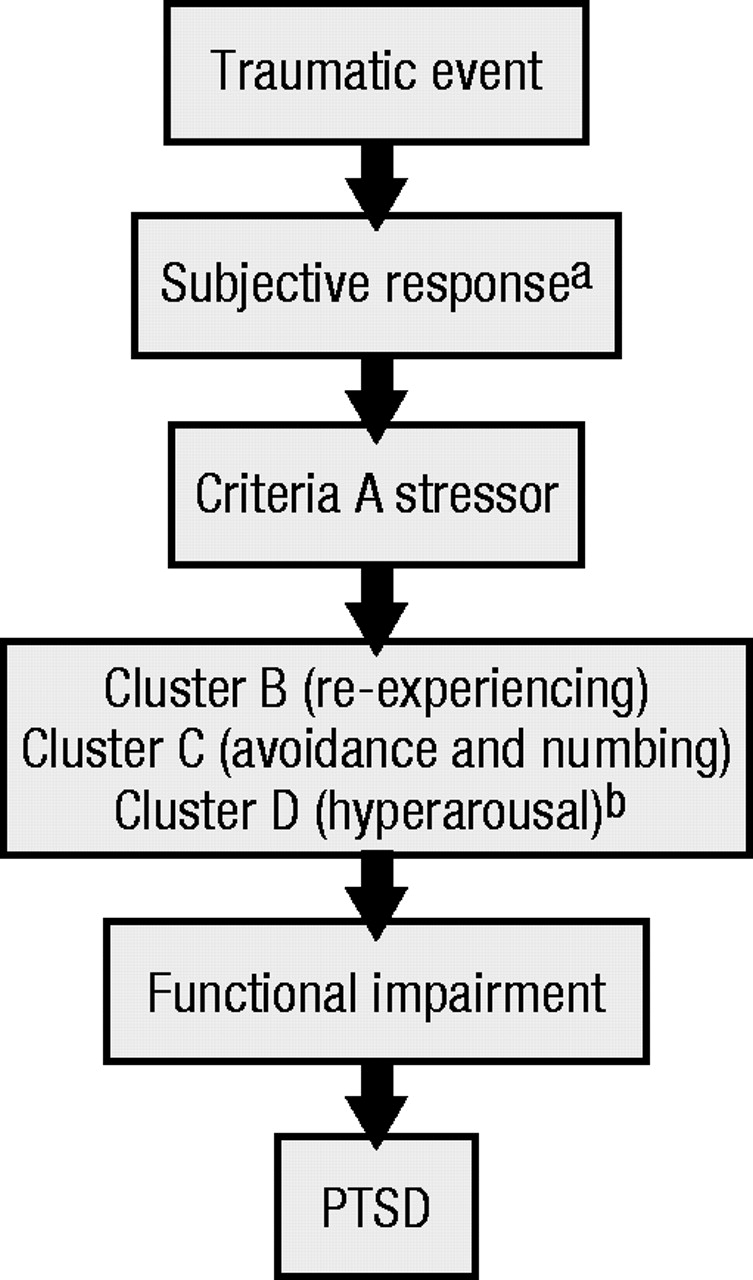
The core features of posttraumatic stress disorder (PTSD) include exposure to an event that involves actual or threatened death or serious injury to the self or others with an associated response of intense fear, helplessness, or horror and symptoms from each of three clusters involving reexperiencing the event, avoiding stimuli related to the event and psychic numbness, and persistent increased arousal (
1). Although descriptions of the effects of such events on individuals have long existed, PTSD was not recognized as a distinct diagnostic entity until its incorporation into the Diagnostic and Statistical Manual, 3rd Edition (
2). For at least a century before PTSD was officially born, investigators noted somatic, physiologic, and behavioral consequences of trauma, currently embedded in the DSM-IV criteria. As early as 1871, Da Costa described the autonomic cardiac symptoms of soldiers exposed to the horrors of the Civil War (
3). During the early 1900s, psychoanalysts observed “traumatic neurosis” that resulted from different forms of trauma. In World War I, “shell shock” was understood as a form of brain trauma caused by the terror induced by exploding shells. Although Lindemann emphasized acute and distorted grief reactions in the aftermath of the 1941 Coconut Grove disaster, survivors and family members of victims were left with nervousness, fatigue, nightmares, and other symptoms that resembled current conceptions of PTSD (
4).
The diagnosis that came closest to what we know as PTSD in DSM-I was “gross stress reaction” (
5). This diagnosis suggested that everyone had a breaking point and, given a severe enough trauma, it would be relatively “natural” to have a severe reaction. In DSM-II, the corresponding category was renamed “transient emotional reaction,” which emphasized the temporary nature of the psychological response to an overwhelming trauma (
6). It was not until after long-term post-war follow-up studies of Vietnam veterans that investigators realized these “reactions” were anything but temporary for many of the affected veterans. With the introduction of DSM-III, PTSD was born. In the initial iteration, symptoms needed to be present for at least 6 months before the diagnosis could be made, but in DSM-III-R the required duration was shortened to 1 month (
7).
In DSM-IV, the category of acute stress disorder, manifested by the same constellation of symptoms as PTSD, was added. The major difference between acute stress disorder and PTSD is that the duration of symptoms and distress is less than 1 month in the former disorder. If symptoms persist for more than 1 month, the diagnosis changes to PTSD. The “stressor” criteria in DSM-IV was broadened to include a subjective component—experiencing the trauma with helplessness and horror—and include traumas that are witnessed or occur to loved ones or are personally experienced. Finally, in DSM-IV, the individual must experience avoidance and psychic numbing rather than just avoidance (
2).
Perhaps no other diagnostic category has gone through as many alterations and permutations as has PTSD. Until recently, many investigators and clinicians considered PTSD a product of malingering or a form of personality disorder (
8). Over the last 10 or so years, however, the validity of PTSD has become well established and is currently considered one of the most prevalent and disabling psychiatric disorders in civilian and military populations (
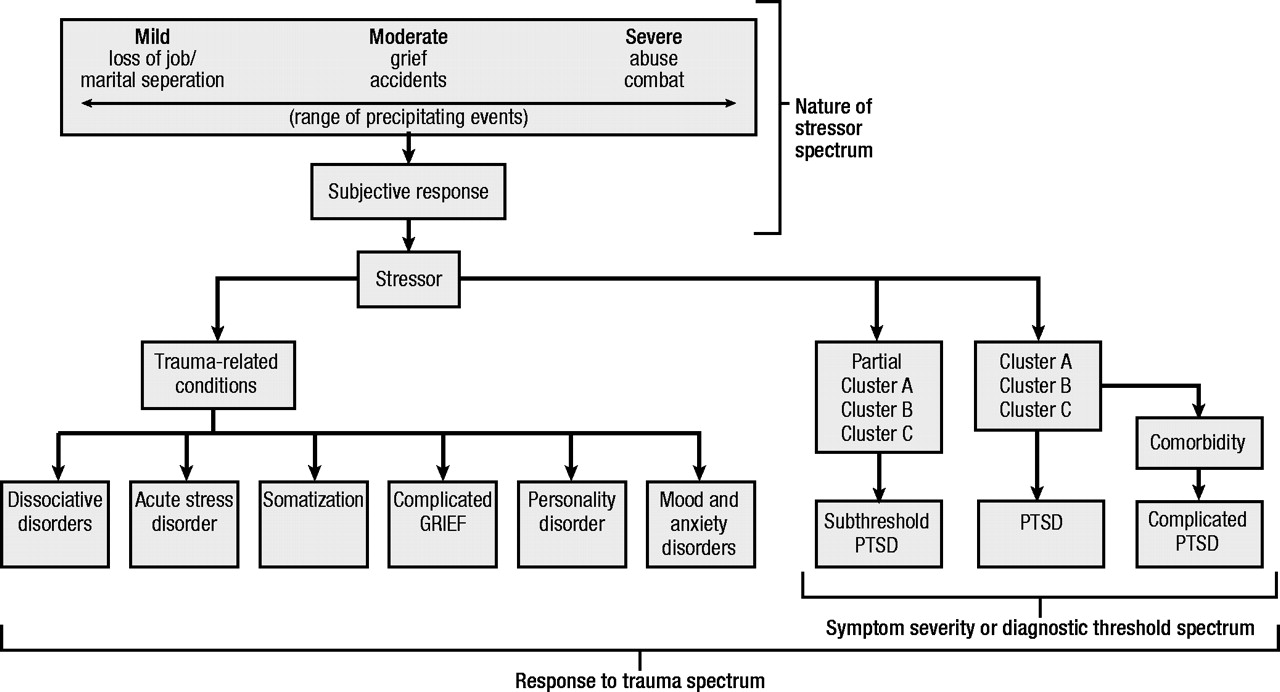
9). It is still not clear whether PTSD, as currently conceptualized, is a distinct and homogeneous category (Figure 1) or whether it would be more accurate to think of PTSD as being part of one or more dimensions or spectra (Figure 2). PTSD is rarely found alone; it is often comorbid with several other psychiatric diagnoses, which calls into question the use of the current categorization of PTSD. In the rest of this manuscript, the authors present the case that PTSD can best be understood as existing along at least three spectra: 1) one based on symptom severity (or diagnostic threshold), 2) another based on the nature of the stressor, and 3) a final one based on potential responses to trauma.
Symptom severity
Using DSM-III criteria, the National Comorbidity Survey found a lifetime prevalence of PTSD of 7.8%. This survey also recognized the impact of several noncombat forms of trauma, including rape and molestation in women and witnessing someone being badly injured or killed (
10). Using similar criteria to identify patients with PTSD, numerous studies have demonstrated substantial biopsychosocial impairment for occupation (
11), somatic distress and concomitant medical illness (
12), poor quality of life (
13), suicidality (
14,
15), impaired intimacy (
16), increased burden to spouse or partner (
17), and social dysfunction (
18). Other studies, however, have begun to demonstrate comparable impairment in individuals who experience only some, but not all, symptoms of PTSD.
Marshall et al. (
19) reviewed studies that demonstrated that subthreshold PTSD caused by various stressors was as common as full PTSD. In the National Vietnam Veterans Readjustment Study (
20), partial PTSD was defined by levels of dysfunction equivalent to PTSD, the presence of two of three symptom clusters, or meeting most criteria in each of the three clusters. Subthreshold PTSD was reported in 22.5% of men and 21.2% of women exposed to war-related trauma in Vietnam. In a longitudinal study of 132 persons involved in serious motor vehicle accidents, 28.5% met criteria for two symptom clusters 1 to 4 months after the accident (
11). Of 136 survivors of a plane crash into two apartments, 20% met criteria for two symptom clusters followed for 6 months (
21). 146 political prisoners in the former German Democratic Republic were compared to subjects in that country who had not experienced trauma. 29% met criteria for partial PTSD, which was defined as satisfying criteria in the reexperiencing cluster and either hyperarousal or avoidance clusters (
22). A community study that used standardized telephone interviews of 1002 persons asked about trauma, and positive replies were given a DSM-IV PTSD symptom checklist. Persons with partial PTSD had clinically meaningful levels of functional impairment in association with their symptoms (
23). Impairment could not be directly attributed to PTSD symptoms in this sample, however, because there was no control for comorbid conditions.
More recently, Marshall et al. (
19) found that 2608 of 9358 individuals on National Anxiety Disorders Screening Day 1997 had at least one PTSD symptom for at least 1 month’s duration. Impairment increased linearly with each increasing number of subthreshold PTSD symptoms. Even after controlling for the presence of major depressive disorder, individuals with subthreshold PTSD were at elevated risk for suicidal ideation. A limitation of this study includes the assessment of impairment by self-report and failure to assess for specific areas of impairment, such as occupational or social functioning.
Subthreshold symptoms may represent a prodrome of the full syndrome or residual symptoms of PTSD in partial remission. Regarding the former possibility, individuals who react to trauma with dissociation are at elevated risk for later developing the full syndrome of PTSD (
9). For many patients, mild symptoms, such as numbing of affect and irritability limited to the recollection of trauma, persist indefinitely. Even after treatment, many individuals with PTSD continue to suffer from residual symptoms years after the full syndrome is no longer present (
19). Although not yet empirically validated, individuals with residual symptoms may be more susceptible to developing the full syndrome after subsequent traumatic exposure than individuals with full symptom and functional recovery. Further complicating matters, a characteristic course of PTSD is fluctuating symptom severity, with persons meeting full criteria for diagnosis intermittently over the course of many years (
24).
One side of the severity spectrum contains individuals with subthreshold symptoms. In the middle of the spectrum is uncomplicated PTSD, and on the other side of the severity spectrum is PTSD complicated with multiple comorbidities. More than 80% of patients with chronic PTSD have at least one comorbid psychiatric condition, most often mood, anxiety, or substance use disorders (
10). When comorbidity is present, PTSD is often misdiagnosed, chronic, more severe and impairing, and more difficult to treat (
9).
Stressor criteria
An important evolution in the diagnostic criteria for PTSD concerns the inclusion of the victim’s appraisal of the event. Before DSM-III, many clinicians limited the diagnosis to individuals exposed to combat or only the severest forms of civilian trauma. In DSM-III and DSM-III-R, the event was required to be objectively catastrophic and out of keeping with ordinary events of life. Automobile accidents or death of a loved one did not qualify. Although discussed in the text of DSM-III-R, the person’s response to the event was not included in the criterion set. DSM-IV, on the other hand, lists criterion A as exposure to a traumatic event in which both of the following conditions were present:
1.
The person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury or a threat to the physical integrity of self or others.
2.
The person’s response involved intense fear, helplessness, or horror.
Perry et al. (
25) showed that the severity of PTSD symptoms in burn victims was not proportional to the extent of injury but rather to the person’s perception of injury. A clear definition of criterion A is of absolute importance because it is necessary for the diagnosis of PTSD. For example, persons who suffer from all other symptom clusters would not meet the diagnosis of PTSD if the precipitating stressful event failed to qualify as a criterion A trauma. Snow et al. (
26) found that the prevalence of PTSD among 2859 Vietnam veterans ranged from 1.8% to 15% depending on whether combat exposure was defined relatively narrowly or broadly. The significance of the person’s subjective reaction to a traumatic event is underscored by Yehuda’s study of adult offspring of Holocaust survivors (
27). Adult offspring of Holocaust survivors were more likely than demographically similar comparison subjects to designate a non–life-threatening event as their most distressing event, despite having experienced potentially life-threatening events. Although both groups had a similar number of traumatic events, there was a greater prevalence of PTSD in the adult offspring of Holocaust survivors. Davidson and Foa (
8) state “clinical observations seem to suggest that for some patients the loss of a job or marital separation may also give rise to this syndrome, leading to criteria B (reexperiencing), C (avoidance and numbing), and D (hyperarousal) symptoms of PTSD.” Two studies assessed the impact of “low-magnitude” trauma that showed that marital disruption, death of a loved one, failed adoption plans, miscarriage, and poisoning may lead to PTSD (
28,
29). The nature of the stressor is believed to have considerable breadth, from the loss of a job or marital separation to the loss of a loved one or involvement in a serious accident or involvement in abuse or combat.
Two recently published studies illustrate how individuals may reexperience a stressful event, avoid reminders of the event, and have hyperarousal with associated significant impairment yet fail to qualify for the diagnosis of PTSD if the stressful event is not deemed traumatic by DSM-IV. In the first study, Pfefferbaum et al. (
30) discovered that 20% of 69 sixth grade children met criteria for reexperiencing, avoidance, and hyperarousal and had difficulties functioning 2 years after the bombing of the Oklahoma City Alfred P. Murrah Federal Building, despite living 100 miles away and not knowing anyone killed or injured. The authors did note that media exposure was a significant predictor of symptomatology. In a second study, Zisook et al. (
31) reported chronic and debilitating symptoms of PTSD in a group of mostly middle-age and older widows and widowers, even after relatively chronic terminal illnesses and when the death had been expected. Although PTSD was more prevalent when the death was “unnatural” (i.e., suicide or homicide), it was still seen in almost 10% of the sample after spouses died of natural causes. A spectrum of stressors and a spectrum of symptoms below the DSM-IV threshold produce impairment and a need for treatment. These spectra must be elucidated further in future diagnostic manuals.
Trauma-related conditions
Stressful events are known to precipitate and exacerbate various psychiatric conditions. In the ICD-10 classification (
32), acute and chronic PTSD, adjustment disorders, and personality change after catastrophic stress are included in a stress and trauma section. Similarly, the DSM-IV Advisory Subcommittee unanimously voted to classify PTSD in a new stress response category (
33). One proposal for classification might include PTSD at the severe end of a spectrum of stress-related disorders, with adjustment disorders at the other. In that vein, McFarlane et al. (
34) showed that responses to trauma are heterogeneous and include PTSD, major depressive disorder, drug abuse, other anxiety disorders, and eating disorders. According to Yehuda and McFarlane (
35), “the relative rareness of pure PTSD, compared to the presence of more complex forms, suggests that traumatic stress may precipitate a whole host of symptoms and conditions.” In this section, the authors review several stress-related conditions and examine their associations with PTSD.
Complicated grief
Diagnostic and Statistical Manual-IV includes bereavement as a “V” code contained in the section “other conditions that may be a focus of clinical attention.” Despite clinical observations by various authors, including Freud (
36), Lindemann (
4), Bowlby (
37), Parkes (
38), and Horowitz (
39), that prolonged grief reactions are functionally impairing and often differ from diagnostic classifications of depression or other established psychiatric disorders, the makers of DSM-IV excluded complicated or prolonged grief as an axis I diagnosis because of a lack of empirical evidence regarding the symptoms (
40). Since that decision was made, at least two separate groups of investigators have provided empirical data suggesting that a diagnostic category of complicated grief may be appropriate.
Prigerson et al. (
41) found a distinction between depressive symptoms and symptoms of complicated grief in 82 recently widowed elderly individuals. Complicated grief is characterized by persistent intense grief, with yearning, pining, and longing for the deceased, recurrent intrusive images of the death, and a distressing admixture of avoidance and preoccupation with reminders of the loss. Memories of the deceased are either blocked or excessively sad. Prior episodes of major depression seem to be risks for the development of complicated grief. Prigerson and colleagues found that bereaved individuals who meet criteria for complicated grief were substantially more impaired psychiatrically, socially, and medically and had greater mortality rates than bereaved individuals who did not evidence complicated grief. Similarly, Horowitz et al. (
39) reported that 70 bereaved spouses had symptom patterns that did not overlap with those of major depressive disorder. Symptoms included intense intrusive thoughts, pangs of severe emotion, distressing yearnings, feeling excessively alone and empty, excessively avoiding tasks reminiscent of the deceased, unusual sleep disturbances, and maladaptive levels of loss of interest in personal activities more than 1 year after the loss. Prigerson et al. and Horowitz et al. emphasized that complicated grief overlaps with symptoms of PTSD but is not identical to it. Both groups also found symptoms of complicated grief, even when the death was not particularly sudden or violent.
The situation may be even more complicated and more akin to PTSD when the death is “unnatural” and violent, such as a homicide, suicide, or accidental. In addition to the separation distress seen after such a loss, violent death also may incite traumatic distress as manifested by cognitive reenactment of the dying, terror, and avoiding reminders of the dying (
42). Adults who lost a family member to homicide had recurring images of the violent death as a disorganizing flashback and dream and showed greater degrees of bereavement and trauma than normal subjects and other cohorts of bereaved subjects (
43). Zisook et al. (
31) found that death from accident or suicide was associated with PTSD symptoms in newly bereaved spouses. The consensus criteria (
44) developed by Prigerson and colleagues may help facilitate additional research and the development of standardized diagnostic criteria. Further study also is needed in this unique population to address traumatic or complicated grief as a subgroup of PTSD.
Somatization
The earliest descriptions of the effects of trauma on individuals focused on physical manifestations. In defining the new category of PTSD, however, the framers of DSM-III focused on the psychological symptoms of reexperiencing a traumatic event, avoidance and numbing, and hyperarousal. Subsequently, several studies found high rates of somatic symptoms in persons with PTSD. Most of these studies addressed the relationship between combat-related PTSD and physical symptoms.
Beckham et al. (
45) showed that somatization and PTSD symptom severity in Vietnam veterans were related to self-reported health problems and not the sole result of self-report bias. In a study of 21,244 Gulf War veterans, the number of physical complaints was higher in veterans with PTSD compared to those with any other psychological condition, those with a medical illness, and those labeled as healthy (
46). The most common somatic symptoms included fatigue, sleep disturbance, joint pain, memory loss, headache, depressed mood, and difficulty concentrating. In addition to combat-related PTSD, McFarlane et al. (
12) showed high rates of physical complaints in a community sample of firemen with PTSD. Based on data from an event-related potential study that showed that individuals with PTSD had lower responsiveness to external stimuli and a general difficulty in evaluating the significance of stimulus change, McFarlane posited that somatization may be explained by an impaired ability to differentiate relevant from irrelevant stimuli and a tendency to focus on and misinterpret somatic sensations. In the DSM-IV field trials, high levels of association between trauma and somatization were reported (
24). A prospective study by Andreski et al. (
47) found increased risk of somatization symptoms in persons with PTSD beyond that expected by the presence of comorbid psychiatric disorders.
Rather than considering co-occurring PTSD and somatization disorder as totally separate conditions, further research is needed to discern whether somatization may be one potential pathway for trauma to express itself psychologically, just as there are somatic symptoms in depression and other anxiety disorders. Prospective studies may help discern whether there is a subgroup of PTSD sufferers who have prominent somatic complaints and how this subgroup differs from individuals with fewer somatic symptoms. van der Kolk et al. (
24) found a substantial number of persons who, even after their PTSD symptoms had resolved, continued to suffer from high levels of somatization. This group is unlikely to receive effective clinical care if their symptoms are not viewed from a dimensional perspective.
Acute stress disorder and dissociation
By current definition, PTSD requires minimum symptom duration of 1 month. Before DSM-IV, persons who experienced PTSD symptoms from severe trauma for less than 1 month were given the nonspecific diagnosis of adjustment disorder. The diagnostic nomenclature did not recognize a difference between persons who experienced mild, transient difficulties caused by a stressor and persons with severe PTSD symptoms of less than 1 month. To address this problem, the diagnosis of acute stress disorder was added to DSM-IV, which added a category to handle spectrum-like phenomena. The significant differences between acute stress disorder and PTSD are an increased emphasis on dissociative symptoms in acute stress disorder and duration of symptoms of less than 1 month (
48). Several retrospective and prospective studies found that PTSD was predicted by dissociation at the time of or immediately after trauma (
49). Acute stress disorder serves as an important risk factor for the development of PTSD. Still, there could be a group with subthreshold or full PTSD symptoms for less than 1 month who did not experience dissociation and would be diagnosed by current conventions as having an adjustment disorder.
Marshall et al. (
50) reviewed six prospective and two retrospective studies to determine the proportion of trauma survivors who had PTSD symptoms of less than 1 month’s duration or who met full criteria for PTSD yet did not have prominent dissociative symptoms at the time of trauma. They did not meet criteria for acute stress disorder. These studies showed a substantial number of persons with PTSD symptoms of less than 1 month who did not meet criteria for acute stress disorder, based on a lack of substantial dissociative symptoms around the time of the event. The data showed that acute stress disorder was indicative of greater severity and chronicity of PTSD, however. Using a dimensional approach, individuals who do not respond symptomatically to trauma are at one end of the spectrum. They constitute the largest number of people along the spectrum of PTSD. A second group meets criteria for an adjustment disorder. Further along the spectrum of PTSD severity are persons who also experience peri-traumatic dissociation (e.g., have an acute stress disorder). This group is not only at higher risk to develop PTSD but also is likely to develop a severe and chronic case. The most severe point on the spectrum is complicated PTSD, in which depression, panic disorder, and other comorbid conditions are evident.
Borderline personality disorder
Because of the broad range of symptoms seen in survivors of trauma, clinicians may incorrectly identify those symptoms as character pathology rather than a response to trauma (
51). Zanarini et al. (
52) studied 504 inpatients with personality disorders and found PTSD to be a common comorbid disorder among borderline patients. Numerous reports describe childhood traumatic experiences in adult patients diagnosed with borderline personality disorder (
53–
55) and other reports of traumatic childhood experiences as common antecedents of PTSD (
56,
57). Although there is currently a paucity of research in this area, the diagnosis of borderline personality disorder often may be a misattribution of symptoms more correctly conceptualized as chronic PTSD.
Major depressive disorder and posttraumatic stress disorder
Several studies have found high rates of comorbid major depression in persons diagnosed with PTSD (
10,
14,
29,
58–
60). When PTSD is comorbid with major depression, a chronic course often results. The relationship between major depressive disorder and PTSD is complex; the temporal relationship is variable. Some investigators have demonstrated that preexisting depression serves as a risk factor for PTSD (
56,
61). Others have found that depression is often secondary to PTSD (
10,
61,
62). The complexity of the relationship is highlighted by a study that examined the development of PTSD and major depressive disorder in adult offspring of Holocaust survivors. Yehuda and colleagues found a strong relationship between parental PTSD and the occurrence of PTSD in offspring. Parental trauma exposure more than parental PTSD, however, was significantly associated with lifetime depressive disorder in offspring (
63).
Several investigators have suggested that the three most common impairing psychological sequelae from traumatic stress are PTSD alone, major depressive disorder alone, or comorbid PTSD and major depressive disorder (
64–
67). Breslau et al. (
68) reviewed retrospective and prospective data from the Epidemiologic Study of Young Adults in southeast Michigan (
58) to demonstrate whether traumatic events increased the risk for depression independent of their PTSD effects. Breslau et al. found a markedly increased risk for major depression in persons with PTSD but not in persons exposed to trauma who did not develop PTSD. This increased risk suggests that PTSD and major depression may share a common underlying vulnerability. Stated otherwise, major depression after traumatic events and PTSD do not have separate vulnerabilities but exist along a spectrum of potential sequelae of traumatic experiences.
Other anxiety disorders
Several authors have elaborated on the phenomenologic similarities between PTSD and other anxiety disorders for panic disorder (
69,
70), phobic anxiety (
71,
72), and generalized anxiety disorder (
73). Episodic physiologic arousal or intense fear cued by stimulus exposure is seen in panic disorder, phobic anxiety, and PTSD. PTSD and generalized anxiety disorder are associated with poor concentration, irritability, hypervigilance, exaggerated startle response, and sleep disturbance. According to the National Comorbidity Survey (
10), the estimates of lifetime prevalence of other anxiety disorders in persons with a lifetime history of PTSD were significantly greater than in persons without a lifetime history of PTSD. Comorbidity may be explained in part by the significant overlap in symptomatology. As with major depression, some investigators also have found that anxiety disorders other than PTSD can occur after trauma, either alone or as a comorbidity with PTSD (
65,
66). This finding suggests that a possible spectrum of anxiety-related symptoms and symptom clusters can follow trauma.
A handful of studies also have examined the relationship of PTSD to obsessive-compulsive disorder. Historically, Janet observed that obsessive-compulsive disorder can be a consequence of emotional shock (
71). Kardiner described “defensive ceremonials” associated with traumatic neuroses (
74). Both conditions are associated with persistent, recurrent, intrusive, and unwelcome images, thoughts, or memories, The major difference between the intrusive thoughts in obsessive-compulsive disorder and thoughts in PTSD are that the intrusive thoughts in obsessive-compulsive disorder are viewed by the individual as inappropriate and not related to experienced trauma. The intense fear, helplessness, or horror associated with the traumatic event in PTSD is generally not experienced in patients with obsessive-compulsive disorder. According to an epidemiologic catchment area survey of the general population, the risk of obsessive-compulsive disorder is increased 10-fold in persons with PTSD (
29). In veterans of high war zone stress, the prevalence of obsessive-compulsive disorder is 5.2% compared to 0.3% in veterans of low to moderate war zone stress (
75). There seems to be evidence, albeit limited at this time, of a possible PTSD-obsessive-compulsive disorder dimension, similar to that observed in other anxiety disorders.
Summary
An understanding of PTSD and stress-related conditions is in its infancy. This is not surprising given the fact PTSD was not recognized as a distinct diagnostic entity until 1980. Since that time, the diagnostic classification has undergone continuous change as our understanding of PTSD is refined. The authors believe that PTSD can be best understood through a dimensional conceptualization viewed along at least three spectra: 1) symptom severity, 2) the nature of the stressor, and 3) responses to trauma.
Among the severity spectrum, studies that review diagnostic thresholds reveal significant prevalence of PTSD symptoms and impairment that results from subthreshold conditions. Comorbidity patterns suggest that when PTSD is associated with other psychiatric illness, diagnosis is more difficult and the overall severity of PTSD is considerably greater. With regard to a stressor criteria spectrum, the diagnostic nomenclature initially only recognized severe forms of trauma personally experienced. More recently, however, the person’s subjective response and events occurring to loved ones were included. This has greatly broadened the stressor criteria by leading to an appreciation of the range of precipitating stressors and the potential impact of “low-magnitude” events. Given that responses to trauma vary considerably, another possible spectrum includes trauma-related conditions. Traumatic grief, somatization, acute stress disorder and dissociation, personality disorders, depressive disorders, and other anxiety disorders all have significant associations with PTSD.
Further research is needed to clarify and expand the current understanding of PTSD and other trauma-related conditions. Consideration of the severity of symptoms and the range of stressors coupled with the various disorders precipitated by trauma should greatly influence scientific research. The future undoubtedly will bring a refinement of the current understanding of PTSD and improved treatments.