Few patients with bipolar disorder experience a simple trajectory of clear-cut episodes and complete recovery. Judd et al. (
1) found that patients with bipolar I disorder were, on average, symptomatically ill 47.3% of weeks throughout a mean of 12.8 years of follow-up. In that study, depressive symptoms were predominant, and subsyndromal symptoms were nearly three times more frequent than syndromal major depressive and manic symptoms. Furthermore, patients with bipolar disorder who had been hospitalized had spent about 20% of their lives in episodes from onset of their disorder, with 50% of those episodes lasting between 2 and 7 months (median=3 months) (
1).
Subsyndromal symptoms of bipolar disorder can contribute to impaired occupational performance (
2,
3); disruption to the quality of relationships with partners, family members (
4,
5), and friends (
6); impaired cognitive functioning (
7); and decreased involvement in social and leisure activities (
8). These occupational, social, and relational dysfunctions reduce patients’ quality of life (
9–
11), and individuals with ongoing residual symptoms have been reported to relapse three times faster than those without residual symptoms (
12).
The usual treatment for bipolar disorder in New Zealand, and in many other countries, includes treatment of an acute episode of mood disturbance (often in an inpatient setting), a period of stabilization of symptoms (usually in community mental health services), and discharge to general primary care services (
13). Clinical guidelines in New Zealand recommend that effective recovery is best facilitated by a combination of pharmacological and nonpharmacological interventions (
14), whereas according to the Canadian Network for Mood and Anxiety Treatments and the International Society for Bipolar Disorders, level 2 evidence supports the use of bipolar disorder-specific psychotherapies for episodes of acute depression and for the maintenance phase of treatment for bipolar disorder (
15). Interpersonal and social rhythm therapy (IPSRT) is one such psychotherapy.
IPSRT combines interpersonal psychotherapy with social rhythm therapy to help patients reduce stressors that may lead to relapse and to learn to live with bipolar disorder and its impact on their lives. This therapy has been described in detail by Frank et al. (
16). It is underpinned by the hypothesis that whereas biological factors play the strongest role in the pathophysiology of bipolar disorder, the timing of individual episodes is strongly related to environmental, psychological, and psychosocial factors. For example, multiple biological processes have been shown to have disturbed rhythmicity in bipolar disorder (
17,
18). As its name implies, IPSRT is underpinned by chronobiology research. Social rhythms have been defined as the social relationships and demands or tasks (social zeitgebers) that entrain biological rhythms (
19).
Most individuals with bipolar disorder report having had symptoms for up to 10 years prior to diagnosis, which usually occurs in their mid-20s. The disorder can impair normal development (
20) and may lead the person to use maladaptive behaviors to manage their symptoms (
21). Interpersonal relationships and occupational and social functioning may be damaged or lost as a consequence of the impact of mood episodes. IPSRT has been specifically developed to address the four basic mechanisms of relapse (biological vulnerability, medication nonadherence, disrupted social rhythms, and life events with specific personal meanings) (
22). The aim of this study was to evaluate the clinical effectiveness (measured by relapse rate and level of functioning) of providing patients with treatment in a bipolar disorder clinic (BC) that combined medication management with IPSRT. Medication management followed clinical guidelines (
14).
As noted, in New Zealand and many other developed countries, patients with bipolar disorder are treated in publicly funded mental health services during an episode, undergo initial stabilization, and are then rapidly discharged back to general practice medical care. This approach does not take into account the chronic relapses common of bipolar disorder nor the importance of ongoing subsyndromal symptoms and functional impairment. We therefore aimed to evaluate the clinical effectiveness of providing treatments in a BC that combined IPSRT and medication management at the point of discharge from publicly funded mental health services. The primary hypothesis was that patients with bipolar disorder discharged from mental health services who were randomly assigned to receive BC treatment would have a lower rate of relapse at 18 months than patients randomly assigned to treatment as usual (discharge to general practice medical care).
Methods
Sample
All participants were patients with bipolar I or bipolar II disorder who had been discharged from publicly funded mental health services provided by the Canterbury District Health Board in Christchurch, New Zealand, during the previous 3 months. Inclusion criteria were being age 18–64 years; not currently meeting criteria for an episode of depression, mania, or mixed state; and being able and willing to sign informed consent for the research protocol. Exclusion criteria were a primary diagnosis of schizophrenia, schizoaffective disorder, or severe alcohol and drug dependence. We registered the study prospectively with the Australia and New Zealand Clinical Trials Registry (ACTRN12611000961943).
Recruitment
All patients with a diagnosis of bipolar disorder were provided with general information about the study when they were discharged from publicly funded mental health services. If patients were interested, they could contact a research nurse who screened them for eligibility and provided them information about the study. Ethical approval was obtained from the New Zealand Health and Disability Commission.
Assignment to Treatment Groups
Patients were randomly assigned to treatment groups by using a computerized schedule. Randomization was stratified based on patients having had ≥12 previous mood episodes, taking into account Scott’s (
23) study, which found that patients with ≥12 previous episodes were less likely to respond to psychotherapy for bipolar disorder.
Initial Clinical Assessment
Following patient provision of written informed consent, the research nurse used a modified Structured Clinical Interview for DSM-IV Axis I Disorders (
24) to conduct a baseline assessment, confirm the diagnosis, and identify any co-occurring Axis 1 disorders or Axis 2 borderline personality or antisocial personality disorder. Baseline medication data were also collected from each patient’s medication data sheets. After this initial assessment, patients were allocated a research ID number and randomly assigned to the treatment-as-usual group or to the specialized BC intervention group.
Measures
The primary outcome measure was the Longitudinal Interval Follow-up Evaluation (LIFE) (
25), which was designed for prospective studies of patients with mood disorders. The LIFE is used to retrospectively rate the severity of depression and mania on a weekly basis over 6 months. LIFE scores are rated on a 0–5 scale, where 0=no symptoms, 3=marked symptoms but not meeting diagnostic criteria, and 4 and 5 indicate meeting diagnostic criteria. In addition, we asked about the age at onset of mood episodes, self-harm behavior, suicide attempts, and medication. The LIFE was completed for each patient at weeks 26, 52, and 78 by an experienced research assistant who was blind to patient therapy allocation. An episode of depression was defined as 2 weeks with scores of 4 or 5, and an episode of mania was defined as 1 week with scores of 4 or 5.
We administered two secondary measures at baseline and at the end of treatment: the Social Adjustment Scale (SAS) (
26) and the Quality of Life–Bipolar Disorder Scale (QoL-BD) (
27). The SAS is a 45-item questionnaire that is used to rate social functioning during the previous 2 weeks across 11 domains: work outside home, housework, social and leisure activities, extended family, marital, parental, family unit, performance, feelings and satisfaction, friction, and interpersonal behavior. Each item is scored on a 5-point Likert scale, with higher scores reflecting greater impairment. The QoL-BD is a 56-item questionnaire composed of 14 domains: physical, sleep, mood, cognition, leisure, social, spirituality, finances, household, self-esteem, independence, identity, work, and education. All 14 domains contain four items, and each item is scored on a 5-point Likert scale. A total score is obtained by summing responses across 48 items (excluding education and work items) and dividing by the total number of items answered, yielding an average score per item, with higher scores reflecting higher quality of life.
Data on readmission to publicly funded mental health services was obtained from electronic medical records. Readmission was defined as any contact beyond a one-time crisis assessment or review and included both outpatient services and inpatient admissions.
Intervention
The intervention consisted of 18 months of IPSRT provided by four experienced therapists (nurses and social workers) and medication management by experienced psychiatrists.
IPSRT.
IPSRT was delivered according to a manualized protocol. Three of the therapists had considerable experience in the delivery of IPSRT and provided leadership for the group supervision for all the therapists. IPSRT included 10–12 weekly sessions, followed by sessions every two weeks, and every month. Patients experiencing deteriorating moods were seen more regularly. Subject to patient consent, all psychotherapy sessions were recorded to ensure treatment integrity and adherence to therapy protocols.
Medication management.
Medication management was based on clinical guidelines (
14). An initial session with a psychiatrist to assess medication needs was followed by medication monitoring and education. The treating psychiatrist saw the patient at intake into the study and monitored the patient’s response to the medication monthly, unless an additional review was initiated by the psychiatrist, patient, or therapist.
Control Group
Patients randomly assigned to the control group remained under usual care from a general practice physician and were provided with information about education and services by Bipolar Support Canterbury.
Statistical Analyses and Power
The primary outcome measure was a binary measure of depressive or manic episode occurrence (i.e., whether or not a participant had experienced a full mood episode). With readmission data collected by the publicly funded mental health services in Christchurch and the findings of a naturalistic study (
28), we estimated that 60% of patients diagnosed as having bipolar disorder and in usual care will meet criteria for a full mood episode within 18 months of discharge. On the basis of the Frank et al. study (
16), we hypothesized that IPSRT would reduce this rate to 30% or less, a difference that would be clinically significant. The study required 42 patients per treatment group to have 80% power to detect this difference (60% vs. 30%) as statistically significant (two-tailed α=0.05).
Patients were classified as having dropped out of the study if we were unable to contact them to obtain data for follow-up. For the primary intention-to-treat analysis, patients classified as having dropped out were considered to have had an occurrence of an episode. We also conducted a per-protocol analysis of the primary outcome, which excluded the patients who had dropped out of the study, and a further analysis in which patients who had dropped out were considered as not having had an occurrence of a mood episode.
We conducted the analyses by using SPSS Statistics, version 25. Descriptive analyses, including frequencies, percentages, and means±SDs, were used to describe the baseline demographic and clinical characteristics of the BC and treatment-as-usual groups. We used paired t tests or chi-square tests to test for significant differences between the groups.
The primary outcome analysis on the intention-to-treat sample and the per protocol sample compared randomized groups, stratified by number of mood episodes, by using the Mantel Haenszel chi-square test. The Mantel Haenszel chi-square test was also used to compare rates of readmission to publicly funded mental health services and end-of-treatment medication use between groups. We also compared total LIFE scores for depression and mania in the two groups over the 78 weeks of treatment. Given the non-normal distribution of the data, we used a nonparametric Mann-Whitney U test to determine significant differences between groups. A Kaplan-Meier survival analysis was also used to determine time to relapse, along with Cox regression analysis to assess the difference in time to relapse between the two groups. The secondary analyses of the SAS and QoL-BD scores compared the mean change (from baseline to end of treatment) between the groups by using an analysis of variance model incorporating the stratification as a fixed factor. We used t tests to compare SAS subscale scores between groups.
Results
Recruitment, Retention, and Sample Characteristics
Participant entry into the study is illustrated, as recommended by the Consolidated Standards of Reporting Trials (CONSORT) guidelines (
29), in a flow diagram available in the
online supplement to this article. Of 157 individuals assessed for eligibility, 67 were excluded. Of those excluded, 20 did not meet criteria (currently experiencing an episode, N=6; did not have a bipolar disorder diagnosis, N=4; discharge greater than 3 months from baseline, N=5; and unable or unwilling to provide consent for the 18-month intervention, N=5), 38 declined to participate, and 10 could not be contacted. A total of 88 individuals entered the study and were randomly assigned to the BC group (N=43) or to the treatment-as-usual group (N=45). Six participants were lost to follow-up (one in the BC group and five in treatment as usual). Four participants in the BC group discontinued the intervention during the 18-month period (see
online supplement).
Baseline demographic and clinical characteristics of the sample are presented in
Table 1. For both groups, a majority of participants had bipolar I disorder and were female. Mean age was 39.9±14.4 years for the BC group and 40.02±13.0 years for the treatment-as-usual group. Mean age at onset of depression was 17.8±7.1 years in the BC group and 21.3±9.4 in the treatment-as-usual group, a statistically significant difference (t =–1.96, df
=83, p=0.05); however, there was no difference between groups in mean age at onset on mania. Comorbid anxiety and substance use disorder were common in both groups, as were previous psychiatric hospitalizations and suicide attempts, with no differences between the groups. There were also no differences between groups in history of physical or sexual abuse, quality of life, or social adjustment.
At baseline, 28% of the BC participants took lithium, 44% took another mood stabilizer, 49% took antipsychotics, and 51% took antidepressants. These data were similar to those of the treatment-as-usual group, with 33% taking lithium, 36% taking another mood stabilizer, 56% taking antipsychotics, and 56% taking antidepressants at baseline.
Outcomes
The primary outcome was the between-group comparison of participants who had a full mood episode (depression or mania) during the 18 months of study treatment, as assessed by the LIFE. In the intention-to-treat analysis, 18 (42%) participants in the BC group had a mood episode, as did 18 (40%) participants in the treatment-as-usual group. No significant differences were observed in rates of mood episodes between the groups (odds ratio [OR]=0.93, 95% confidence interval [CI]=0.37–2.17, p=0.86). In a repeat of the intention-to-treat analysis, in which participants who had dropped out of the study were considered to have remained well, 17 (40%) participants in the BC group had a mood episode, compared with 14 (31%) in the treatment-as-usual group. There were no significant differences in rates of mood episode between the groups (OR=1.01, 95% CI=0.43–2.39, p=0.97).
In the per protocol analysis, 17 (40%) participants relapsed in the BC group, compared with 14 (31%) in the treatment-as-usual group, with no significant differences between the groups (OR=0.76, 95% CI=0.31–1.86, p=0.55).
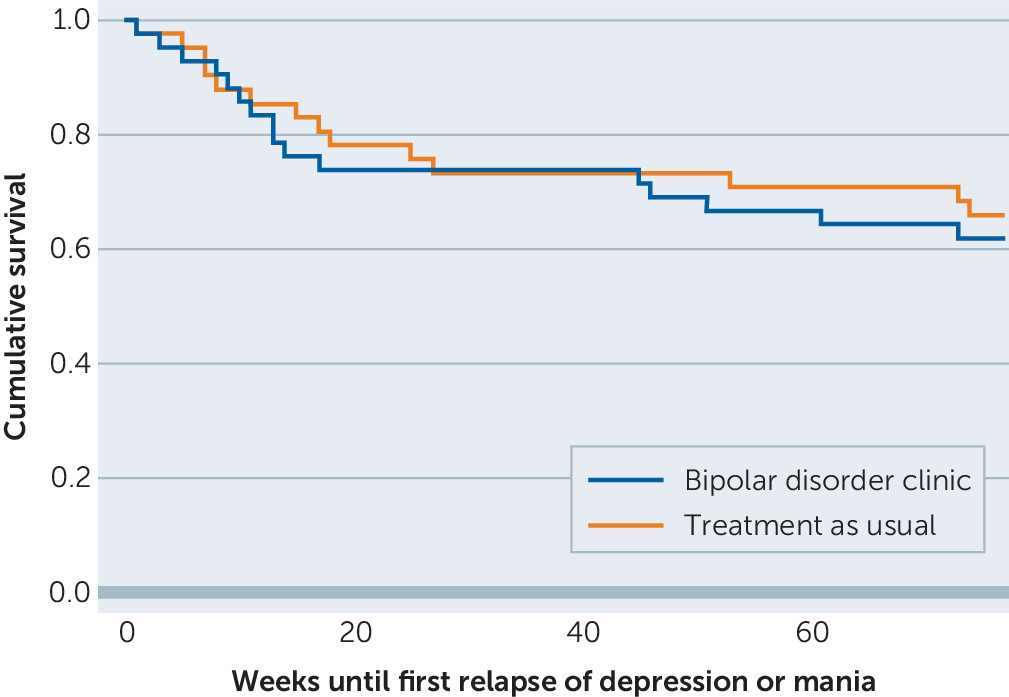
Figure 1 shows time to first mood episode for both groups, with no difference between the groups (hazard ratio=0.92, 95% CI=0.60–1.41, p=0.69). A majority of mood episodes for both groups happened during the first 20 weeks of study treatment.
There were no significant differences between the groups for total LIFE scores for occurrence of any mood episode (U=962.5, p=0.60), depression (U=896.0, p=0.95), or mania (U=1,002.0, p=0.39).
Table 2 presents the median LIFE scores, median LIFE depression scores, and median LIFE mania scores over the 18 months and the change between baseline and 18 months on SAS and QoL-BD scores for the two groups. The only statistically significant difference between the BC and treatment-as-usual groups was the change in SAS scores (overall effect size=0.5). Of the SAS functioning domains, change in the following subscales significantly differed between groups, with all showing greater improvement in the BC group: friction (t=2.58, df=69, p=0.01, effect size=0.67); social and leisure activities (t=2.0, df=69, p=0.05, effect size =0.68); parental (t=2.23, df=20, p=0.04, effect size=0.88); and interpersonal behavior (t=2.532, df=69, p=0.02, effect size=0.54). Change in the domains of feelings and satisfaction, performance, family unit, marital, extended family, housework, and work outside the home did not significantly differ between groups.
Six (14%) participants in the BC group required readmission to publicly funded mental health services, compared with 18 (40%) in the treatment-as-usual group. This difference was statistically significant (OR=3.83, CI=1.32–11.12, p=0.01).
Medication at Follow-Up
End-of-treatment medication information was reported for participants who had taken medication continuously for the last 6 months of the study. In the BC group, the percentage of participants taking lithium and other mood stabilizers at the end of the study was the same as the percentage at baseline, 28% (N=12) and 44% (N=19), respectively; there was a slight decrease in antipsychotic use (49%, N=20) and an increase in antidepressant use (67%, N=29). In the treatment-as-usual group, reported use decreased for all medications compared with baseline, with 30% (N=13) taking lithium, 31% (N=14) taking another mood stabilizer, 38% (N=17) taking antipsychotics, and 40% (N=18) taking antidepressants at the end of the study. The only statistically significant difference between the BC group and the treatment-as-usual group was in antidepressant use at the end of treatment, with higher use of antidepressants among the BC group (OR=0.34, CI=0.13–0.87, p=0.02).
Discussion
For the primary outcome, rates of recurrence of a mood episode, no difference was found between the groups. Total symptoms, both depressive and manic, across the 78 weeks did not differ between the groups. Change from baseline to follow-up in QoL-BD scores did not differ between groups, but SAS scores in the BC group showed significantly greater improvement compared with the treatment-as-usual group. The effect size of this difference was moderate (0.5). The functioning domains that significantly improved were friction, social and leisure activities, parental, and interpersonal behavior. A statistically significant difference (p=0.01) was found in readmission rates to mental health services, with the BC group having fewer readmissions.
The finding of no difference in relapse rates was counter to our primary hypothesis. Both groups had relapse rates of about 40%, which was lower than expected, suggesting that the patients recruited for the study were relatively more stable than expected. Most patients who relapsed did so within the first 20 weeks of the study. Although the relapse rates were similar between groups, the patients in the BC group were less likely to require readmission to mental health services.
The significant difference between groups in the degree of change in functioning showed an improvement in the BC group but no change in the treatment-as-usual group. It is difficult to quantify what this improvement means in real life, but an improvement of 0.2 equated to an average improvement of 0.2 on each item or (given that most patients responded to about 50 items and scores were averaged across items). For example, an improvement of 1 out of 5 points on 10 of the items would show an improvement of 0.2 across the scale.
Studies have repeatedly identified significant functional impairment among patients with bipolar disorder, even when the analyses have been controlled for concurrent levels of depression (
30–
32). Whereas symptomatic recovery and relapse prevention are important, so too, is functional recovery (
13). The traditional clinical emphasis on acute symptom reduction has shifted to include longer-term focus on recovery of functioning in everyday life (
33). It has been estimated that 79% of the societal cost of bipolar disorder is due to indirect costs, such as functional impairment, rather than to direct treatment costs (
34). Similar to self-management programs for chronic physical conditions, the BC intervention was focused on promoting self-management and teaching the participants to live well in the presence of symptoms. This focus may have had an impact on the low readmission rate and improved levels of functioning.
Frank et al. (
35) found that 2 years of IPSRT improved occupational functioning by ameliorating interpersonal and role functioning. The BC group also made interpersonal gains, although many of the patients did not work outside the home. The areas of significant improvement (friction, social and leisure activities, parental, and interpersonal behavior) were those that could be regarded as targets for IPSRT. The participants in the BC group had less conflict with others; were more socially engaged and engaged with their children; and were more able to discuss feelings, seek support, and make decisions. Participants skipped questions on work and marriage if these did not apply to them. The social rhythm component of IPSRT emphasized stabilization of social rhythms to enhance stability of biological rhythms. Biological rhythm disturbance has been identified as a predictor of functional impairment (
36) and may provide a rationale for the greater improvement in functioning experienced by the patients in the intervention arm.
Because of the regular medication reviews conducted by psychiatrists with expertise in treating bipolar disorder, which specifically adhered to clinical guidelines, we expected to see differences in medication prescription between the two groups. However, the only difference was a higher rate of antidepressant prescription among participants in the BC group. The lack of alterations in use of mood stabilizers and antipsychotics during the study, and the lack of difference between the treatment groups, may have been because patients were relatively stable and had arrived at a combination of medication determined by their previous psychiatrists over a period of time and possibly over many years of intermittent contact with specialist services. The higher rate of prescription of antidepressants among patients in the BC group was probably related to a higher awareness of depressive symptoms because of more regular and intensive reviews than would have occurred in general practice and because the therapists brought these symptoms to the attention of the psychiatrists. However, the fact that this increased use of antidepressants among patients in the BC group was not accompanied by a reduction in depressive symptoms as measured by the LIFE is notable and suggests either that the LIFE was relatively insensitive in this regard or that the use of antidepressants did not prevent relapse. The increased use of antidepressants was not associated with manic relapse, which would be a theoretical concern (
37). However, because the groups were small, most patients were taking mood stabilizers, and the medication treatment was closely monitored, it is not surprising that no difference in manic or depressive relapse was seen.
This intervention following discharge from publicly funded mental health care was relatively intensive compared with treatment as usual—in this case discharge to general practice medical care, which was likely to involve irregular follow-up and medication management. It is unlikely that the patients in the treatment-as-usual group received any form of psychotherapy, although some may have accessed a peer support group, which was operating in the city during half of the study. Forty percent of patients in the treatment-as-usual group were readmitted to publicly funded psychiatric services during the study. This rate was significantly greater than the readmission rate for the BC group, which may have been because patients in the BC group were in effect receiving specialist outpatient psychiatric service. The high readmission rate among the treatment-as-usual group, however, may have diluted the differential effect of the BC treatment, because many patients in the treatment-as-usual group ended up receiving specialist rather than general medical treatment. No bipolar disorder-specific therapies were available from publicly funded mental health services at that time, but patients may have accessed other generic psychological input. The lack of major differences in medication management between the two groups suggests that IPSRT was the factor that conferred a greater improvement in functioning among the BC group.
There are few similar studies with which to compare our results. A Danish study (
38) found a significant reduction in in-patient hospital readmissions—36% of intervention group patients and 54% of the treatment-as-usual patients—after 2 years of treatment in a specialist BC. Our previous study identified that 18-month IPSRT, in combination with medication, significantly reduced mania and depressive symptoms at 18 months and after 3 years of follow-up, and that specialist supportive care resulted in similar reductions for depressive symptoms (
39,
40).
The design of this study resulted in some recruitment issues (approximately one-third of those who showed initial interest and met inclusion criteria declined to participate) and contributed to a sample that was more stable than expected. A series of major earthquakes that caused citywide destruction and disruption occurred during the early stages of the study, influencing potential participants’ willingness to participate. The effects of this event are unlikely to have differentially affected one group over the other, however, especially in the context of the lack of overall difference in mood measures between groups. The use of the LIFE as a primary outcome measure may have also been a limitation. A measure that requires retrospective self-report of mood symptoms over a 6-month period by patients who, as reported in the literature, may have ongoing cognitive difficulties, may not be ideal. Further research is required to determine the accuracy of such a measure in this situation.
Conclusions
This pragmatic clinical effectiveness trial found that a combination of IPSRT and medication management over 18 months did not significantly improve mood relapse but did improve patient functioning. In the absence of sensitive measures of symptoms over time, future research needs to focus on multiple aspects of recovery for patients with bipolar disorder. The promotion of recovery among patients with bipolar disorder needs to include an emphasis on function, along with strategies to manage symptoms and early warning signs. Our results suggest IPSRT is an intervention that has the potential to promote the process of functional recovery among patients with bipolar disorder.