The empirical development of a psychotherapy for a specific patient population is a multifaceted project. Such a process involves conceptualization of the pathology and approach to treatment, a written document (i.e., a manual) that describes the treatment in detail, preliminary data on the potential impact of the treatment, randomized controlled trials (RCTs), investigation of moderators and mediators, and generalization of the treatment to diverse settings and patients (
1). In this article, we review research findings on the development of a psychoanalytic treatment for personality pathology called transference-focused psychotherapy (TFP) over approximately 40 years of empirical exploration. The research efforts highlighted here were accomplished under the leadership and inspiration of Otto F. Kernberg with colleagues at Weill Medical College in New York City and abroad.
First, we briefly review the development and manualization of TFP and the empirical evaluation of its efficacy. Rather than focus solely on outcomes, we discuss efforts to evaluate TFP’s process and mechanism of change (i.e., that patients change in ways consistent with the hypothesized model and that those changes are linked to TFP-specific interventions). Second, we discuss Kernberg’s object relations model of personality and its implications for assessment and diagnosis of personality disorders. Last, we examine functional implications for patients of borderline personality organization (BPO) with a model that integrates the patient’s interpersonal functioning, object relations, and self-regulatory functioning, including preliminary findings and future directions for research evaluating personality dysfunction and its treatment.
Empirical Investigation of TFP
The treatment of borderline personality disorder has been dominated by a focus on development of coping skills with cognitive-behavioral therapy (CBT) (
2). A major question has been whether a complex psychodynamic treatment, in contrast with a very specific CBT-based skills approach, could be articulated in a manual and be reliably delivered by therapists trained in the process.
Many decades ago, a few senior psychiatrists under Kernberg’s leadership video-recorded their psychotherapy sessions with the goal of generating principles of intervention, which led to the first published manual describing the strategies, tactics, and techniques of TFP (
3). In contrast with treatment manuals that describe a set pattern of techniques and foci of an intervention applied uniformly to all patients, the TFP manual is principle driven, providing the therapist with not only a structure for the primary targets of intervention but also flexibility in how to relate to each unique patient.
TFP was originally articulated as an intensive individual treatment for adults with the categorical diagnosis of borderline personality disorder. However, as research and treatment experience have accumulated, TFP has been refined and extended to a wide range of patients with a personality disorder (
4,
5), with treatment focused on the common problems related to self-functioning and functioning with others.
Evaluating TFP Outcomes
The articulation of TFP in a principle-driven manual enabled the first test of the hypothesized safe and effective TFP treatment for female patients with borderline personality disorder, which was funded by an NIMH treatment development grant (MH51348-01; principal investigator: J.F.C.). In that study of a 1-year TFP treatment, which included 10 patients diagnosed as having borderline personality disorder who served as their own controls, the treatment was well received by the patients, the dropout rate was low (19.1%), and none of the patients experienced a deterioration of measurable symptoms or were adversely affected by the treatment (
6). Compared with the year before treatment, patients experienced significantly fewer psychiatric hospitalizations, fewer days of inpatient hospitalization, and a reduction in the number of suicide attempts. These results suggested that TFP was effective in lowering health care costs incurred by emergency department visits and hospitalizations.
This initial demonstration of the safety and efficacy of TFP was succeeded by an RCT of a 1-year TFP treatment that was compared with a supportive psychodynamic treatment (SPT) and with dialectical behavior therapy (DBT) (
7). Individual growth curve analysis was used to investigate changes in symptoms and domains of functioning over time for each of the 90 female patients diagnosed as having borderline personality disorder and for each treatment group. All three treatment approaches showed significant changes across multiple domains of functioning. However, only TFP and DBT were associated with improvement in suicidality, and only TFP was significantly associated with improvements in impulsivity, irritability, and verbal and direct assault. TFP was also uniquely associated with reduction of aggression. Subsequent research demonstrated that pretreatment patient characteristics differentially predicted changes in aggressive dyscontrol, anxiety and depression, impulsivity, and global functioning (
8). A review detailing this RCT’s (
7) procedures and results can be found elsewhere (
9).
To evaluate the effectiveness of TFP in a cultural setting different from that of the original study in New York, in a two-site RCT conducted in Europe, 104 female patients diagnosed as having borderline personality disorder were randomly assigned to receive 1 year of either TFP or treatment by community therapists who were experienced in the treatment of personality disorders (
10). Patients treated with TFP, compared with those receiving treatment by community therapists, showed significantly greater reductions in borderline personality disorder criteria met, suicide attempts, and hospitalizations. Furthermore, improvement in social and personality functioning was superior in the TFP group. Because the comparison treatment was conducted by highly experienced therapists in the community, the authors concluded that the specific mechanisms of TFP were associated with greater improvement for patients.
These studies demonstrate the efficacy of TFP, and their specificity points to future directions in outcomes research. To date, clinical trials of TFP have evaluated women diagnosed as having borderline personality disorder. Although reducing heterogeneity was essential in initial RCTs, future research should seek to demonstrate the therapy’s efficacy for patients with varying genders, cultures, ages, and diagnoses. Recent developments in the treatment model for patients with narcissistic personality disorder (
5) and adolescents with severe personality disorder features (
11) have broadened the reach of TFP. Furthermore, whereas clinical trials have evaluated individualized TFP, the treatment’s application in broader psychiatric and medical group settings (
12) should be a focus of future research.
Evaluating TFP Processes
Whereas RCTs are considered the gold standard to demonstrate the relative efficacy of the psychotherapy in question, our clinical research group has been interested in equally important questions concerning treatment process and mechanism of change. The hypothesized mechanism of change in TFP that affects borderline personality disorder is increased affect regulation, achieved through mentalization (i.e., the growing ability of the patient to put momentary affect arousal, especially in social interactions, into a more benign and broader contextual understanding of self and others) (
13).
Each of the aforementioned RCTs examined characteristics beyond the symptoms of borderline personality disorder to evaluate changes in attachment style and reflective functioning. Patients receiving TFP were significantly more likely to move from an insecure to a secure attachment style and to have increased capacity for mentalization (reflective functioning) after 1 year of treatment, compared with patients receiving the other therapies (
14). These results, although preliminary, shed light on the specific efficacy of TFP via a mechanism of change in which positive personality traits and interpersonal functioning are enhanced through greater mentalization and attachment security.
The fact that TFP is associated with increases in reflective functioning has led researchers to study how this effect is accomplished in the therapeutic process. In a study comparing the use of different treatment approaches (
15), adherence to the principles of prototypical TFP and interventions that enhance mentalization was highest among TFP therapists, relative to those who used SPT and DBT. Higher adherence to TFP principles predicted larger reductions in verbal assault and increases in reflective functioning only with TFP, and lower adherence predicted larger reductions in direct assault with SPT. The fact that adherence to prototypical TFP interventions predicted better outcomes supports the treatment’s model of change.
The therapeutic process of TFP was further evaluated in early-, middle-, and late-phase videotaped sessions of TFP and compared with the processes of DBT and SPT. Therapy sessions were divided into therapist and patient speaking segments (
16), which were rated in terms of invitations or opportunities for patients to reflect on their mental state (i.e., bids for reflective functioning) and were coded for patients’ arousal on the basis of acoustic indicators. Across treatments, therapists’ invitations for patients’ reflection predicted improved posttreatment reflective functioning, which in turn predicted lower emotional arousal. Invitations for reflection were twice as common with TFP than with DBT or SPT. These findings suggest that asking patients to reflect on their mental states has a down-regulatory effect on patients’ arousal when engaged in psychotherapies for borderline personality disorder. Capacity for reflection may be more central in the processes and outcomes of TFP than in the processes and outcomes of other treatments for borderline personality disorder. Below, we detail a model that integrates neurocognitive and self-regulation research to describe the mechanisms by which TFP enhances the capacity to mentalize.
Advances in Models of Personality Dysfunction
The object relations model of personality organization (
17) has traditionally contrasted with the descriptive approach of the
DSM-5 (
18), which differentiates personality disorders by manifest type rather than by underlying psychological structure. Central to how people experience personality is the organization of their internal representations. During childhood, with maturation of cognitive and affective systems, individuals experience an increase in differentiation, integration, and hierarchical organization of representations of self and others. When consolidated in a stable identity, perceptions of oneself and the capacity for relatedness with others are balanced and emotionally integrated. In contrast, manifest symptoms of borderline personality disorder (i.e., affective, interpersonal, and behavioral instability) arise from poorly integrated representations corresponding with unstable affects and polarized perceptions of self and others (
18).
Based on Kernberg’s extensive clinical experience, the specificity of the model lays the groundwork for assessing the relevance of conceptions of personality pathology rooted in object relations and for direct comparison with other current conceptualizations of personality and its pathologies (
19). This model has found recent influence in the Alternative DSM-5 Model for Personality Disorders, in section III of
DSM-5, with its emphasis on self-functioning and functioning with others (see Caligor et al. [
19] in this issue). A direct line can be drawn from an object relations model of personality organization to a model of treatment. TFP leads to symptom change through a focus on the patient’s identity functioning and relatedness as manifested in the therapeutic interaction (
20,
21).
The object relations model has direct implications for patient assessment, which has led to the development of self-report questionnaires (
22) and semistructured interviews to assess personality organization (
23,
24). However, borderline personality pathology is unique in its “stable instability.” The possibility for enormous variability in function (that can change by the minute, hour, or day) cannot be adequately captured by questionnaires and semistructured interviews. Yet, impairments in self-functioning and interpersonal functioning remain generally consistent throughout adulthood (
25).
Because the unstable aspects of borderline pathology may not be adequately captured via cross-sectional self-report data, our research group has used laboratory assessment of personality functioning (e.g., fear vs. trust, rejection sensitivity) and electronic diary studies of the flow of and variation in patients’ daily lives. Experience-sampling methods represent advances over self-report methods, which are susceptible to memory bias, in that participants are asked to provide brief but immediate ratings after specific events or random prompts at specified intervals. Such methods allow researchers to move away from aggregate ratings of a given behavioral or emotional experience to evaluate intraindividual variability. Ratings of the perceptions of others’ behaviors, the perception of one’s response, and the associated affects may provide a simple construction of a self-other dyad. However, when the participant’s experience in specific contexts on specific days is intensively sampled by using daily diary methods, the setting of specific representations of self and others and related affect begins to emerge (
26,
27).
The Specifics of Conflicted Interpersonal Interactions
Object relations theory postulates that representations of self and others that are characterized by negative affect, aggression, and splitting lead to both a tendency to reject others and a co-occurring perception of being rejected by others. How the internal experience of rejecting and being rejected manifests itself in interpersonal behavior depends in part on the level of a person’s effortful control. Effortful control represents the “voluntary” aspect of temperament that allows individuals to successfully resolve conflicts between immediate reactive tendencies and long-term demands and to overcome a dominant response to produce a more appropriate, valued, and goal-directed nondominant response (
28).
The interpersonal and object relations dynamics that characterize individuals with BPO may be understood within the framework of current theories and empirical evidence on how individuals self-regulate when experiencing a relational conflict (
29). According to cybernetic models of self-regulation, conflict emerges when a discrepancy is detected between one’s goal or desired state and the actual behavior in a particular context (
30). This potential mismatch leads to negative affect (i.e., anxiety, frustration) and to a cascade of neurophysiological responses signaling alarm, including the activation of the anterior cingulate cortex (ACC) and of fight-or-flight responses fostered by the autonomic nervous system (ANS). Importantly, this aversive nature of conflict signals to the individual the need to reprioritize his or her own valued goals and pursue additional goal-directed actions to decrease the mismatch between the individual’s desired state and the current one (
31). Therefore, self-regulation begins with conflict.
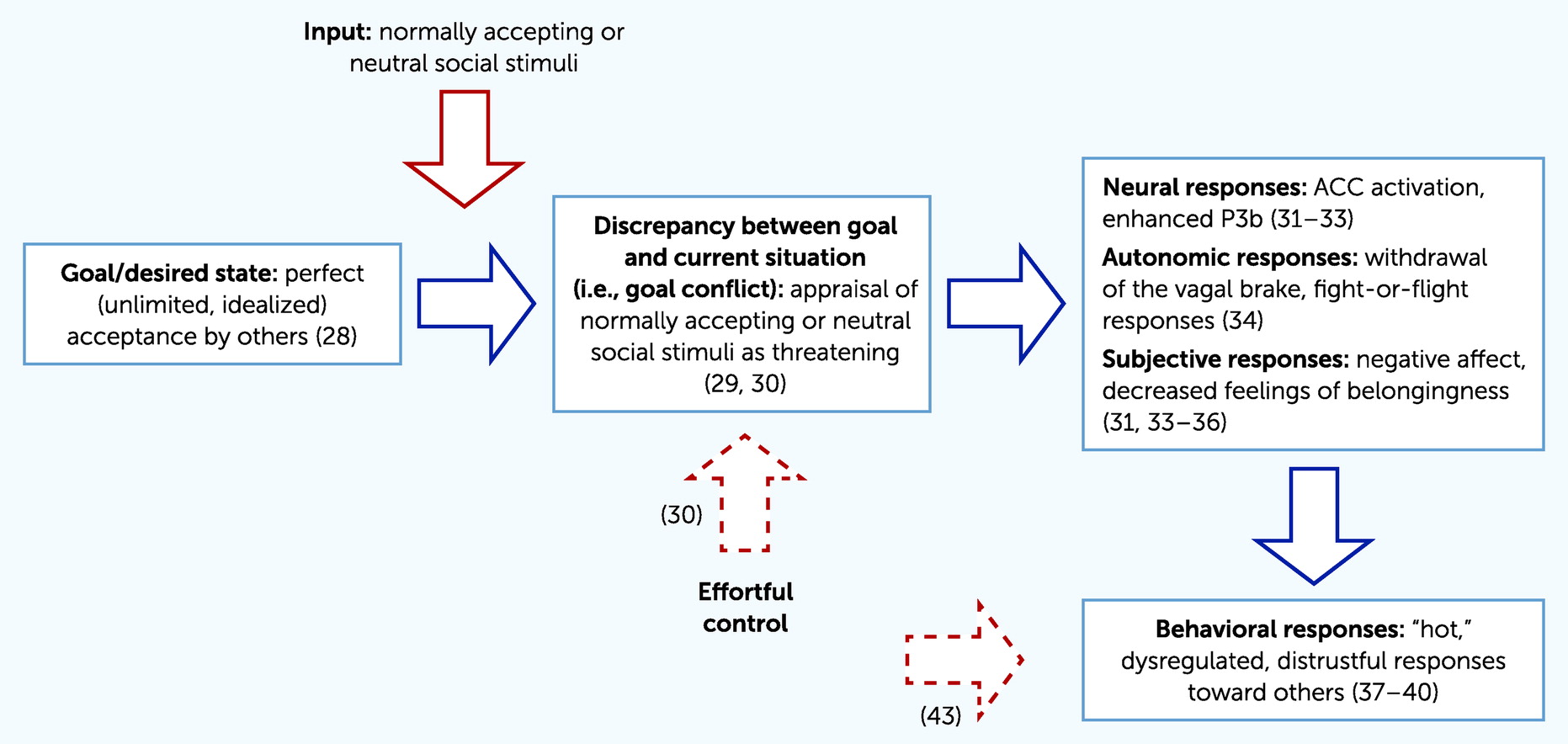
The intense negative affects experienced by patients with BPO may be conceptualized as a prolonged state of inner conflict that is not counterbalanced by the recruitment of successful self-regulatory abilities (
Figure 1). According to object relations theory (
17), patients with BPO exhibit an unconscious, idealized need to find a perfect relationship with a totally accepting and caring other. In a self-regulation view, this need represents the desired, although unconscious, state of patients with BPO (i.e., their motivating goal). In the desperate attempt to protect this unconscious hope for a perfect relationship, individuals with BPO need to project their own negative affect onto others, whom they thus consciously perceive to be malevolent and excluding, even when they are not. This constellation prevents patients with borderline personality disorder from accurately perceiving interpersonal exchanges. Any partner, even one who is benign or neutral toward the patient, may be perceived as threatening when he or she does not match the unconscious, split-off representation of an idealized, perfectly loving other.
Importantly, this appraisal of neutral or even accepting social stimuli as threatening, which is central to the conceptualization of BPO in object relations theory, has been well documented empirically. For instance, those with features of borderline personality disorder show a bias toward undernoticing trustworthiness in others (
32) and misinterpreting neutral facial expressions as negative (
33). Within a self-regulation framework, the resulting discrepancy between one’s own goal or desired inner state (i.e., being involved in a perfectly caring relationship) and the perception of the interpersonal environment (i.e., the biased appraisal of others as malevolent toward the self) generates a state of goal conflict that triggers a variety of neural, physiological, and subjective responses aimed at signaling the conflict and promoting resolution. For those with borderline personality disorder, this “alarm cascade” is activated even in the presence of objectively benign social stimuli.
At the neural and physiological levels, during social exchanges, patients with borderline personality disorder exhibit increased ACC activation, enhanced P3b event-related potential (
34–
36), and a withdrawal of the ANS vagal brake on the heart (
37). These findings indicate an inappropriate activation of the neural social pain circuitries and of fight-or-flight physiological states for those with borderline personality disorder during fair or even inclusive interpersonal exchanges that do not match the implicit, unconscious goal of finding perfect relatedness. This conflict is consistently associated with negative subjective reactions, such as increased negative emotions and feelings of social disconnection (
34,
36–
39). Usually, the aversive outcomes of conflict signal the need to increase self-regulation by activating goal-directed behavioral responses aimed at reducing the mismatch between one’s current and desired states (
31). However, increasing evidence also shows that this does not occur for those with borderline personality disorder, for whom the neural, physiological, and subjective responses to fair or inclusive social interactions are also associated with maladaptive behaviors. For instance, studies of behavioral economics indicate that patients with borderline personality disorder react to others’ fair and accepting behavior as if it were unfair, often by punishing them and exhibiting uncooperative, distrustful, and hostile attitudes (
40–
43). These findings are in line with object relations theory’s understanding of the relationship between the subjective experience of patients with BPO, who have a tendency to feel intense negative affect and to perceive a self rejected by untrustworthy others, and their observed behaviors, which show a tendency to act rejecting and mistrustful of others (
17). From a self-regulation perspective, this behavioral output is not effective in reducing the aversive experience of inner conflict; rather, it is likely to perpetuate conflict by enhancing the discrepancy between one’s own desired state of a perfect relationship and the real-world interpersonal context. In other words, a failure in self-regulation is at work.
Enhancing the ability of patients with borderline personality disorder to accurately reflect on their perception and their emotional and behavioral responses to interpersonal relationships is a fundamental and well-validated mechanism of change in TFP. In TFP, increased mentalization and reflective functioning abilities are critical to the promotion of patients’ understanding and improvement of their internal representations of self and others (
9,
44). The ability to self-regulate is closely related to such processes, as indicated by the association between executive attention and therapeutic alliance during therapy (
45). Distorted perceptions of others as malevolent and subsequent maladaptive responses may be reduced among patients with borderline personality disorder by the deployment of effective self-regulation strategies, as indicated by higher levels of effortful control. In fact, a high level of effortful control buffers the tendency to misinterpret neutral facial expressions as negative among those with severe features of borderline personality disorder (
33) and buffers negative behaviors related to perceptions of interpersonal rejection (
46). These findings support the clinical utility of focusing on patients’ self-regulation abilities, especially at times of intense negative affect, to foster reflective rather than reflexive patterns of social cognition. Specifically, increased self-regulation may reduce the prolonged state of inner conflict by promoting an accurate appraisal of positive social cues, an ability that appears to be impaired in people with borderline personality disorder. This appraisal will decrease the mismatch between patients’ motivating goal of establishing a positive relationship with others and their distorted perception that no positive relationship exists in reality, ultimately fostering the successful integration of their inner, conflicted, and partial representations of self and others.
Preliminary research evaluating changes in brain functioning after TFP treatment is supportive of this model (
47). In a pilot study, patients with borderline personality disorder (N=10) manifesting prominent affect dysregulation received TFP treatment and underwent functional magnetic resonance imaging (fMRI) assessment before treatment and after 1 year of treatment (
48). In a comparison of pretreatment and posttreatment fMRI scans, changes in brain functioning suggested that treatment with TFP was associated with relatively increased activation in the emotional and cognitive control areas of the brain and relatively decreased activation in areas of the brain associated with emotional reactivity and semantic-based memory retrieval.