Functional impairment is a key consequence of depression in both major depressive disorder (
1) and bipolar disorder (
2). Impairment in functioning persists even after 3 years of recovery from depressive symptoms (
3) and is correlated with unemployment, disability, and decreased work performance (
4). This impairment has significant personal, social, economic, and health services impacts. Because impaired functioning is a strong predictor of outcome and relapse, the traditional clinical emphasis on symptom reduction has shifted to include recovery of functioning in everyday life (
5).
Disruption in biological rhythms has been associated with poor functioning among patients with bipolar disorder or major depressive disorder (
6,
7). Additionally, evidence suggests that both circadian and sleep disturbances are important in the pathophysiology of depressive episodes in both disorders, and that these disturbances can affect neurocognitive and general functioning (
8). The circadian hypothesis of depression suggests that disruption of social rhythms and the resulting disruption of nonphotic zeitgebers that normally entrain physiological circadian rhythms trigger depressive episodes among vulnerable individuals (
9). Interpersonal and social rhythm therapy (IPSRT) is an intervention designed to address both social rhythms and interpersonal functioning (
10). A systematic review (
11) of the evidence found IPSRT to be a viable therapy for acute treatment of patients with bipolar depression and for prevention of bipolar mood episodes. There is some evidence that IPSRT also improves functioning (
12–
14). Although no studies have been conducted on the use of IPSRT for patients with major depressive disorder, a recent safety analysis (
15) found that the delivery of IPSRT to patients with major depressive disorder was safe and revealed a strong indication of improved moods and functioning.
Neurocognitive deficits are a core feature of major depressive disorder (
16) and bipolar disorder (
17). There is some evidence that functional impairment is underpinned by residual cognitive impairment (attention, verbal learning and memory, psychomotor speed, and executive function) associated with a depressive episode (
18). Cognitive remediation (CR) is designed to target neurocognitive impairment through online computerized exercises and strategy coaching, completed at home and explored during therapy sessions (
19).
Research is increasingly examining how to achieve functional recovery rather than focusing purely on mood symptoms (
20). To address this goal, it has been suggested that researchers need to consider the perspectives of patients and the problems they perceive in their daily lives (
21). The present study was designed to capture participant perspectives on a 12-month adjunctive psychological treatment for mood disorders. The study aimed to examine participants’ experiences of a psychotherapy (IPSRT with or without CR) and the impact of this intervention on their functioning.
Methods
We chose to undertake a qualitative study to enable in-depth exploration of participants’ experiences of the intervention and its impact on their functioning. Our process of interpretive thematic analysis followed the method described by Braun and Clarke (
22) and was underpinned by a critical realist theoretical position, and an ontological position that assumes that people’s words provide access to their particular version of reality, which, thus, fit the patient-centered approach used in this qualitative study. All authors, apart from the research nurse who conducted the interviews (H.W.), either delivered the therapy or provided medication management as part of the larger randomized controlled Enhancing Recovery Study (ERS). Others involved in this qualitative project were a nurse, two psychiatrists, two psychologists, and a social worker. The research nurse (H.W.) had the interviews transcribed using unique identifiers, and the two authors who conducted the analysis (M.C. and M.I.) did not know which transcript belonged to which participant. Demographic data were correlated with the interview transcripts after the analysis.
Intervention
Participants who were 18 years old or older and had been recruited into the ERS within 3 months of discharge from public mental health services after treatment for a moderate-to-severe mood episode (major depressive disorder or bipolar disorder) and clinician- or patient-rated cognitive impairment. The ERS was a 12-month randomized controlled trial of adjunctive IPSRT compared with adjunctive IPSRT+CR. At baseline, diagnosis of major depressive disorder or bipolar disorder was confirmed through the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (
23). Participants were prescribed medication by treating psychiatrists who saw them on at least three occasions during the 12-month intervention: at baseline, 6 months, and follow-up.
IPSRT has been described in detail (
10). It is a combination of interpersonal psychotherapy and social rhythm therapy conducted in face-to-face sessions by trained therapists weekly, for two initial sessions, and then twice monthly or monthly, depending on patient need. The CR intervention involved a 12-week program of online cognitive activities (
www.scientificbraintrainingpro.com) that was completed in session and at home and was supported by its integration into therapy sessions. The CR activities are designed to improve attention, executive functioning, and memory. Diagnoses were based on the results of the baseline SCID for each participant. Participants’ mood states were regularly assessed with the Quick Inventory of Depressive Symptomatology (QIDS) (
24) and the Young Mania Rating Scale (YMRS) (
25).
Therapy was delivered by three nurses, two psychologists, and a social worker, who were trained in and had extensive experience in the delivery of IPSRT. Fidelity to the therapy method was ensured by the presentation of cases and clinical formulations at peer supervision meetings every 2 weeks and by having a senior therapist review audio recordings of sessions.
Participants
Eligibility criteria for participants in this qualitative study were the same as the RCT: major depressive disorder, bipolar disorder, discharge from public mental health services within past 3 months, clinician-reported cognitive impairment. The interviews for our qualitative study were conducted with 10 consecutive patients who had completed IPSRT and 10 who had completed IPSRT+CR. The first 10 completers in each group of participants agreed to take part in the interviews. On the basis of Braun and Clarke’s (
26) recommendations for sample size, our sample consisted of 20 patients.
Ethical Approval
All participants provided informed consent, and ethical approval was provided by the New Zealand Northern A Health and Disability Ethics Committee (16/NTA/64/). We used research identification numbers for the digital recordings and transcripts of interviews, all identifying information was removed before storage, and the recordings and transcripts were stored in secure online facilities provided by the University of Otago, Christchurch. Participants in the qualitative study provided informed consent at ERS baseline to take part in the follow-up qualitative interviews.
Data Collection
The qualitative interviews were conducted by three clinical research nurses (not responsible for therapy delivery) after the intervention was completed. The interviews were conducted face-to-face and were between 30 and 45 minutes in duration. Follow-up interviews took place 1–2 weeks after completion of the intervention. The semistructured interviews focused on the participants’ descriptions of their experiences of the intervention and of its impact on their functioning and everyday lives. The interview questions focused on current mood, ability to function (relationships, occupation, cognitive functioning), helpful aspects of psychotherapy, helpful aspects of CR, and unhelpful aspects.
Data Analysis
A thematic analysis (
22,
27) was conducted on the transcribed texts of the interviews. Two authors (M.C. and M.I.) independently read and reread the interview transcripts to become intimately familiar with the data. This reading was followed by independent generation of initial codes. The codes were then discussed and agreed upon before they were clustered into shared meanings related to the participants’ experiences of the intervention’s impact on functioning and of the therapy process. We then returned to the data that informed all of the codes in order to identify themes related to the participants’ perspectives on how the therapy affected their functioning. These themes were discussed among the research team, and consensus was reached. The development of themes from these clusters is illustrated in a thematic map (
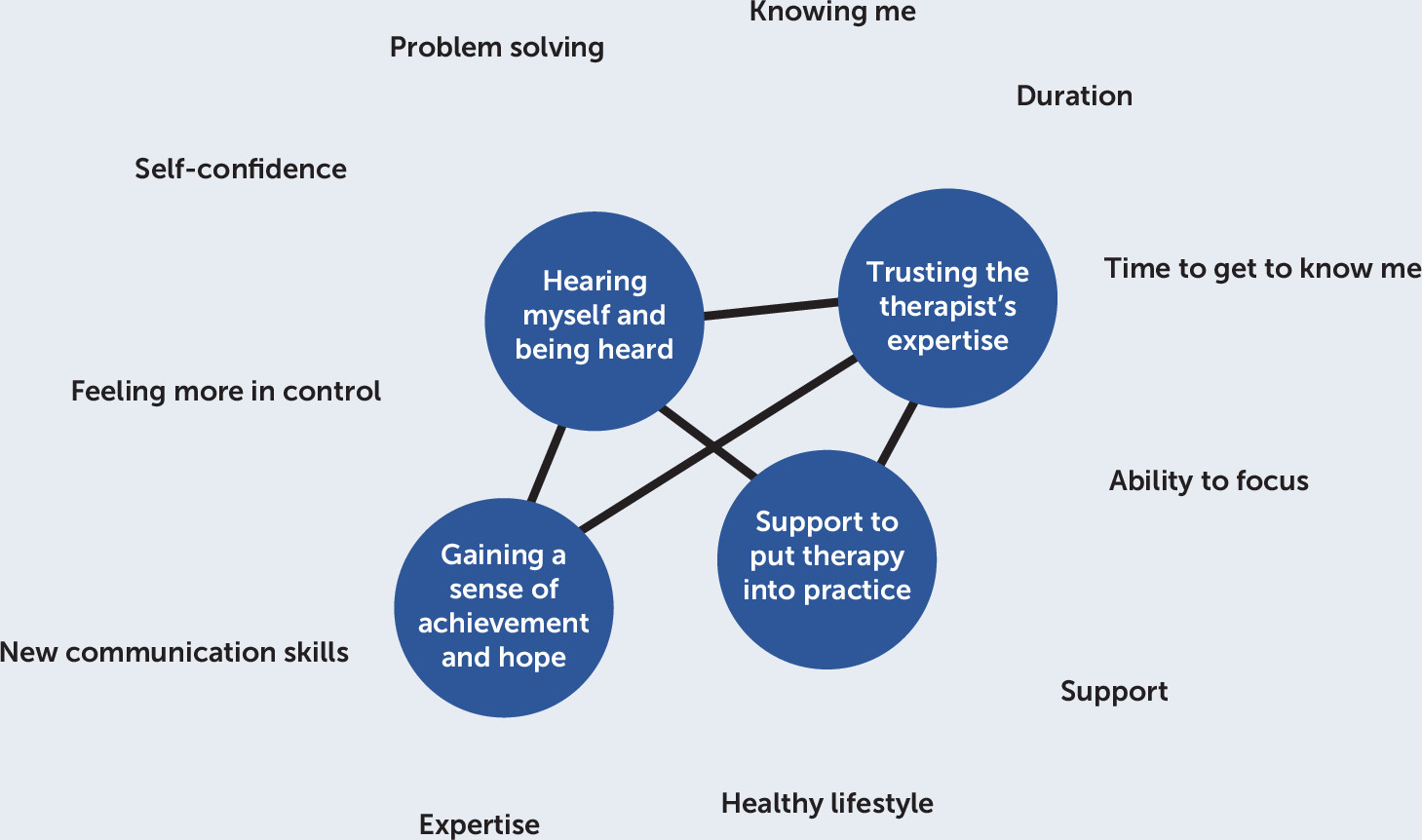
Figure 1).
Rigor
The hallmarks of qualitative rigor have been described by Koch (
28): credibility, transferability, and dependability. Two authors (M.C. and M.I.) independently coded the data and then worked with the other researchers to develop a consensus on the themes. Details of the interventions and setting are provided above. The interventions are described and can be replicated. The interview questions and the process of coding and theme development are described, and the codes have been provided within each theme to enable readers to see the process of development. The use of quotations below provides an illustration of each of the themes.
Results
The 20 participants had the following diagnoses confirmed by SCID-I (
23): major depressive disorder (N=9), bipolar I disorder (most recent episode depressed) (N=6), or bipolar II disorder (most recent episode depressed) (N=5). The sample included 11 men. The participants ranged in age from 22 to 55 (median age=32). Thirteen people identified as New Zealand European, three as Māori, one as Pacific Islander, and three as other. Ten participants had been randomly assigned to receive IPSRT+CR and 10 to receive IPSRT alone. Because the treatment allocation was not blind to either the patients or the therapists in the ERS, we did not break the blind in undertaking the qualitative aspect of the study. At baseline, eight patients were not currently experiencing a mood episode, eight met criteria for mild depression, three for mixed mood, and one for moderate depression. At the time of the follow-up interviews, no participants met criteria for a mood episode. Four of the 10 participants in the IPSRT+CR arm did not complete an adequate dose (defined as <75% of activities) of the CR program.
Functional Outcomes
The clusters of codes related to the participants’ experiences of the outcome of therapy on functioning were described as follows: feeling more in control, new communication skills, new problem-solving skills, ability to focus, healthy lifestyle, and self-confidence (
Table 1). All participants described functional improvements, regardless of whether they received CR. The participants described improvements in interpersonal, intrapersonal (sense of self), occupational, and cognitive functioning.
Therapy Process
The clusters of codes related to the participants’ experiences of the process of therapy were described as follows: expertise and support, encouragement to practice, and time to get to know me (
Table 2). Although most participants completed the CR if they had been randomly assigned to it, four participants did not complete it. Only two of these participants provided negative responses: “too hard at the time” and “I was never good at doing homework” (ERS024, woman with bipolar I disorder); “games were too easy” (ERS019, woman with bipolar II disorder).
Once the clusters were identified, we further analyzed the data informing the codes. Four themes were identified: hearing oneself and being heard, support to put therapy into practice, gaining a sense of achievement and hope for the future, and trusting the therapist’s expertise.
Hearing Oneself and Being Heard.
This theme captured participant descriptions of learning to talk about feelings and thoughts to someone who took the time to understand and who had the expertise to respond by identifying patterns and providing strategies with which the participant could experiment. Participants identified this theme as the key to their engagement in therapy and the basis on which they could undertake new behaviors.
One participant described how the process of talking helped him clarify his thoughts. Sharing his thoughts with someone who listened and had the expertise to respond was important:
Therapy has helped with my thinking. Having someone to talk problems out to. I was hearing what I was saying, and I was deciphering the problems myself. Hearing the problems spoken made them seem not as bad or made more sense why I feel that way. Saying it to someone who is hearing it and can give some feedback was important. While you’re talking, you are discovering what you focus on and learn new tools to change perspectives and approach things in a different way. (ERS44, man, age 31, treated with IPSRT for major depressive disorder)
Many participants acknowledged the importance of being supported to talk:
[The therapist] let me talk about stuff I have never talked to anybody about. To be able talk about some of this stuff was a huge gift. (ERS02, woman, age 44, treated with IPSRT for major depressive disorder)
The process of talking enabled the participants to become aware of what was normal for them and of symptoms of their disorder:
Talking about what is happening and noticing patterns has been really helpful. I used to keep inside my shell. I am now able to talk about it and express my feelings. Having someone to work out with me what is normal for me and not a symptom was really helpful. (ERS20, woman, age 23, treated with IPSRT for bipolar I disorder)
This theme, hearing oneself and being heard, described the process participants went through in engaging in therapy. Therapy provided a venue to articulate and receive feedback about issues and feelings that patients had previously internalized.
Support to Put Therapy into Practice.
This theme refers to the skills participants identified as helping them to manage their moods and improve their functioning: routines, communication skills, pattern identification, and problem-solving skills. They described how learning to integrate these skills into their daily lives had a marked effect on their moods, functioning, and sense of control.
All participants identified the importance of maintaining regular social rhythms as a key skill that they had developed in therapy:
Therapy has been a learning curve. In the past, I was told I had bipolar disorder, and they gave me medication and sent me out the door. They told me nothing about how to recognize the signs but [the therapist] helped me—get sleeping right, getting eating right, and I followed it strictly and followed advice about getting plenty of sunshine. I put into practice all these things. (ERS14, man, age 55, treated with IPSRT for bipolar II disorder)
Participants attributed improved communication skills as key to improvements in functioning, particularly in relationships:
Therapy has definitely helped in my relationships. I always used to struggle in relationships, but I understand how I act now, so I can try [to] shift things a bit. (ERS04, woman, age 29, treated with ISPSRT+CR for bipolar I disorder)
The CR aspect of therapy was helpful for some participants in improving their attention and perseverance:
I enjoyed [CR]. Some of it was challenging, and that was frustrating, but others I connected with and enjoyed. It was good for the brain and helped with my focus. You did have to concentrate. I could still do the games even when low. It required discipline to do each day, but that was good. I felt annoyed when I couldn’t do some of the games. I thought “am I just stupid,” but I persevered and then I felt pleased with myself. (ERS07, woman, age 55, treated with IPSRT+CR for bipolar I disorder)
Participants described the improvement in focus as helping them to become more organized in their daily lives by encouraging more organized thinking:
I feel much better now. I think the therapy helped with that. I can get everything done at home. I can organize my thoughts. I can schedule things. I now organize my days and do things in an orderly manner, and I get things done. Therapy has also helped my memory; the talking has helped me get my thoughts organized. It has definitely helped with my organization—doing things in order. I can really focus now. (ERS19, woman, age 23, treated with IPSRT for bipolar I disorder)
The development of problem-solving skills supported this improvement in organizational skills:
The therapy has helped my thinking. I don’t forget as many things as I used to. I can remember my way through the steps in a process better than I used to. (ERS18, man, age 36, treated with IPSRT for major depressive disorder)
The participants found that the therapy did not just involve talking and being heard, but it also provided them with support to practically apply what they had discussed in sessions. They all noted that the therapy gave them practical strategies to manage their moods.
Gaining a Sense of Achievement and Hope for the Future.
This theme refers to how the participants described having a sense of achievement at the end of the intervention. This sense of having mastered the therapeutic strategies engendered a sense of hope for the future and about their ability to self-manage. This theme also refers to development of understanding of what having a mood disorder meant for them and the unique ways it manifested at a personal level.
Understanding their patterns associated with mood and how to manage them gave participants hope for the future. Therapy provided participants with a framework for understanding symptoms that were sometimes incomprehensible to them. Many participants said that having a framework of understanding took away the sense of blame, deficiency, and defectiveness:
I feel that things make sense now. I feel much better about myself now. (ERS02, woman, age 44, treated with IPSRT+CR for bipolar II disorder)
This sentiment was echoed by a participant who identified the impact the therapy had on her family as well:
The study was life-saving—not just me but my whole family. It helped my husband and I to understand what was happening and how we could manage it. (ERS09, woman, age 31, treated with IPSRT+CR for bipolar II disorder)
The participants described how a critical aspect in improving functioning involved being able to put the strategies discussed in therapy sessions, particularly the strategies for stabilizing social rhythms, into practice in their everyday lives.
Trusting the Therapist’s Expertise.
This theme refers to the participants’ appreciation for the level of expertise and support that was provided by the therapists. The participants described the initial challenge of both trusting the therapist and trying new skills; however, all described how they valued this process of working together for their benefit.
Many participants identified the process of engagement and the duration of the intervention as very important in helping them develop trust in both the therapist and the model of therapy:
It was important having someone that knows you in depth. I had done some counseling, but I never found that useful. The length of time was really good because I knew I had the time to explore what I needed to do. I felt an obligation to continue—an obligation to others—to help others (being part of a research study). I wasn’t that good at helping myself. The therapy had a structure that felt more sincere than just talk. (ERS15, man, age 31, treated with IPSRT for major depressive disorder)
Participants described how the therapy put their symptoms into perspective, and for many, that meant realizing that their mood disorder symptoms were not part of their personality:
You need to be very comfortable with the therapist because you are so vulnerable. [The therapist] made me feel normal and interesting and welcomed. Before I came to therapy, I thought I was some sort of freak. (ERS02, woman, age 44, treated with IPSRT+CR for bipolar disorder)
The therapeutic process took time, and the process of engaging in therapy and the duration of therapy were important because they enabled participants to develop a commitment to the model:
In the beginning, I felt embarrassed and ashamed about being depressed. I think having therapy gave me some accountability. Sometimes I wanted to avoid doing it, but I didn’t want to let [the therapist] down. Having someone to be accountable to was important; if I had been doing things on [my] own, I might have let things slide more. It was challenging but in a good way. It made me aware that you can get better, and so when my mood slips, I have not been as hopeless. I have learned to manage things a lot better. It helped me identify that there were alternatives to the way I was living. (ERS08, man, age 29, treated with IPSRT+CR for major depressive disorder)
Many participants found therapy challenging in the early stages, and some described taking a couple of months to engage fully:
Initially [I] thought, how is this going to help me? And I have had lots of previous therapy and counseling. It took me a few months to get rapport with [the therapist] and to understand where it was all going and then it started clicking into place. (ERS16, woman, age 52, treated with IPSRT+CR for bipolar II disorder)
Most participants described the intervention as a challenge that required them to take responsibility to self-manage their moods. To be able to do this, they needed a therapist who was an expert in understanding the person and their mood disorder and in conveying strategies for managing mood disorders that engendered trust in the relationship. The participants described the therapy as an active process, with both parties working together.
Discussion
At the completion of the 12-month intervention, all participants in the study reported that both IPSRT and IPSRT+CR as an adjunct to medication had been effective in improving their functioning across a range of domains (interpersonal, occupational, and cognitive). The therapy was understood as a bidirectional process that involved the development of a sense of self that was more in control, more confident, and more able to focus, problem solve, and communicate effectively, which enabled the participants to undertake activities that led to functional improvements. As participants tried out their new skills and were able to master them, it reinforced their sense of self as being more in control of their lives and thus more confident. To our knowledge, this is the first study to examine participants’ perceptions of improvements in functioning, in the context of bipolar disorder and major depressive disorder, and of what they believed facilitated these improvements.
Some of the therapy characteristics identified by participants as most helpful (social rhythm management, a focus on interpersonal relationships, and CR) were specific to this intervention. Alongside these characteristics were common factors related to effective psychotherapy more generally (being heard, understood, and supported and receiving practical strategies, psychoeducation, and a framework of understanding that instilled hope).
Ensuring that the voices of people with mood disorders are heard is important for both clinical practice and research. Previous research suggests that people with bipolar disorder want treatment in which the clinician listens to and understands their individual needs (
29). A review of the literature on the experiences of bipolar disorder (
30) identified that people with this disorder are distressed by its associated losses in control, autonomy, work, sense of purpose, social connection, sense of identity, and functioning. This sense of loss has also been reported as a specific aspect of impairment in occupational functioning (
31). Our study found that a 1-year intervention of IPSRT (with or without CR) provided participants with the opportunity not only to regain some of these losses but to develop a healthier sense of self, which could help them tackle their functional challenges.
The literature on what patients with mood disorders experience as important is minimal (
32,
33). It appears that a proportion of these patients find the traditional medication model lacking. Patients have reported that they want treatment that helps them feel empowered and in control of their moods and other aspects of their lives; however, many have found this outcome may not occur in a one-size-fits-all approach to therapy (
34). As a previous study found (
35), these were patients who had experienced a crisis point in their lives for which medication was only partially effective; they were motivated to learn new skills.
This study had some limitations. First, the study’s interpretations reflect the perspectives of the research team. Second, because participants had been engaged in 12 months of psychotherapy, those who were dissatisfied may have dropped out (N=3). Third, the sample was not necessarily representative of all patients with recurrent mood disorders. In addition, the participants chose to take part in a psychotherapy study, and thus may not have been representative of a more general sample.
Conclusions
The participants of this qualitative study, all of whom had recurrent mood disorders, described experiencing improved functioning as a result of the intervention. It may be useful for people with mood disorders to take part in therapies, such as IPSRT with or without CR, that formulate their mood disorder in terms of a model that provides an understandable and evidence-based rationale, facilitates a sense of control and confidence by encouraging practical routines that can be integrated into daily life, focuses on practical communication and problem-solving skills, and engenders a sense of hope by offering self-management strategies relevant to their specific symptom experiences and to the life they choose to live.
Acknowledgments
The authors acknowledge Andi Bartram (data management), Bridget Kimber (clinical research coordinator), and Rachel Day-Brown (clinical research nurse) for their contributions to this work.