This approach to clinical ethics teaching is a natural extension of traditional psychiatric resident supervision. It is not difficult to implement and may already occur implicitly in meetings between supervisors and residents when they focus on ethical issues. Making the process explicit and applying it to a variety of supervisory relationships occurring in residency, however, are crucial in the effort to develop a more systematic, clinically based approach to teaching ethics in psychiatry programs. The versatility and value of this supervisory strategy for teachers of psychiatry residents becomes apparent in illustrations of its use.
Case reports
Example One. A resident objected on ethical grounds to filling in federal forms that routinely declare certain psychiatric patients “decisionally incompetent.” In supervision, this issue was discussed in relation to a particular psychiatric inpatient whose decisional capacity did show some significant deficits. The resident had the impression that the patient’s financial benefits might be withheld if the form were not completed.
The first step in supervision was to clarify the patient’s psychiatric diagnosis and related deficits in cognition and judgment. This served two aims: 1) to make certain that the patient’s clinical needs were not obscured in the resident’s passion to “do the right thing” by fighting institutional bureaucracy, and 2) to teach the resident about the phenomenology of the patient’s illness and about ways of assessing his decisional abilities, the basic educational goals of clinical supervision in this case. The second step was to help the resident to identify the ethical issues involved, such as the resident’s view of coercion by the institution, the resident’s perceived duty to protect a vulnerable patient whose financial benefits were apparently in jeopardy, the limited autonomy of the patient because of psychiatric illness, confidentiality, and others. The process of clarifying the ethical binds and personal frustrations experienced by the resident made it possible to approach the patient’s care with a better separation of the therapeutic goals from the complexities of training within a certain institutional setting. The supervisor talked with the resident about the distinction between decisional capacity, a clinical assessment, and competence, a legal determination. The resident was encouraged to read about decisional capacity and neuropsychological testing and to gather more complete historical information about the patient. She also sought information from faculty and administrators at the institution about the actual use of the federal form.
Possible responses to the ethical dilemma, that is, whether and how to fill out the form, were then explored by the resident and supervisor. With support and further discussion with the attending supervisor and permission from the patient and his family, the resident made a decision to write a separate report documenting the observed strengths and deficits of the patient. The patient’s benefits were not hindered. The resident worked further to change the policy requiring routine completion of the form. The resident and supervisor followed the patient case afterward and discussed the impact, both positive (special attention to clinical issues, continuation of the patient’s benefits, and a modest sense of accomplishment for the resident) and negative (additional work and some disruption of routine), of the resident’s choices in later supervision sessions.
Example Two. A resident on the consultation-liaison service worried about a discharge request made by a woman who had taken an impulsive overdose of antidepressant pills during an argument with her boyfriend. She had very nearly died and was in the intensive care unit on the medicine service. The patient was the mother of two children and homeless. Of greatest concern to the resident was that the patient’s boyfriend frequently and severely beat her. Although the patient asked to leave the hospital and denied suicidality, the resident felt that it was “unethical” to let the patient go.
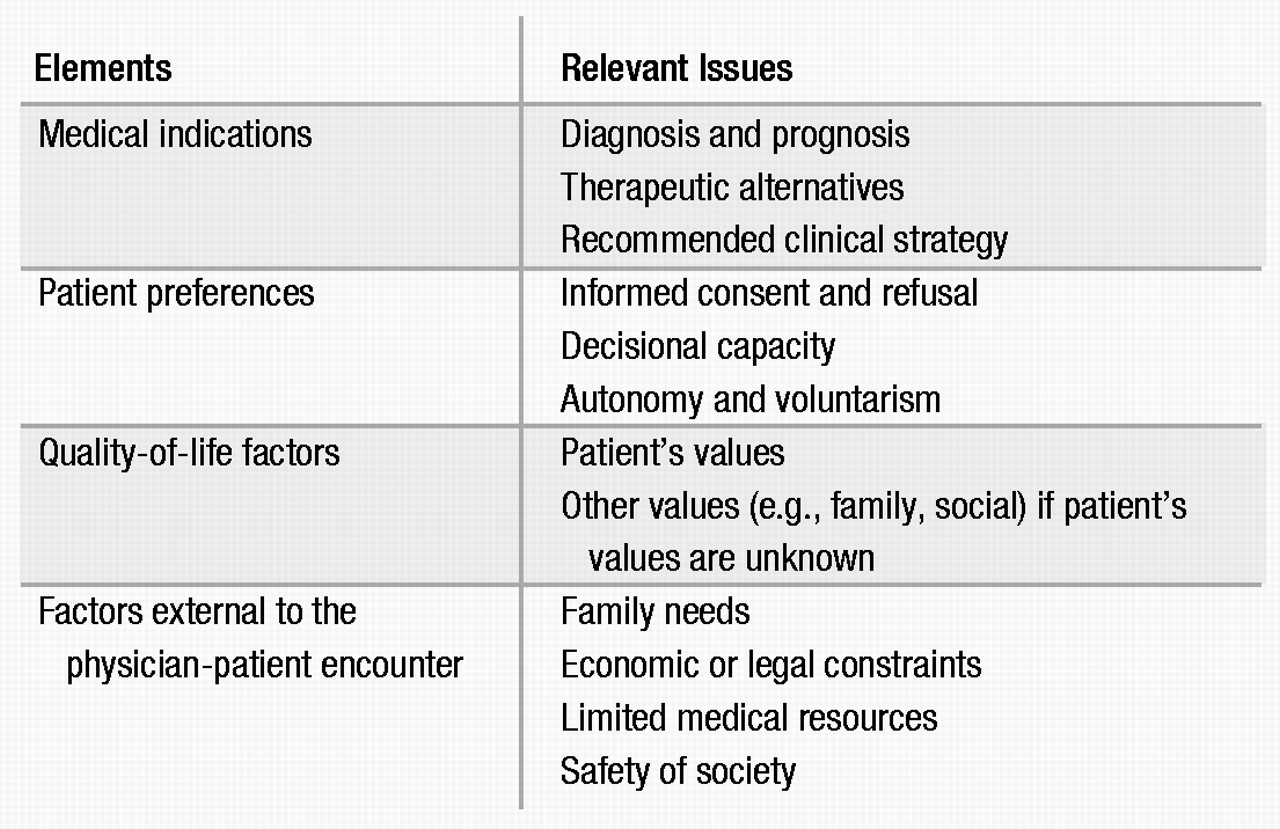
The first step in supervision was to evaluate the clinical situation of the patient. She exhibited QRS widening on ECG and had elevated blood levels of a tricyclic antidepressant. On mental status examination, she was cooperative, sleepy, distractible, inaccurate by 4 days on the date, and unable to add or subtract even small numbers. It was clear that the patient’s medical indications warranted continued hospitalization. A discussion of the ethical issues encompassed topics such as patient autonomy and preferences, decisional capacity and standards of competence, informed refusal of treatment, quality-of-life factors, the duty to report child abuse, and others. It became evident that the resident needed additional information on the children (who, as it turned out, had previously been placed with the patient’s father) and on delirium, antidepressant toxicity, physical abuse, resources for battered spouses, and legal and institutional guidelines on holding patients involuntarily and on reporting domestic violence.
The resident and supervisor discussed a number of possible responses to the patient’s discharge request, including, if necessary, coerced observation and treatment. An evaluation was done by the supervising attending physician who clarified that the patient was not demanding to leave the hospital immediately. The patient stated, in fact, that she wanted treatment so that she would “be ok” before returning to “the shelter.” The patient agreed to remain in the hospital until she felt “a little bit better” and to accept the social work consultation. After careful assessment, the attending physician determined that the patient was capable of this level of consent in the acute situation. With the agreement of the attending supervisor, the resident decided to speak with the patient about remaining in the hospital and meeting with a social worker to help with her social situation. Over the next several hours, as the patient’s cardiac toxicity and delirium cleared, she decided to return to her boyfriend. Psychiatric and social work follow-up was arranged. When the resident and supervisor reviewed the case, the resident was still concerned about the patient’s refusal of inpatient psychiatric care and her decision to return to a reportedly abusive relationship. He could, however, articulate the limits of the law, the rights of patients, standards of competence necessitated by different clinical situations, and his own thoughts about each of these issues. He believed that he had handled the case well despite its unsettling facts.
Example Three. A resident miscopied an evening insulin dose when writing the orders on an elderly patient being admitted to the psychiatric unit. She discovered the error the next day when she found that the patient’s blood sugar readings were in the low 100s rather than the usual low 200s. The patient felt “fine,” and the orders were corrected. She wondered how much to tell the patient and his family about the mistake in prescribing insulin.
In the first step, the patient’s clinical status was investigated, and the issue was discussed with members of the treatment team who then were especially vigilant in their observation of the patient. The patient was considered to be stable and unharmed by the incident. The supervisor and resident discussed the ethical issues that surround medical mistakes, such as respect for persons, truth-telling, beneficence, justice, and the role of clinical outcomes in ethical analysis. They further talked about the resident’s discomfort with the mistake. The supervisor and resident explicitly acknowledged that the resident had not made such errors before, directly addressing the resident’s embarrassment. They then gathered information and read about the ethical issues surrounding medical mistakes and truth-telling and about the management of insulin-dependent diabetes mellitus. The institution’s process for documenting mistakes, even for those with no clear harm inflicted, was also investigated and completed.
The choices before the resident (e.g., speaking with the patient and his family, or not, and talking further with the team members) were explored. The resident wished to talk about the error with the patient and treatment team immediately and with the family during their next scheduled session. The supervisor offered support to the resident as she pursued this series of discussions. Afterward, the supervisor reviewed with the resident the patient’s reaction (unconcerned), the family’s comments (critical), the teacher’s response (supportive), and the resident’s self-assessment (shaken but intact) and efforts to repair the situation (more than adequate). The supervisor and resident discussed this experience in the context of the resident’s personal and professional development as a psychiatrist.
Example Four. A psychiatric resident was told “confidentially” by a patient that he had sexually molested and physically hurt several girls though he had never been caught. The patient said that he now had his “eye on” a girl in his apartment complex. He offered no name, though he described her, and then would neither affirm nor deny any definite intention to abuse her. The patient had been admitted to the psychiatric unit to “rule out depression” after taking an overdose shortly after his wife left him.
The first step in supervision was to clarify the patient’s psychiatric diagnosis and to take measures ensuring the safety of the patient and of others on the locked ward. The supervisor and resident performed separate evaluations on this patient as a matter of ward routine. They both found that the patient had had a long history of self-destructive and difficult behaviors but had no prior psychiatric admissions. He had consistently been diagnosed with character pathology and experienced no psychotic or uniquely depressive symptomatology. He understood that sexual abuse of children was “damaging” and “wrong.” He clearly stated what the consequences would be if he were caught. The patient was observed closely and behaved in a safe manner on the ward.
The next step in supervision involved discussing a number of ethical issues, including physician-patient boundaries and “secrets”; physician duty-to-warn, patient privilege, and confidentiality; culpability for deliberate, harmful actions by nonpsychotic psychiatric patients; dilemmas posed by “difficult patients”; and others. The supervisor and resident next sought expertise from the hospital’s attorneys, reviewed psychiatric and medical codes of ethics, and learned more about the patient’s past history. With direction from the institution’s legal counsel, the supervisor intervened and advised the police about the patient’s vague threat to sexually abuse an unnamed, but identifiable, girl. Her family was then notified of the threat to the child. The supervisor and resident together informed the patient of this action. The supervisor and resident discussed therapeutic options for this difficult patient and considered possible responses to the many ethical dilemmas his care presented. Ultimately, the patient was discharged and referred for treatment of pedophilia. He was informed that he was regarded as accountable for his actions and the fact that he had undergone a psychiatric hospitalization did not relieve him of responsibility for his behavior toward others. In this case, the resident appreciated the collaborative approach taken by the attending supervisor and felt that he had learned in the process of the patient’s care. The series of decisions in this extraordinarily challenging case were reviewed by the supervisor, resident, treatment team, and the legal counsel of the hospital, allowing for some sense of resolution if not satisfaction with the case. Additional follow-up information was not obtained, as the patient went to another state.
Each of these examples demonstrates how the everyday care of patients poses significant ethical challenges to psychiatry residents. Use of this six-step strategy is felt to have improved the quality of resident teaching and patient care in each case. Supervisors experience the approach as straightforward and as not extending the supervisor and resident significantly beyond the usual tasks of supervision in a way that is burdensome or contrived. The strategy thus offers an excellent method for use by supervisors in their efforts to foster residents’ decision-making skills and clinical judgment in ethically complex situations.