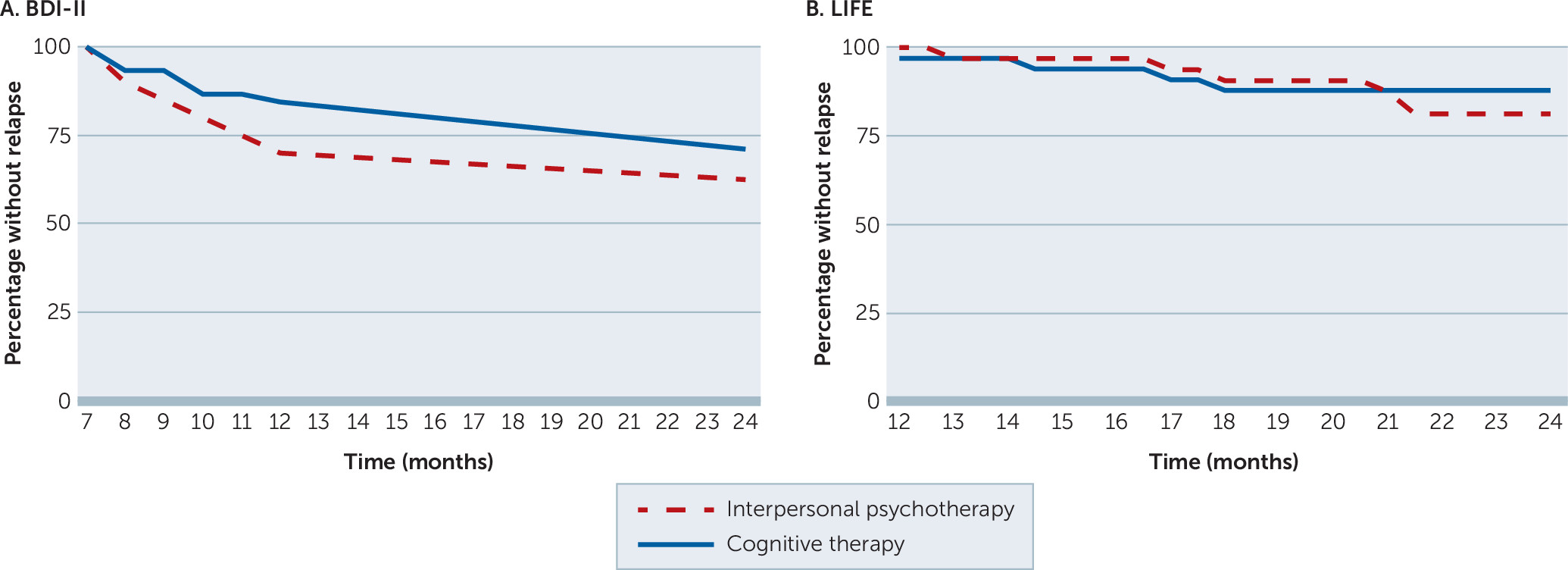
Analysis of BDI-II data from the follow-up phase (months 7–24) (
7,
13) showed that the symptom reduction achieved during the 7-month treatment phase on average was maintained across the follow-up period for both IPT and CT (
Figure 2A). Two-thirds of the treatment responders completed the follow-up phase without meeting criteria for relapse as measured by the BDI-II. Depression relapse rates when assessed with the LIFE were even lower. Cumulative survival rates for time without relapse stratified by treatment condition are shown in
Figure 3. Again, no overall differential effects between treatment conditions were found. In a subsequent analysis (
14), we identified three posttreatment predictors for long-term depression severity: posttreatment depression severity, hopelessness, and self-esteem.
IPT or CT: What Works for Whom?
Despite overall comparability of the interventions, certain (groups of) patients may benefit more from either IPT or CT. We therefore examined associations between various baseline patient characteristics and treatment outcomes. We first examined the role of baseline depression severity, a much-discussed factor of differential treatment effect, which has shown contradictory results in previous randomized comparisons of CT and IPT. One study (
17) concluded that patients with severe depression (BDI-II >29) were better off with IPT, whereas another study (
18) found that CT was more beneficial for this subgroup. In our study, baseline depression severity did not moderate the effect between treatment type and outcome (
7).
Because depression is a disorder with high comorbidity, especially anxiety and personality pathology, we also examined the (differential) effect of baseline comorbid anxiety and personality pathology on outcome (
11,
12). We looked at both full disorder diagnoses as well as symptoms and/or traits of disorders. Comorbid anxiety disorder and symptoms were associated with better acute treatment outcomes for CT. However, this differential effect disappeared during the follow-up phase (up to 5 months after treatment termination). For both treatments, participants with a comorbid anxiety disorder were at higher risk for dropout. The presence of a comorbid personality disorder did not significantly negatively affect treatment outcome during treatment or follow-up. However, we found that patients with higher cluster A and/or B traits did significantly better in CT than in IPT during both treatment and follow-up.
In another analysis, in which we examined the relative contribution of multiple baseline characteristics (
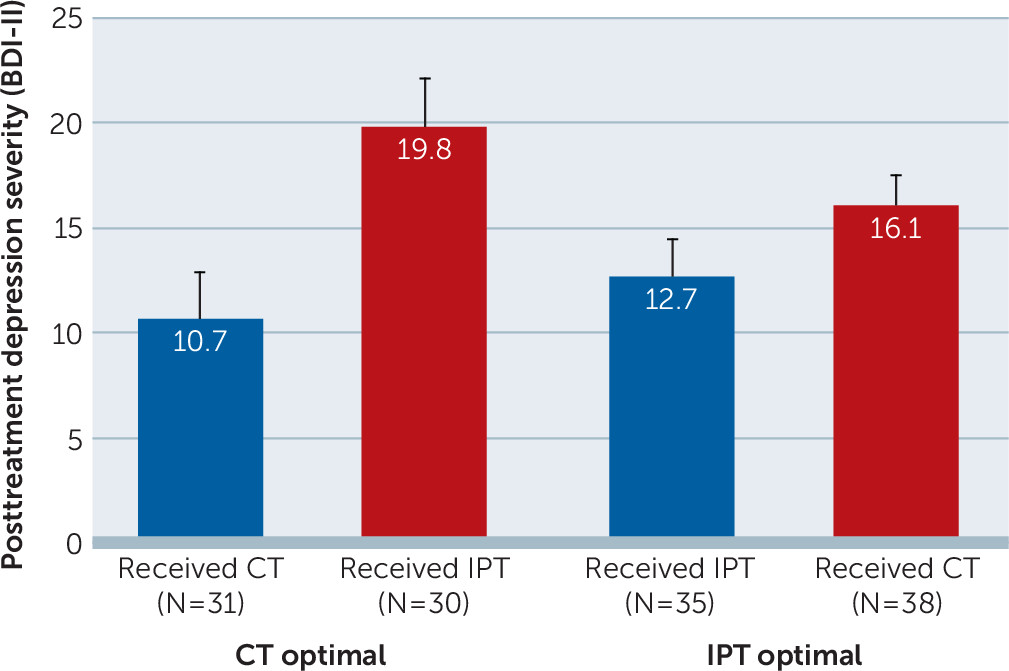
8), we identified five general predictors and six moderators of treatment outcome. Female gender, active employment, absence of a personality disorder, low anxiety, and a high quality of life predicted lower depression symptoms at the end of treatment, irrespective of the intervention received (i.e., predictors). Somatic complaints, cognitive problems, paranoid symptoms, interpersonal self-sacrificing, an attributional style focused on achievement of goals, and the number of life events experienced in the past year all predicted a differential response in CT and IPT (i.e., moderators), with cognitive problems predicting a better response to IPT and the other five predicting a better response to CT. We subsequently combined these factors in the Personalized Advantage Index (PAI) (
19) to form a personalized treatment recommendation. The PAI is a weighted algorithm that predicts which treatment will be optimal for an individual patient. The PAI uses baseline characteristics to retrospectively calculate the predicted outcome for each of the studied interventions. The difference in outcome (in our case the difference in predicted posttreatment BDI-II score in CT compared with IPT) is the PAI score. The higher the absolute value of the PAI score, the larger the predicted advantage for one or the other of the interventions. The PAI scores for a majority of the patients in this analysis (N=84 of 134, 63%) were either higher than 5.0 (indicating a clinically meaningful predicted advantage for CT) or lower than –5.0 (indicating a clinically meaningful predicted advantage for IPT). The average absolute value of the PAI in our sample was 8.9 BDI-II points, indicating substantial differences in predicted outcome for the two therapies. Moreover, we showed that those who had been randomly assigned to receive their predicted optimal treatment had considerably better acute treatment outcomes than those randomly assigned to their predicted nonoptimal treatment (average BDI-II score of 11.8 in the optimal therapy group versus 17.8 in the nonoptimal group; effect size of this difference=0.51). Although this effect was found in both conditions, it was most prominent for patients receiving CT (
Figure 4).
IPT and CT: How Do They Work?
Insight into the mechanisms that are responsible for therapeutic change is important for treatment improvement, because it allows for more targeted use of therapeutic techniques and interventions.
The psychological processes that are assumed to be responsible for therapeutic change are often represented in research by mediators (
20). A mediator is a variable that statistically explains why and in what way a treatment has an effect on outcome, and it can be seen as a proxy of a mechanism. Apart from statistical mediation, it is important to test, among other factors, whether change in the mediator precedes change in the outcome. It is therefore desirable for both the candidate mediator variable and the outcome variable to be assessed at multiple points during treatment.
According to their respective theoretical models, different mechanisms are involved in IPT and CT. In IPT, it is assumed that improvement in interpersonal functioning is crucial for symptom improvement (
15), whereas cognitive theory states that depression severity can be reduced by altering the function, content, and structure of cognitions and schemas associated with depressed mood (
16). Contrary to the view that treatments exert their beneficial effects through their specific theorized mechanisms is the idea that treatments work through factors that are shared by all interventions: the nonspecific, or common, factors, such as motivation or therapeutic alliance (
21). Unfortunately, clear empirical evidence for both of these ideas is lacking (
22–
25).
To contribute to the evidence on the role of mechanisms, we examined the role of five (therapy-specific and nonspecific) candidate mediators: dysfunctional attitudes (representing cognitive theory), interpersonal functioning (representing interpersonal theory), rumination, self-esteem, and the quality of the therapeutic alliance (
10). We examined whether scores on these measures changed during treatment and whether these changes differed in patients receiving IPT versus CT. We then used Pearson’s correlations and latent difference score models to examine the relationships (both concurrent and temporal) between (changes in) each potential mediator and change in depression and tested whether each of these processes evidenced a mediational pattern, even when the criterion of temporal priority was imposed.
Over the course of treatment, scores on all five mediator measures changed in the expected direction. However, change in candidate mediators was smaller than change in depressive symptoms (pre- to posttreatment Cohen’s d ranged from 0.39 to 0.98, versus 1.72 for depression severity) and mainly occurred during the second half of treatment. No significant differences between CT and IPT were found. Change in mediator measures and concurrent changes in depression were strongly related. No temporal mediation was found. Thus, despite a well-considered temporal research design, careful selection of candidate mediators and measurement instruments, and the use of various innovative statistical approaches, we found only limited empirical evidence for the theoretical models of change.
Although pre- to posttreatment changes were comparable, there were indications that the processes through which change was brought about differed between IPT and CT. For example, significantly more patients had sudden gains—large and stable symptom improvements during a single between-session interval—in CT (N=27 of 64, 42%) compared with IPT (N=13 of 53, 25%) (
9). The fact that there were differences in the occurrence of sudden gains in two treatments that overall showed similar outcomes must reflect different mechanisms of change. Furthermore, the identification of various moderators (
8,
11,
12) also suggests differential pathways of change (
20).
Discussion
This overview has summarized key findings of our RCT on the clinical effects and mechanisms of change of individual IPT versus CT for adults with major depression. Our study was the first randomized comparison of IPT and CT that also included a waitlist control group and that examined relative clinical effects up to 17 months after treatment termination. We not only replicated but also extended findings of previous randomized controlled trials that directly compared individual IPT and CT (
17,
18,
26). Furthermore, the temporality of our research design, which included repeated measures of both clinical outcomes, various potential moderators, and specific and nonspecific candidate mediators, allowed for examination of individual treatment effects, mediating factors, and temporal relations, thereby expanding the literature on mechanism research and treatment allocation (
22–
25,
27,
28). By training therapists in a research-oriented clinical setting, we aimed to optimize the quality of the trial as well as the generalizability of its findings.
Conclusions and Recommendations
Several conclusions and recommendations can be drawn from the studies that were presented. First, trial findings add to the accumulating evidence that IPT and CT are efficacious for many patients with depression, both during the acute phase of treatment and beyond. On average, both interventions were superior to the waitlist condition and had outcomes that did not differ significantly from one another. Second, although we did not succeed in identifying the mechanisms through which each treatment brought about its effects in our group-level mediation analyses, the fact that we obtained clear evidence of moderation (subsets of patients responded differentially to the two treatments) suggests that the mechanisms through which change is brought about differ between CT and IPT (i.e., IPT and CT may trigger different mechanisms).
Third, IPT and CT can be offered across a wide range of patients, without special preference for patients with severe depression or comorbid personality disorder. In both treatments, clinicians need to be aware of the higher dropout risk for those with a comorbid anxiety disorder.
Fourth, although IPT and CT tap into more than depressive symptoms alone, change in secondary clinical outcomes and purported mechanism measures was considerably smaller than change in depressive symptoms, especially during the first phase of treatment. This result was underlined by our mediation study, in which we found no evidence for temporal mediation. Fifth, patients who responded to IPT were not significantly more likely to relapse after treatment termination than patients who responded to CT. This finding suggests that IPT may have a prophylactic effect not different from that established for CT. Finally, despite overall lack of difference in effectiveness, for the majority of trial participants, one of the interventions was predicted to be more beneficial than the other. Although the utility of the PAI needs to be evaluated in prospective research and out-of-sample validation, it seems to be a promising method that may advance personalized treatment selection.
Limitations
An important remaining question is why we found only limited empirical evidence for the theoretical models of change. Several explanations for our findings are possible, including that we had a power problem, we focused on the wrong mediators (constructs) or measured them the wrong way, theories were incorrect, or—as is most likely—our study design (e.g., the number of assessment points) or analytical methods (e.g., group level analyses not accounting for individual differences) did not support or allow for sensitive, powerful tests of the relevant hypotheses (
10).
Clinical Implications and Future Research
The studies presented in this overview have implications for at least two major areas of clinical practice. First, our work on individual predictors of differential treatment outcomes has promoted the development of treatment selection approaches that can be used to guide clinical decision making in mental health care, thereby advancing the goals of personalized medicine. Second, our mechanistic work (e.g., our mediation study) may assist in the optimization of treatment delivery itself. However, our findings also illustrate the need for further research (
22,
29). Briefly put, the field would benefit from the further refinement of research methods that have the potential to disentangle mechanisms of change, progress in theory development, and advances in personalized medicine (i.e., person-specific analyses and treatment selection methods). Together, these developments can bring us closer to an empirical foundation for optimized tailor-made mental health care.
Acknowledgments
The authors thank the participating patients and therapists at RIAGG, Maastricht.