Over the past 2 decades, there has been increasing recognition of the importance of well-being—the concept of how a person is doing overall—beyond absence or presence of illness and its symptoms. Different researchers and scholars have conceptualized well-being in various ways (
1–
4), but all agree that well-being encompasses more than the absence or presence of pathology and its symptoms. Some have conceptualized well-being as feeling subjectively good and functioning well, in spite of some symptoms, while maintaining a sense of purpose and being engaged in positive relationships (
4). Scholars have differentiated eudemonic from hedonic well-being. Hedonic well-being relates to feeling good, whereas eudemonic well-being has a broader definition, acknowledging that well-being does not require a person to feel good all the time. Eudemonic well-being encompasses having a sense of purpose as well as the degree to which a person is fully functioning in their life (
2) including in their work and in their relationships. Ryff (
1) has noted that key components of eudemonic well-being include self-acceptance, positive relationships with others, autonomy, environmental mastery, purpose in life, and personal growth.
Recognition of the importance of well-being has burgeoned in the literature on positive psychology but has been limited in clinical research and practice to date. Many short scales that are commonly used to assess patients’ experience of their illness symptoms and life situations focus on the symptoms of specific disorders. Examples include the Patient Health Questionnaire–9 (
5), the Generalized Anxiety Disorder–7 scale (
6), the Clinically Useful Depression Outcome Scale (
7), and the Clinically Useful Anxiety Outcome Scale (
8). Although measuring symptoms over time can be an important component of care, patients’ experience of themselves and their lives encompasses more than their symptoms. Clinicians who excessively focus on symptoms may miss important aspects of a patient’s experience and may set the stage for a narrow case formulation and treatment plan. Such a narrow focus often results in the sole use of symptom-focused interventions, either pharmacological or psychological, that may not address important environmental and psychosocial problems.
Need for an Ultrabrief Clinimetrically Guided Measure of Well-Being
For a measure of well-being to have broad clinical utility, it needs to be easily integrated into clinical practice without lengthening the clinical encounter or creating extra work after the encounter ends. Such a measure also needs to provide broad, pertinent information about a patient’s experience of their life that can inform clinical conversations between providers and patients. This focus on ease of use and clinical utility is consistent with a clinimetric approach. Clinimetrics is concerned with clinically relevant and useful scales that can be used to enhance clinical interactions (
9). As with traditional psychometrics, clinimetrics acknowledges the importance of forms of validity that can differentiate between different groups of people (e.g., patients vs. nonpatients) (
9).
Our goal was to create a very short, clinimetrically guided measure of eudemonic well-being that can be used in clinical settings with a wide variety of patients. We began the process of item development by considering areas of well-being identified in the literature, and then we held focus groups of patients and therapists to talk about self-identified important areas of life experience beyond pathology. The following areas were identified: overall satisfaction with quality of life, the ability to function by completing tasks, experience of emotional support in important relationships, and sense of purpose in life. We discuss the rationale for each area in turn.
Rationale for Each Dimension of Well-Being
According to the World Health Organization, disease burden is a measure of life lost because of either premature death or presence of a health condition that limits a person’s ability to function in occupational and social contexts. Research on disease burden demonstrates that disability is a major burden of illness (
10,
11). Disability encompasses many areas, but one key area is the ability to complete tasks at home, at work, in school, or in social situations. Asking about patients’ ability to complete tasks is one way to quickly assess functioning, regardless of whether patients are working for pay, enrolled in school, or engaged in not-for-pay caregiving or household management (
10–
12).
Another area that strongly affects overall health and wellness is the degree to which people feel that their lives are purposeful. There are some people who cannot work because of a disability but still feel a profound sense of purpose, whereas others who are able to work and complete tasks feel that their lives lack purpose. Having a sense of purpose in life is a marker of feeling that one is leading a meaningful life (
13). Consistent with this framework, McKnight and Kashdan (
14) have argued that the effort to set and achieve life goals is a renewable source of engagement and meaning for patients. Research has supported the health benefits of living with a sense of purpose (
15–
17).
Relationships have a profound impact on health and wellness. A wide body of research has demonstrated that supportive relationships promote health, ease adjustment to illness, and improve the trajectory of illness (
18–
26). Supportive family relationships have an impact on health equal to that of physiological risk factors such as cholesterol or high blood pressure (
24). The opposite is also true: relationships that are corrosive, judgmental, critical, or hostile have an adverse effect on health (
24). In a similar vein, time spent with others in satisfying relationships is associated with better mental health and general medical health (
26,
27). Research has also demonstrated that a patient’s most important resource is their family, because family relationships affect how patients navigate illness (
25). Although supportive relationships are health enhancing and corrosive relationships are health depleting, few providers routinely ask about satisfaction with relationships as a health-related variable.
We also wanted to gather information about patients’ overall satisfaction with their lives. Quality of life is a construct that was designed to be a composite of several different areas of life that gives a holistic picture of overall life satisfaction. Many studies of health and disease have used quality of life to get a sense of the degree to which people are satisfied with their lives, regardless of their symptom burden (
28–
33). Data on quality of life provide clinically useful information about the impact of illness on a patient and the potential need for additional treatment.
Study Aims
After we identified four central areas of eudemonic well-being, we developed an ultrabrief measure to assess them: the Brief Multidimensional Assessment Scale (BMAS). The aim of this study was to present the preliminary clinimetric and psychometric properties of the BMAS. Our team identified reliable and valid multi-item assessment scales to correlate with each dimension of patient experience included on the BMAS. We hypothesized that each BMAS item would demonstrate a moderately strong correlation with an established, reliable, and valid scale of the construct that it was designed to measure. We hypothesized that each BMAS item would also correlate moderately with all other BMAS items and that the BMAS items would demonstrate adequate internal consistency. To explore validity, we aimed to test whether BMAS scores reflected significantly more distress in clinical samples than in non–help-seeking samples.
Methods
The study sample consisted of 499 participants (250 women, 245 men, 4 nonbinary). Patients were recruited from several departments at a New England general hospital (N=412), and participants for the nonclinical sample were recruited from the community (N=87). The mean age of all participants was 45 years. Patients (18–85 years of age) from inpatient medical units, inpatient psychiatric units, an outpatient psychiatric clinic, and an outpatient medical clinic affiliated with the general hospital were asked to complete questionnaires if they were able to read and understand English and were not exhibiting florid psychotic symptoms. Patients completed the paper-and-pencil measures, described later, while they were in their rooms in an inpatient unit or while they were waiting for their appointment if they were recruited from an outpatient setting. We entered the data with REDCap. The study was approved by the institutional review board of Rhode Island Hospital, and participants signed informed-consent forms.
Using a snowball strategy, we collected data from a recruited nonclinical community sample (N=87) that comprised friends and family members of the current study’s research team. Participants in the nonclinical sample completed the measures online using REDCap.
Measures
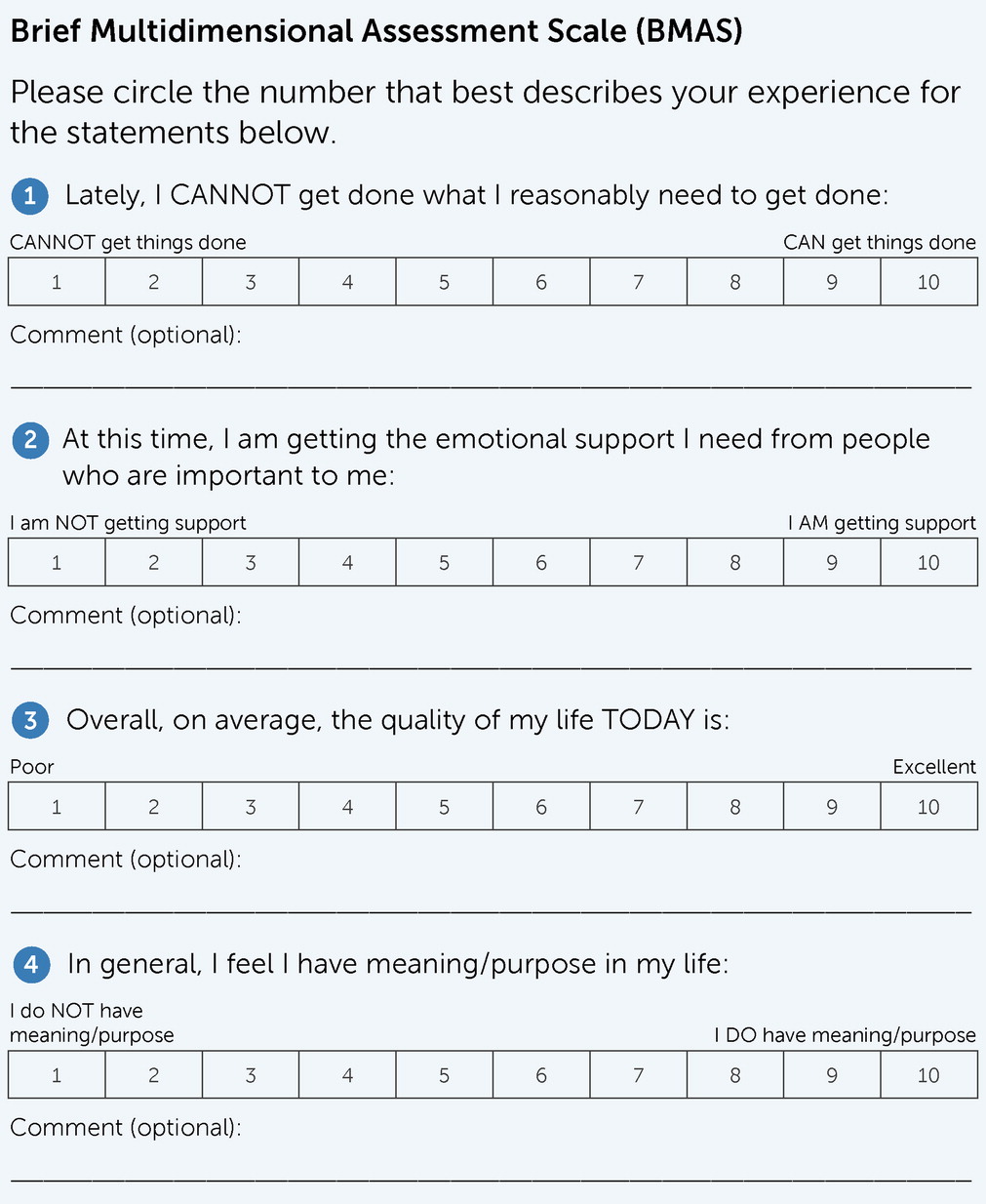
BMAS.
The BMAS is a four-item scale that was used to measure participants’ emotional support in important relationships, ability to get things done, sense of purpose in life, and quality of life. Each item’s response options range from 1 to 10 (higher scores indicate better well-being), as depicted in
Figure 1.
Multidimensional Scale of Perceived Social Support (MSPSS).
The 12-item MSPSS (
34) was used to measure participants’ perceived level of social support from family, friends, and significant others. Mean scores range from 1 (highest level of social support) to 12 (lowest level of social support). The MSPSS has demonstrated adequate reliability and validity (
35). The internal consistency of the MSPSS for the current study was 0.96.
World Health Organization Disability Assessment Schedule (WHODAS 2.0).
The eight-item life activities subscale of the WHODAS 2.0 was used to measure difficulties in taking care of household and work or school responsibilities as a result of general medical or mental health conditions. Mean scores range from 20 to 100, with lower scores indicating less difficulty and higher scores indicating more difficulty with functioning. The WHODAS 2.0 has demonstrated good validity and reliability (
11). The internal consistency of the WHODAS 2.0 life activities subscale for the current study was 0.96.
Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q).
The 16-item Q-LES-Q (
29) was used to measure participants’ satisfaction with general health, relationships, and other life activities. Scores range from 1 to 5, with higher scores indicating more life enjoyment and satisfaction. The Q-LES-Q has demonstrated good reliability and validity (
29). The internal consistency of the Q-LES-Q for the current study was 0.94.
Purpose in Life Subscale (PILS).
The 14-item PILS, part of the Ryff Scales of Psychological Well-Being (
36) was used to measure participants’ sense of purpose in life. Scores range from 14 to 84, with higher scores indicating a greater sense of meaning or purpose in life. The PILS has demonstrated adequate reliability and validity (
37). The internal consistency of the PILS for the current study was 0.85.
Results
Characteristics of Samples
The sample consisted of 499 adult participants from several different settings, each of which is described in the following text. Information about the samples is presented in
Table 1. Participation in the study was voluntary, and no compensation was provided for completing the questionnaires. For all samples, recruitment ended when the COVID-19 pandemic began.
Inpatient medical sample.
The inpatient medical sample consisted of 197 adults who received inpatient medical treatment at a tertiary care teaching hospital in Providence, Rhode Island. Patients from designated medical units were approached during their hospital stay to participate in the study. After providing informed consent, patients were given the one-time packet of questionnaires to complete. Nine inpatients had a family member who also completed questionnaires.
Inpatient psychiatric sample.
The inpatient psychiatric sample consisted of 104 adults who received treatment for various mental health concerns at a psychiatric unit of a tertiary care teaching hospital in Providence, Rhode Island. Nursing staff recommended which patients on the unit were appropriate to approach for inclusion in the study. After obtaining informed consent, patients were given the one-time packet of questionnaires to complete. Patients were informed that survey responses would not affect their treatment.
Outpatient medical sample.
The outpatient medical sample consisted of 37 adults who sought medical treatment from a medical clinic in Providence, Rhode Island, affiliated with the teaching hospital. Patients who arrived at their appointment were approached and asked to participate in the study. Once they consented, patients had the option to complete the one-time packet of questionnaires before or after their appointment. Patients were informed that survey responses would not affect their treatment.
Outpatient psychiatric sample.
The outpatient psychiatric sample consisted of 65 adults who sought mental health treatment from a psychiatric clinic affiliated with the teaching hospital in Providence, Rhode Island. Patients who arrived at their appointment were approached and asked to participate in the study. After providing informed consent, patients completed the one-time packet of questionnaires before or after their appointment. Patients were informed that survey responses would not affect treatment.
Nonclinical sample.
The nonclinical sample consisted of 87 adults from the community and nine family members of patients who were recruited from the inpatient medical and psychiatric sites. Community participants included personal family members and friends of the current study’s researchers and staff. They were invited by e-mail to complete the questionnaires online. Family members who visited patients during their hospital stay or accompanied them to their outpatient appointment were approached and asked to participate in the study. Nine such family members completed questionnaires onsite.
Descriptive Statistics
We began the analyses with the exploration of descriptive statistics. Means±SDs for the BMAS items and all other questionnaires are broken down by recruitment setting and are listed in
Table 2. As expected, distress levels were higher in psychiatric and inpatient settings compared with the outpatient medical setting and among the community sample.
Reliability
We evaluated internal consistency by using Cronbach’s coefficient alpha. Coefficient alpha for the four BMAS items was 0.84 for the full sample and is broken down by recruitment setting in
Table 3.
Validity
We first set out to test the hypothesis that each BMAS item measures a unique construct. We tested this hypothesis by correlating each BMAS item with all other BMAS items. We expected significant correlations between all four BMAS items, because each domain is expected to influence the other areas. However, we wanted to ensure that each BMAS item was not too highly correlated with other BMAS items, because an especially high correlation (e.g., 0.75 or higher) might suggest that the items are measuring the same construct. Correlations between BMAS items ranged from 0.45 to 0.69 and are presented in
Table 4.
Concurrent validity.
Concurrent validity of the BMAS was analyzed by using Pearson product-moment correlations between BMAS items and the mean scores on the scales designed to relate closely to the constructs of BMAS items. We correlated the BMAS functioning item (i.e., getting things done) with the WHODAS 2.0, the BMAS emotional support item with the MSPSS, the BMAS quality of life item with the Q-LES-Q, and the BMAS purpose in life item with the PILS of the Ryff Scales of Psychological Well-Being. We expected BMAS items to correlate moderately strongly with scales that were designed to measure similar constructs. Correlations between scales are listed in
Table 4. As expected, correlations were moderately strong, ranging from −0.63 to 0.73.
Construct validity.
We tested construct validity by comparing BMAS item scores in a community sample with BMAS scores in various help-seeking samples. We compared scores by using nonpooled t tests (
Table 2), because sample sizes and variances were not homogeneous. In most comparisons of the clinical samples versus the community sample, the clinical samples reported being significantly more distressed.
Discussion
The four-item BMAS shows promise as a brief, multidimensional scale that assesses four unique and clinically significant areas: the ability to complete tasks that need to be completed, satisfaction with emotional support in relationships, quality of life, and purpose in life.
Reliability
The BMAS demonstrated reliability with internal consistency statistics above 0.70 in multiple samples. The coefficient alpha in the full sample was 0.84, which is strong given that the measure consists of only four items. In the subsamples, coefficient alpha was lowest but still acceptable in the inpatient psychiatric sample. Of interest, mean scores on all BMAS items were lowest in this subsample, and variability was relatively high. These findings are understandable, given that people who need psychiatric help often have difficulty functioning or getting the support that they need in relationships. Such people may also struggle with the meaning and purpose of their lives.
Validity
Concurrent validity.
As expected, each BMAS item demonstrated a moderately strong correlation with the established scale of the construct that it was designed to measure. Given the difficulty of attaining even moderately strong correlations with just one item, the current study’s moderately strong correlations demonstrate adequate validity. The strongest correlation was between the BMAS purpose in life item and the PILS.
Construct validity.
When we compared the community sample with each of the clinical samples, we found that, in nearly every case, significant differences existed between samples. This finding suggests that the four items of the BMAS are able to discriminate between clinical and community samples, which supports construct validity. However, no differences were found between the community sample and the outpatient medical sample for the BMAS items concerning the ability to get things done, receipt of emotional support, and quality of life. A possible explanation for this finding may be that people seeking outpatient help for a general medical problem have less severe illness and are functioning better than those seeking psychiatric help or inpatient medical help.
Limitations and Directions for Future Research
Although we had a relatively large sample size, some limitations should be noted. First, the sample was diverse with regard to income and education but not with regard to race and ethnicity. Future research should recruit more people of color and of Latinx cultural backgrounds. It would also be helpful to collect more data from outpatient medical samples and to recruit an even larger community sample.
Second, we were not able to create population norms for the BMAS, and future research may address that gap. One barrier to this task is that three of the established measures we used to validate the BMAS do not have population norms or cutoff scores, making it difficult to conduct the analyses.
Third, this study was not intended to measure change over time. Future studies should assess the ability of the BMAS to track course of illness.
Fourth, more studies of the clinimetric properties of the BMAS would be useful. Criteria for clinimetric patient-reported outcome measures have been developed, and future studies should explore the BMAS in light of those criteria (
9). Future studies may explore the ability of the BMAS to detect treatment-related improvements in well-being. Future studies should also formally explore ease of use as well as clinician and patient impressions of the utility of the BMAS in clinical practice.
Implications for Practice
The BMAS was designed to offer clinicians and patients a brief, nonburdensome measure that assesses eudemonic well-being in four domains. Patients’ BMAS responses can be a starting point for a conversation about how patients are experiencing their lives. It can be used easily as part of routine patient encounters, regardless of diagnosis, in both inpatient and outpatient settings.
Patients were willing to have their status evaluated routinely with a scale that is easy to complete. Clinicians whose patients participated valued the quantifiable data on different aspects of their patients’ life experiences and reported that administration of the BMAS did not interfere with their busy practice schedule. Clinicians also noted that scores on the BMAS alerted them to problems and strengths in their patients’ lives.
Conclusions
The BMAS demonstrates preliminary promise in fulfilling the need for an ultrabrief measure that provides a broad picture of well-being. The BMAS is a useful tool for assessing patients with any clinical condition for which assessing well-being is desirable.
Acknowledgments
The authors acknowledge Sheila Pho, B.A., and Anita Curran, B.A., for their work on data collection, recruitment, and manuscript editing.