Psychodynamic psychotherapy incorporates many principles of psychoanalysis. Despite the inherent challenges of developing a full understanding of psychoanalytic theory, central treatment guidelines may be distilled to provide the nonanalyst with a comprehensive system for appreciating conflict, symptoms, psychic pain, personality development, and the intricacies and power of the doctor-patient relationship. This article provides a distillation of the more useful attributes of psychoanalytic theory. Readers who are interested in an immersion in psychoanalytic theories, classical as well as more recent, such as post-Freudian ego psychology, object relations, self psychology, and interpersonal/intersubjective psychology, may consult any of numerous sources (
1–
5).
What are the psychodynamic psychotherapist's central beliefs?
A psychiatrist’s psychodynamic orientation includes each of the following ideas:
•
People feel and behave as they do for specific reasons.
•
People are frequently unaware of why they feel or behave in a certain fashion.
•
Past events and experiences, often outside of awareness, determine how people feel about themselves and their world.
•
The need to master psychological pain and discomfort is compelling and accounts for why many people behave consistently and predictably in often self-defeating or disappointing ways.
•
The power of the therapeutic relationship is predicated on the physician’s ability to provide a safe forum for examining psychological problems, feelings, and behaviors by maintaining an open, nonjudgmental, and empathic rapport with the patient.
•
The past experiences of both the patient and the therapist have a role in determining the valence and power of the therapeutic relationship.
•
A successful treatment must integrate both cognitive and affective components of the patient’s self-awareness and includes supportive as well as interpretive interventions.
Although many would consider these ideas to be common to all therapies, an elucidation of these central beliefs and their corollaries will demonstrate how dynamic therapy can be distinguished from other treatment models.
Understandable reasons underlie feelings, wishes, and behavior
This tenet stipulates that behavior is not haphazard. This important assumption of psychodynamic psychotherapists supports the quest by psychiatrist and patient to appreciate the meaningfulness of a patient’s feelings, hopes, discomfort, and symptoms within and outside of therapy. Unlike in other forms of psychotherapy, the dynamic psychotherapist is interested in the “why,” not just the “how.” The omnipresent question in the therapist’s mind is “Why now?” Why is this patient seeking treatment now? Why is this patient addressing this topic with me now? Is something being said about the treatment relationship? Is there an expression of discomfort about certain feelings? The ability to address these questions is predicated on the therapist’s understanding of “process communication.” The dynamic clinician listens to patients in a distinct manner that is unlike the listening that occurs in normal social discourse. Psychodynamic therapists understand that patients communicate on multiple levels and often in indirect fashion. Poignant material, for example, may be expressed through jokes, shifts in topic, revelations at the very end of a session, metaphors, and symbols. The organizing principle of listening, once again, is the curiosity about “why now.”
Another dimension of this tenet is the paradoxical phenomenon of ambivalence that all patients have about treatment, regardless of motivation and commitment to the psychotherapy. This ambivalence is manifested by subtle covert, and sometimes overt, behavior within the therapy that tends to oppose the goal of developing a deeper understanding of problems. It may take the form of missed appointments or an unwillingness to explore specific areas of the patient’s life. A common example of this ambivalence, known theoretically as resistance, is the patient’s jumping from one topic to a less upsetting one. The role of the dynamic psychotherapist is not to disabuse the patient of this ambivalence but rather to attempt to understand the psychological function served by the patient’s reluctance. Resistance serves a protective function against threatening feelings and fantasies. Greater understanding of the phenomenon deepens the psychotherapy and provides a resource for appreciating how earlier experiences in the patient’s life influence his or her current behavior within treatment and in the world at large.
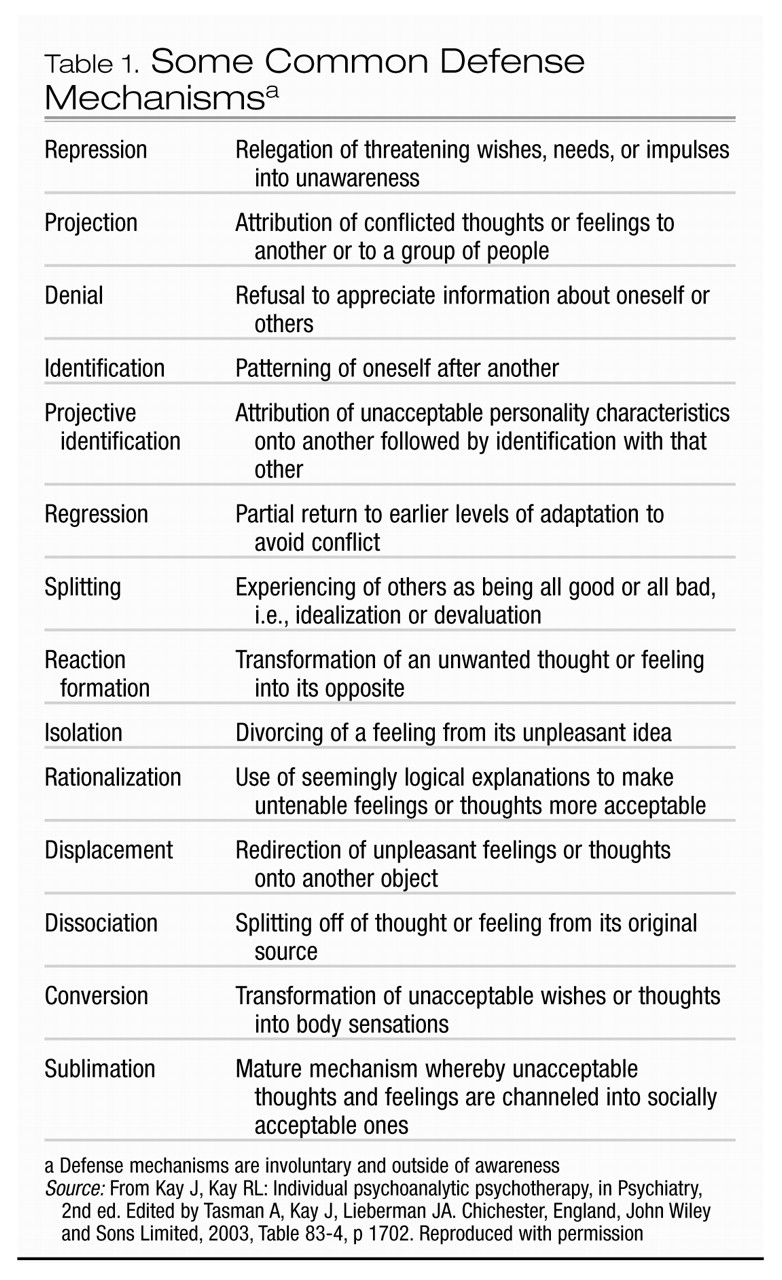
Among other things, personality or character reflects predictable ways in which people adapt to novelty as well as to affect. A person’s style of relating to both the internal and external worlds in attempts to ward off unpleasantness and strong feelings is served by maneuvers outside of awareness, which have traditionally been referred to as defense mechanisms (Table 1). Dynamic psychotherapy affords an opportunity to understand the psychological function of these adaptive and dysfunctional maneuvers.
Feelings and behavior are often a mystery to the patient
The notion that people experience and act on unknown wishes and fears is an enlightening concept for many patients. Support for this belief is found in the contributions of cognitive neuroscience. The study of learning and memory was advanced considerably through the scientific definition of types of memory. Memory can be categorized as short term or long term, with the latter divided into implicit and explicit memory. Implicit memory, the simplest form of memory, consists in the ability to perform certain tasks or procedures, or the knowledge of how to do so. It also includes perceptual-representational experiences. Implicit memory lacks a sense of self or temporality; it does not require conscious attention, and it does not rely on intact hippocampal function. Explicit memory includes memory of facts and events. In contrast to implicit memory, it does require conscious attention and a sense of recollection of the past, and it is dependent on intact hippocampal function.
Implicit memories begin to form shortly after birth. Repeated reciprocal interactions between mother and infant are the foundation of affective templates that organize neural structure and determine experience of the self and other. Implicit memory plays a crucial role in psychological trauma as well, which is why patients often cannot fully recall experiences of severe abuse and neglect. In short, much of mental life is outside of awareness.
The past lives in the present
The concept of implicit memory, coupled with the need to ward off and contain extremely disruptive feelings, explains why some traumatic and disappointing experiences are not accessible. In addition, early experiences shape personality and interpersonal relationships while the nervous system is developing. For example, the child who loses a parent must rely heavily on the remaining parent. If the latter becomes depressed and emotionally unavailable, the child may grow up with anxiety about intimate relationships and, possibly, fear of abandonment. The concept of disorganized attachment describes the abused and neglected infant and toddler who are unable to develop a cohesive sense of self and trust of others because they experienced their mothers as either frightened (unsure of their ability to care) or frightening (through unempathic relating) (
6).
Perceptual distortions are ubiquitous
An individual’s responding to someone in the present as if that person were an important figure from the past is known as transference. In the therapeutic relationship, this phenomenon receives a great deal of the dynamic therapist’s attention. When the patient develops the ability to become aware of these distortions, it is a major therapeutic accomplishment. One way of conceptualizing the helpfulness of this type of therapy is to observe the patient’s ability to examine his or her predictable ways of responding to the therapist. Understanding this type of distortion (transference) within the therapeutic relationship elucidates sources of unhappiness and promotes greater self-understanding. When repetitive feelings and styles of interacting with others are no longer outside of the patient’s awareness, he or she can begin to feel and relate differently. Neurobiologically, this type of therapy provides new experiences, which in turn promote changes in neural circuitry.
Perceptual distortions of others are not the exclusive domain of the patient in the clinical setting, however. Clinicians, too, have feelings about and responses to patients that may be confusing at times. Although once considered unhelpful, these responses—referred to as countertransference—actually facilitate treatment enormously. When the therapist is able to appreciate why a certain feeling has arisen during a session, it provides him or her with a view of that patient’s psychic world. This understanding can in turn deepen the therapeutic process. The definition of countertransference has been broadened over time to include not only distortions, feelings, and responses to the patient that lie outside the therapist’s awareness but any reactions, feelings, and attitudes toward the patient, regardless of their source. In a sense, the presence of countertransference is an indication of the level of the therapist’s engagement. Moreover, the therapist’s self-analysis and identification of transference and countertransference enactments often facilitate the patient’s appreciation of the impact he or she has on others.
The type and forcefulness of the transference depend on the nature of the patient’s relationships with significant people earlier in life—usually parents, although siblings and other family members may also have an important role. A patient who has a primitive personality disorder and is frequently angry, hostile, and untrusting because of earlier, highly disappointing experiences is likely to manifest those feelings and responses within the psychotherapy as well. Thus, the therapist can expect that the transference will be quite intense. On the other hand, a patient can defend against true feelings sufficiently that transference is manifested in the absence of feelings. Finally, patients also have strong longings for care and affirmation from the therapist that are related to earlier significant disappointment.
Self-defeating behavior
How is it that some people never learn from their mistakes? For example, why has a man married three women in succession, each one alcoholic and abusive? Or why might a victim of childhood sexual abuse place herself in dangerous situations that might facilitate further trauma? Most people do not enjoy psychological or physical pain, yet some consistently demonstrate self-defeating or destructive behavior. People repeat unhelpful behavior in an attempt to master enduring conflict or trauma, ever hopeful that they can repair or resolve painful experiences by placing themselves once again in a precarious situation to “make it turn out differently.” Certainly, self-defeating behavior can be more subtle than the examples provided above. For instance, just as a person is about to achieve success in some endeavor, he or she behaves or does something in such a manner that recognition is withheld and success dashed. The person sabotages his or her achievement because of experiences and conflicts that are outside of awareness but that color success with danger or unworthiness.
Perhaps one of Freud’s more helpful clinical insights was the recognition that behaviors are repeated unless one becomes aware of patterns and reasons for the predictability of the behavior (
7). To paraphrase Freud, those who cannot remember certain affect-laden experiences are doomed to repeat them. One aspect of dynamic psychotherapy is to help the patient appreciate the compelling repetition of unhelpful situations or behaviors in which remembering can then replace repeating or reliving.
The emotional and the intellectual aspects in therapy
If much of a patient’s mental life takes place outside of awareness, psychodynamic psychotherapy can be helpful in promoting a process that allows both cognitive and affective components of negative experiences to be examined. Cathartic experiences alone are unlikely to provide relief or promote behavioral change. Novice dynamic psychotherapists often attempt to teach the patient the dynamics behind the psychopathology. This type of intervention invariably comes off as intellectual, premature, and distant for the patient. Because early attachment relationships are encoded as affect-laden implicit memory, psychodynamic psychotherapy replicates this experience by helping the patient examine predictable feelings and distortions within the safe therapeutic relationship. It is effective insofar as it promotes changes in neural structure that afford the patient an additional resource for feeling and behaving differently. Although dynamic therapy does not destroy memories, it restructures intense implicit memories within the context of an attuned relationship.
The interventions employed by the therapist in this type of psychotherapy have evolved over the past 50 years to encompass not only interpretive or expressive but also supportive operations. Today, psychodynamic psychotherapists conceptualize treatment interventions along a continuum that varies according to the needs of the patient at any given time. In this sense, an additional task for the clinician is to provide a balance of interventions between the supportive and the expressive domains (
8). Many mistakenly consider only interpretive, clarifying, or confronting interventions as being psychodynamic. However, the psychodynamic approach informs therapists in supportive psychotherapy that is aimed at buttressing patient deficits as well as in brief therapy (
9). Examples of supportive interventions are suggestion, reassurance, advice giving, praise, and environmental manipulation. Substantial gains can be made in supportive therapy with patients who are experiencing significant psychiatric illness. A psychodynamically informed approach is also exceptionally helpful in appreciating the meaningfulness of medication to the patient and thus plays a vital role in medication compliance (
10).
What are the tasks of the psychodynamic psychotherapist?
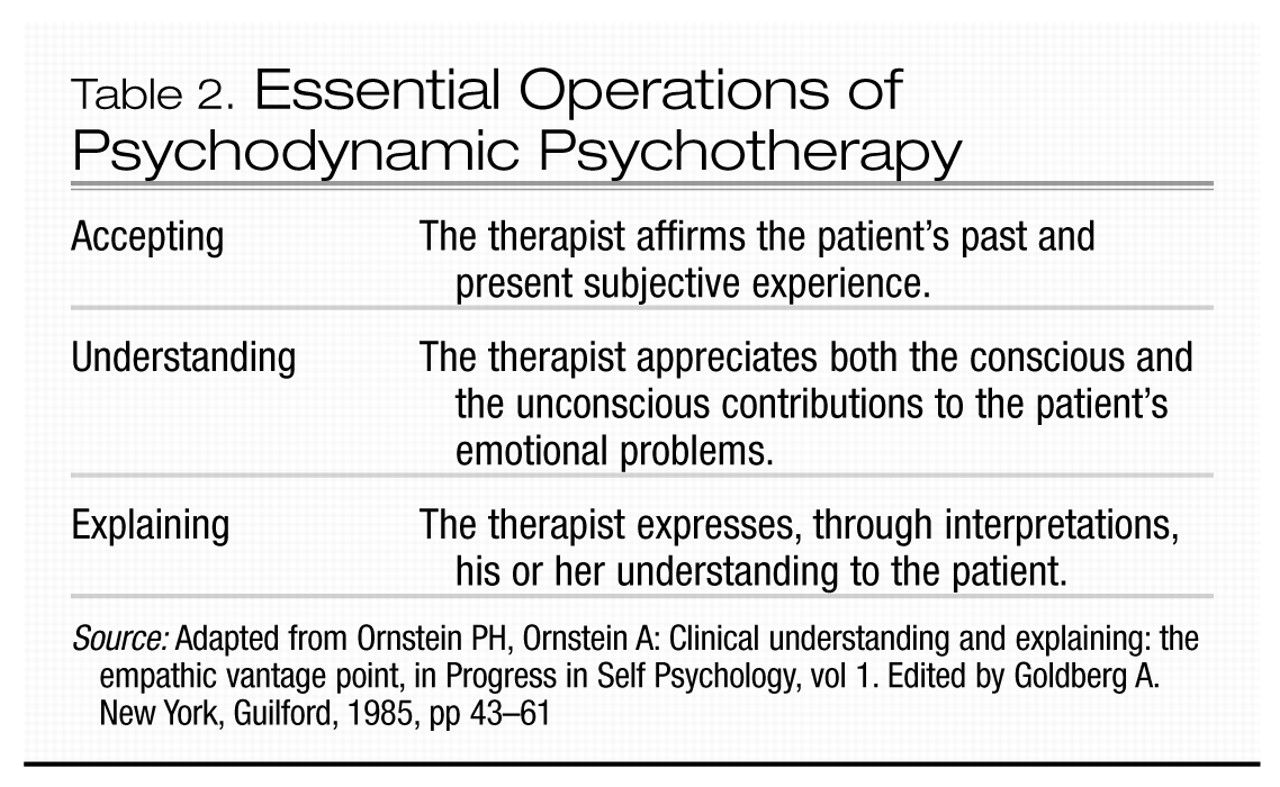
The overarching responsibility of the psychodynamic psychiatrist is to make contact with and comprehend, as thoroughly as possible, the patient’s subjective inner world in order to engage in an interpretive examination of it (
4). This type of psychotherapy comprises three operations: accepting, understanding, and explaining (Table 2).
The therapist’s accepting the patient’s subjective experience of pain and conflict implies that therapist and patient engage in the treatment to work together toward a common goal. This engagement, predicated on the therapist’s empathy and non-judgmental rapport to provide a safe forum for exploration, is commonly referred to as establishing a therapeutic or working alliance. If this engagement and collaboration are successful, the clinician will become increasingly familiar with the details of the reasons for the patient’s plight. Moreover, the patient learns through self-observation to observe and understand while also experiencing. Since much of what the therapist observes initially is outside the patient’s awareness, the second component of therapy, understanding, is the recognition of reenactments and the reliving of earlier experiences that occur in and outside of treatment. The third component, explaining, is the sharing, in timely and regulated fashion and in an empathic and interpretive mode, of what the therapist has come to appreciate about the genesis of, and the reasons for, the patient’s symptoms (
11).
Boundaries: ensuring emotional and physical safety
Much has been made so far of the requisite for the patient’s safety and security if therapy is to be effective. In a process requiring that the therapist tolerate ambiguity and complexity, some predictable and consistent procedures for the patient can be established. For example, in addition to acknowledging the goals of treatment and confidentiality, the clinician defines the framework of the working relationship through sessions of a specified duration, place of meeting, and fee for treatment. Ethically, the clinician never takes advantage of the patient to meet his or her own financial, sexual, or other personal needs. Recognition of the patient’s wish for approval from the therapist in any form (given the situation of unequal power and authority) must not be manipulated for the clinician’s benefit.
When a break in either role or boundary has occurred, it is the therapist’s duty to help the patient understand its impact, thoroughly clarifying and interpreting the meaningfulness of the event. For example, a clinician may begin to confide his or her problems and needs, transforming the therapy into an unhelpful experience for the patient. Or, in a more simple example, a psychiatrist may be late for a session. The effect of this experience must be elucidated not only to restore the process but also to deepen it through an appreciation of the specific meaning of this event for the patient.
The interpretive process
As noted, effective interpretation is predicated on a number of skills, including the therapist’s capacity to:
•
Identify a patient’s behavior and emotional patterns, especially transferences, through understanding often subtle or initially confusing communication
•
Recognize the meaning of one’s own fantasies and responses to the patient (counter-transference)
•
Maintain a verbal flow that deepens the treatment
•
Appreciate the timing and dosage of interpretations
The latter, particularly at times when the patient is experiencing intense emotion, is often referred to as the capacity to “stay in the chair” as well as to provide a “holding environment” that contains strong feelings and wishes. This skill also adds an important dimension to the safety of the treatment, since many patients, when expressing what they consider to be unacceptable and inappropriate thoughts and feelings, expect rejection, fear, or judgment from the clinician. The therapist’s capacity to be at ease with emotional intensity is a critical skill, and engaging with it is often a novel experience for many patients who feel unbearable emotional pain in the therapeutic revisiting of early isolation, trauma, and the accompanying humiliation, guilt, and shame that are so necessary for treatment success.
Similarly, the dynamic clinician abides by the principle that repeated identification and examination of reenactment and reliving of earlier experiences are vital for effective treatment and are accomplished through basic techniques of confrontation, clarification, and interpretation. This concept, working through, constitutes the middle phase of psychodynamic psychotherapy and is where the majority of therapeutic work occurs. Ultimately, working through helps the patient identify and resolve unconscious conflicts and fears that have compromised interpersonal relationships and achievement. Although brief psychodynamic psychotherapy is unquestionably effective (12), for patients with significant characterological problems, the longer the therapy is provided, the better the outcome.
The timing, dosage, and tact of the therapist’s transference interpretations are predicated on an awareness of the patient’s mental state and capacity to integrate material that has been outside of awareness. This awareness also implies an ability to appreciate the patient’s defenses, taking care not to overwhelm or traumatize a patient by insisting that he or she confront more than is tolerable. The therapist must sense when the patient will be able to accept and ultimately integrate an intervention.