On March 30, 2020, the World Health Organization (
1,
2) declared COVID-19, caused by the SARS-CoV-2 virus, to be a worldwide pandemic. The new coronavirus, detected in December 2019 in Wuhan, China, caused flu-like symptoms, such as fever, shortness of breath, and cough (
3). Because of its high transmissibility and spread, most countries and populations quickly adopted measures to contain the virus, which largely focused on self-imposed and/or mandatory quarantines and shutdowns of major services and places (
4). Although these measures were viewed as necessary to control the virus’s spread, potential impact on individuals’ mental health soon became of interest and concern to health organizations (
2). As has been discussed in the literature (
2), individuals may develop a wide range of psychiatric symptomatology (e.g., anxiety, panic attacks, sleep disturbances, and posttraumatic stress disorder) as a consequence of infectious disease outbreaks.
Other life changes resulting directly from lockdown measures introduced several factors that may have facilitated the experience of anxiety—characterized by feelings of tension, apprehension, and worry—and physiological changes, such as sweating, dizziness, and increased blood pressure and heartbeat. In particular, factors such as uncertainty about the future, economic sanctions, mortality statistics, media exposure, lack of a vaccine, risk of unemployment, and difficulties in eradicating the virus may have caused anxiety symptoms (
5,
6). Several authors (
4,
6–
11) have expressed concerns about COVID-19 lockdown and quarantine causing anxiety, depression, panic, loneliness, stress, difficulty concentrating, and desperation.
According to the health belief model (HBM), beliefs about the severity of an illness tend to significantly affect how individuals perceive and experience different aspects of the illness (
12). Thus, perceived susceptibility, severity, and threat of the illness may mediate or modify individuals’ behaviors (
12,
13). In this sense, beliefs about health conditions are predicted to play a major role in how individuals react to pandemic situations and may influence individuals’ experiences and behaviors. However, to date, there is a scarcity of work exploring perceptions about COVID-19 severity (i.e., beliefs about the seriousness and the dangerousness of being infected by SARS-CoV-2 and developing COVID-19).
To address these issues, we aimed to develop a brief inventory of perceptions about COVID-19 that focused on two major domains: anxiety about COVID-19 and beliefs about the disease’s severity. This questionnaire was based on aspects of the HBM regarding perception of threat, susceptibility, and severity of an illness. We also explored potential associations of these domains with scores on mental health indexes measuring psychological distress and well-being as well as symptomatology.
Specifically, our three hypotheses were as follows: perceptions about COVID-19 would be correlated with psychological distress and well-being (hypothesis 1), would be correlated with psychopathological symptoms (hypothesis 2), and would mediate the relationship between symptomatology and mental health (hypothesis 3).
Methods
Participants and Procedures
Participants were tested individually (April 20 to May 20, 2020), with a 4-day maximum to complete the research protocol. Participants were recruited online via social media (e.g., Facebook, LinkedIn), where they completed a battery of three questionnaires hosted in the Qualtrics platform.
Exclusion criteria were age <18 and having a major neurocognitive disorder diagnosis. All participants gave informed consent, and no compensation was provided for participation. This research was approved by the ethics committee of the Faculty of Psychology, University of Lisbon.
Measures
COVID-19 Inventory.
The COVID-19 Inventory was developed in Portuguese and was based on the theoretical underpinnings of the Health Belief Model. The inventory measures respondents’ beliefs regarding COVID-19. The initial pool of items consisted of 20 items that covered dimensions of the respondents’ beliefs about the severity of COVID-19 and the intensity of their anxiety. After designing the inventory’s conceptual structure, we asked two independent judges to screen the pool of items for face validity, providing them with a category dictionary for use in matching each item in each category. A 5-point Likert scale was used to rate the intensity of the respondents’ experiences. Before presentation to the public, we pilot tested the inventory with 10 randomly selected individuals with no knowledge of the measure to test for vocabulary and construct comprehension. We then released the instrument online to the general population.
Mental Health Inventory.
Mental health was assessed by using the Portuguese version (
14) of the Mental Health Inventory. This version measures general psychological well-being and distress on a 5-item Likert scale. This self-report instrument is used to quickly screen distress and well-being as indexes of mental health. Higher scores represent higher levels of the variables (distress and well-being). Total scale Cronbach’s alpha was excellent at α=0.92 (α=0.90 for psychological distress and α=0.87 for well-being).
Brief Symptom Inventory–53 (BSI-53).
To assess symptomatology, the Portuguese version of the BSI-53 (
15) was used. This 53-item self-report inventory uses a 5-item Likert scale (0 to 4) to assess several psychopathological symptoms, including paranoid ideation, somatization, phobic anxiety, and anxiety. Higher scores represent higher levels of symptomatology. In the present investigation, internal consistency for the General Severity Index (GSI) was considered very high (α=0.94) and ranged from medium (α=0.77, paranoid ideation) to high (α=0.92 phobic anxiety) in the subscales.
Statistical Analyses
Descriptive statistics were used for sample characterization. Normal distribution was assumed (N>30). To explore associations between variables, we used the Pearson product-moment correlation coefficient. For mediation analysis, the macro process for SPSS (
16) was used. A bootstrapping procedure was used to calculate the 95% confidence intervals of the mediation coefficient. A mediation was considered significant when the intervals did not contain the zero value. Statistical analyses were performed in SPSS Statistics, version 24.
Results
Sociodemographic characteristics of the participants are provided (
Table 1). We used exploratory factor analysis to examine the factorial structure of the COVID-19 Inventory. Factors with eigenvalues higher than 1 were extracted, and varimax rotation was performed. Two factors were extracted that explained 69% of the total variance. Items loading below 0.50 were removed. Factor 1, called COVID-19 anxiety, explained 55% of the variance; factor 2, called COVID-19 severity, accounted for 14% of the variance (
Table 2). The solution converged in nine interactions. The Kaiser-Meyer-Olkin measure was 0.872, revealing good correlations between variables (
17). The Bartlett sphericity (BS) test was also statistically significant (BS=706,801, p<0.001), revealing appropriate associations between variables (
17). Cronbach’s alpha for COVID-19 anxiety (factor 1) was 0.85 and for COVID-19 severity (factor 2) was 0.80. Both alphas were considered acceptable.
COVID-19 anxiety was positively correlated with COVID-19 severity (r=0.59, p<0.05), GSI score (r=0.19, p<0.05), and psychological distress (r=0.24, p<0.05). COVID-19 anxiety was negatively correlated with psychological well-being (r=–0.22, p<0.05). GSI scores were positively correlated with psychological distress (r=0.78, p<0.05) and negatively correlated with psychological well-being (r=–0.77, p<0.05). COVID-19 anxiety was positively correlated with somatization (r=0.21, p<0.05), anxiety (r=0.23, p<0.05), phobic anxiety (r=0.37, p<0.05), and paranoid ideation (r=0.16, p<0.05). Perceived severity of the COVID-19 illness did not correlate with scores on the GSI (
Table 3).
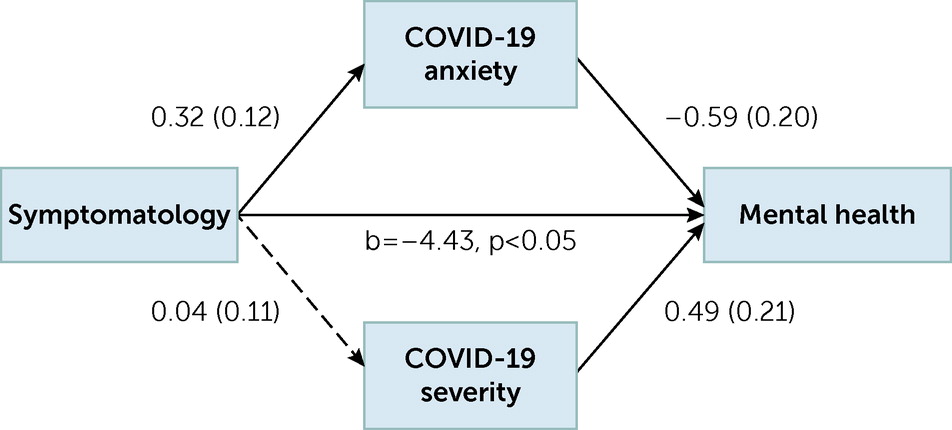
A composite mediation model was tested with two mediators: COVID-19 anxiety and severity. Ninety-five percent confidence intervals and 10,000 bootstrap computations were used. The model was partially confirmed. COVID-19 anxiety (−0.3938, −0.0158, p<0.05) mediated the relationship between GSI score and mental health, whereas perceived severity of the illness (−0.1067, 0.1510, p>0.05) did not (
Figure 1).
Discussion
The relationships between COVID-19 perceptions, scores on mental health indexes, and symptomatology (as measured by the GSI) were explored. Some considerations related to these preliminary results are highlighted below.
Our first hypothesis was partially confirmed. COVID-19 anxiety was associated with psychological distress and well-being, which is in line with previous assumptions (
6). Several factors, such as media exposure, catastrophic news, lack of a vaccine, and future uncertainty, may contribute to increased anxiety related to COVID-19 and may lead to higher distress levels and lower psychological well-being (
4,
5,
7,
8). However, perceived COVID-19 severity did not correlate with distress and well-being. One likely explanation for this result may be that the rapid development of pandemic situations, may cause individuals to respond primarily in an emotional way. Another explanation may be related to our new questionnaire, which has not undergone a detailed psychometric study. However, because of the lack of measures to assess anxiety about COVID-19, it was essential to develop one. Moreover, these are preliminary data, which means that results may vary with a different sample size.
Anxiety about COVID-19 was associated with somatization, anxiety, phobic anxiety, and paranoid ideation (partial confirmation of hypothesis 2). However, as in the case of hypothesis 1, perceived severity of COVID-19 did not correlate with scores on the GSI. One likely explanation may be that perceptions about a disease’s severity may not correspond with psychiatric symptomatology. Individuals may hold several beliefs that do not represent their actual emotional state. Another likely explanation may be that perceived severity of the disease may play a mediating role in general mental health. This possibility is described further below.
We expected that COVID-19 anxiety might be associated with other forms of anxiety, especially phobic anxiety, because of its relation to fear and tension regarding contamination. We also expected that COVID-19 anxiety would be associated with somatizations, because of the physical aspects of anxiety. It is also understandable that COVID-19 anxiety may be associated with paranoid ideation. Systematic exposure to catastrophic events through the media, as previously described, may evoke thoughts of danger and feelings of mistrust, which is in line with previous assumptions (
5).
Finally, only anxiety about COVID-19 mediated the relationship between mental health and GSI score (partial confirmation of hypothesis 3). These results support the previous assumption regarding COVID-19 anxiety as a significant predictor of mental health (
5) and are aligned with the theoretical assumptions of the HBM (
12). Perceived severity of COVID-19 did not mediate the relationship between symptomatology and mental health. However, in the model, this variable predicted the variance in mental health which demonstrated the complexity between cognitions, symptomatology, and mental health: anxiety about COVID-19 seemed to be directly associated with symptomatology, whereas perceived severity of the disease seemed to be more related to general mental health. In this sense, perceived severity of the disease also seemed to play a role in mental health, which means that beliefs regarding COVID-19 severity may also be targets for psychological intervention. Severity perception may be influenced by a country's culture. It is important to explore perceptions of COVID-19 in other countries to determine whether they match our results. These results may help clinicians find better ways to assess and conceptualize anxiety about COVID-19 and perceived severity of the disease, which can then be addressed through telepsychiatry (because of confinement measures) (
18).
Despite its strengths, this study had several limitations. This study was conducted online and used a cross-sectional design, which may have limited some causal explanations about the variables under study. Another limitation may have been the use of self-report measures, which are limited by individuals’ self-awareness. The lack of preexisting standardized measure to assess perceptions about COVID-19 was also a limitation. Moreover, the sample size was small, which limited generalization and statistical power.
Conclusions
COVID-19 anxiety and perceptions about the disease’s severity may have pervasive impacts on individuals’ mental health index scores, including the GSI and other measures of psychological distress and well-being. These preliminary results may add to the limited literature on the impacts of the COVID-19 pandemic on mental health and may inform psychotherapists regarding case conceptualization and clinical decision making.