Rationale for using CBT in the management of schizophrenia
Schizophrenia, as classified by Kraepelin (
1), was believed to represent an organic cerebral disease (dementia praecox) with a uniformly poor prognosis of ongoing deterioration punctuated by episodic relapse. However, Kraepelin’s sample was biased in that he only classified a subgroup of all patients with schizophrenia—patients with very severe illness and unremitting positive and negative symptoms, who had often deteriorated further owing to the effects of chronic institutionalization. Kraepelin did not include those patients who had recovered from a single episode or who were coping with relapses without deterioration, although such courses have been well described in subsequent long-term follow up studies of patients with schizophrenia (
2). Indeed, a recent 15- and 25-year follow-up of a cohort of patients with schizophrenia who remained in contact with services found that the majority achieved a favorable clinical outcome in the long term (
3).
Given this variation in outcome, a more optimistic clinical approach to the management of schizophrenia may be indicated. One of the most helpful additions to current treatment modalities would be an effective individualized psychological treatment. Cognitive-behavioral therapy (CBT) appears to have the potential to supply this missing element in the care of patients with schizophrenia. However, if findings concerning longer term outcome in schizophrenia are creating some renewed clinical optimism, this is more than counterbalanced by a number of factors currently operating in the opposite direction that could worsen prognosis. The benefits that could be realized with consistent use of long-term antipsychotic medication are usually not achieved because of poor adherence (
4). Poor adherence similarly hinders involvement in rehabilitation programs, leading to the progressively debilitating effects of repeated relapse and rehospitalization. In addition, patients who develop improved insight into the diagnostic label of schizophrenia often find this so stigmatizing that they reject treatment altogether and disengage with services or become depressed and develop suicidal ideation (
5). As well as the risk of self-harm, patients with schizophrenia usually have no paid employment and may drift into socially deprived neighborhoods, where they are increasingly the victims of violence (
6). This increased mobility and victimization can have a potent effect by increasing arousal and agitation and leading to worsening isolation, hallucinations, and persecutory paranoid delusions. Patients with schizophrenia in such situations frequently develop secondary psychiatric illness such as agoraphobia or social phobia that further exacerbate core symptoms (
7).
The problem of victimization is worsened by the increasing problem of illicit substance use (e.g., use of cannabis, heroin, amphetamine, and cocaine), which leads to reduced adherence and increased rates of relapse (
8). In addition, patients with schizophrenia usually have very poorly developed coping strategies, so that patients who begin to hallucinate tend to withdraw socially and not engage in a positive therapeutic style for help with their auditory hallucinations. In CBT, effective coping strategies can be collaboratively developed, leading to symptomatic improvement (
9).
Treatment-resistant schizophrenia is also a relatively common problem. Even when patients with schizophrenia fully adhere to antipsychotic medication regimes, up to 50% will have ongoing positive or negative symptoms (
10), with 20%–30% of people with chronic schizophrenia demonstrating very little symptomatic response to adequate trials of conventional antipsychotic medications (
11). A switch to clozapine will achieve an improved clinical outcome (e.g., 20% improvement level in 14% of cases) (
12). A recent review of atypical antipsychotics (
13) reported that there is strong evidence that clozapine is superior to conventional antipsychotics in symptom reduction in both the short and longer terms, although there was no difference in short-term relapse rates. Even with the use of optimal doses of clozapine, 40% of patients with treatment-resistant schizophrenia do not respond. An effective psychological treatment is currently the only option for such patients to ameliorate disabling symptoms.
Even when positive symptoms are well controlled with antipsychotic medication, an even greater residue of untreated depression, anxiety, obsessive-compulsive and phobic symptoms can remain, which might benefit from CBT. Many patients with treatment-resistant illness are further disabled by the use of excessively high doses of antipsychotics and polypharmacy. This often happens because, given the lack of complementary treatment options, clinicians attempt to improve efficacy by increasing medication dose at each relapse. The side effects of such polypharmacy may include a worsening of cognitive deficits and negative symptoms. These worsenings of attention, recall, and motivation are major impediments to the implementation of any effective psychological treatment in schizophrenia. Conventional antipsychotics are often less helpful with these cognitive deficits and negative symptoms and a more rational strategy may be to use low-dose atypical antipsychotics which are more cognitively sparing and more effective in the treatment of negative symptoms. A low dose of an atypical antipsychotic combined with CBT can enhance adherence and improve symptom management, and a synergistic effect might be expected when combining CBT with antipsychotics that enhance cognitive function. It is clear from the preceding discussion that there is a persuasive rationale for considering the use of psychological treatments—including CBT—in schizophrenia.
CBT as part of the spectrum of psychological treatments in schizophrenia
The standard treatment for schizophrenia in the United Kingdom is case management supplemented with support in a drop-in center or day hospital. Those who are fortunate might have access to some form of supervised work experience. The main face-to-face contact with the patient is provided by the case worker. This is normally a community psychiatric nurse, who would give a depot antipsychotic and/or check for medication side effects and encourage activities. Therefore, effective psychological treatments are not normally made available for these very highly disabled patients.
Given the current system, it is not likely that either case workers or consultant psychiatrists who are prescribing medications are really engaging with their patients to deal with their psychotic symptoms. A psychiatrist would typically spend 15 minutes once every 3 months in the outpatient clinic with the patient, and even then the time would mostly be used to monitor symptoms, medication dose, and side effects. Thus, patients may remain isolated with no practical support to help them cope with their psychotic symptoms. The standard psychosocial management of patients with schizophrenia in the United Kingdom has been reported to be well below what such disabled patients and their caregivers have a right to expect from mental health delivery teams. In contrast, CBT manuals (
14,
15) stress the importance of spending increased time with the psychotic patient, building trust and starting to test out the reality of his or her symptoms. In some patients, a clear spinoff of an improved therapeutic alliance is improved adherence. With the development of improved coping skills, the use of antipsychotic medication often becomes more acceptable and the use of illicit substances diminishes.
The consequences for an individual of developing schizophrenia are usually wide-ranging. The patient will experience distress as a direct result of the psychiatric illness. Furthermore, the illness often has a significant impact on the person’s psychological, social, and occupational functioning. Since schizophrenia is a multifaceted condition with the potential for far-reaching consequences, a number of approaches have been developed that attempt to improve functioning in these domains, including psychoeducation, social skills training, cognitive remediation, family therapy, and assertive community treatment (ACT). Before turning to a detailed discussion of the use of CBT in schizophrenia, we first briefly review the rationale and evidence for the use of these other psychosocial interventions in patients with schizophrenia and compare them with CBT. It is also true that each of the following psychosocial interventions either contributes components to a full CBT program (e.g., psychoeducation, social skills training) or could act to complement the delivery of individual CBT (e.g., family interventions, ACT, cognitive remediation).
Psychoeducation
When people are faced with serious illness or life events, there is a natural desire to try to make sense of what is going on. As a result, patients and families often request information about the nature of the illness. This need for information has been recognized in the development and delivery of psychoeducational material. Clearly, there are obvious moral, ethical, and legal reasons for providing full information about illness and treatment. Individuals suffering from schizophrenia and their families need information that will help them understand the consequences of the illness. Recent meta-analyses (
13,
16) have considered the results of 10 randomized controlled trials of psychoeducation in schizophrenia. There was considerable variation in the quality and content of the interventions, their duration, and the outcome measures that were used. The results of the meta-analyses were generally inconclusive, although clear evidence emerged that psychoeducation had no effect on preventing relapse. The effect on medication adherence, mental state, and insight did not differ from that of standard care. Thus, it appears that psychoeducation alone is of little benefit to patients suffering from schizophrenia, although it may well be helpful to patients and their families as an adjunctive component of treatment. While CBT uses educative techniques and materials, its aims go far beyond these strategies into case formulation and symptom management.
Social skills training
Patients with schizophrenia, especially those with negative symptoms, usually experience difficulties in social and occupational settings. An early psychological approach to these difficulties was to use behavioral therapy to try to normalize behavior. Social skills training was developed to help people with schizophrenia regain their social skills, improve their functioning, and hence reduce symptomatology. Argyle and Kendon viewed social functioning as a set of skills which had to be learned and practiced (
17). Social skills training, therefore, attempted to identify social skills deficits and train patients in those skills. Traditional social skills training used instruction, modeling, rehearsal, feedback, and homework to teach or retrain interpersonal skills (including eye contact, speech, and body language) that may improve social functioning.
A recent review by Pilling et al. considered the results of nine randomized controlled trials in which the control group was typically standard care (
18). Social skills training had a limited effect on improving behavioral social skills but did not generalize to improved social functioning. Overall, there was little evidence that social skills training reduced relapse rates or length of stay or improved quality of life. However, there was some limited evidence that social skills training did improve mental and social functioning (
19). The generally negative overall conclusions appeared to limit the indications for social skills training, since the outcome generally seemed to be improvements
in situ or in role playing, but little generalization to other settings (
20).
As with psychoeducation, it seemed that social skills training on its own would have little in the way of a robust impact on the management of schizophrenia. Social skills training, however, does play a role in CBT, since modeling of normal social interactions takes place within each CBT session. Homework involving graded activity scheduling takes the patient into a variety of different social situations. Reality testing of delusions involves inspecting the social behavior of others. It appears that social skills training can be enhanced in CBT by providing a personal formulation that makes the training meaningful and by focusing on the psychotic symptoms that interfere with social interactions.
Cognitive remediation
A majority of patients with schizophrenia exhibit deficits in psychological and cognitive functioning. These include impairments in memory and attention (
21), problem solving, and executive functioning (
22). Because such deficits contribute to the distress and disability associated with the illness, attempts have been made to directly target these difficulties by trying to improve performance in these areas. Repeated practice of certain tasks is prescribed in order to rebuild or develop compensatory strategies (in a similar way to the use of remediation in brain injury).
Brenner et al. developed Integrated Psychological Therapy to reduce deficits in these attentional, perceptual, and cognitive domains (
23). Five subprograms designed to ameliorate the cognitive and social deficits assumed to be characteristic of schizophrenia were run sequentially on a computer. The participants underwent 3 months of weekly sessions that targeted basic cognitive skills, as addressed in tasks such as card sorting and dealing with word problems. Social skills deficits were addressed by having the individual practice recognition of emotional expressions and interpersonal problem solving. As with behavioral improvements following social skills training, despite improvements on the target tasks following cognitive remediation, there was no evidence of generalization (
24). Pilling et al. examined five studies of cognitive remediation (
18) and the recent National Institute for Clinical Excellence (NICE) guidelines group (
13) considered the results of seven randomized controlled trials in this area. The two reviews broadly found no evidence to suggest that cognitive remediation improved outcomes in the cognitive functions of people with schizophrenia. While there may be improvements on some specific tasks, there was an absence of general improvement across tasks or generalization outside the treatment setting. Although cognitive remediation also seems inadequate on its own, there is a possibility of synergy with CBT. Improved attention as produced by remediation could help improve the quality of homework (e.g., when investigating the evidence that supports or contradicts a delusion).
Family interventions
A broad array of family interventions has been developed for use in schizophrenia, all of which aim to alter the pattern of interaction within the family or caregiver group of the person with schizophrenia in order to reduce the chance of relapse. Brown et al. reported that, following the closure of the asylums, patients with schizophrenia who returned home to live with their family fared worse than those who went to a hostel or lived alone (
25). Attempts to understand this apparently paradoxical result led to the development of a measure of Expressed Emotion (EE). EE is best viewed as the sum total of the emotional climate between the patient with schizophrenia and family or other caregivers. High EE includes critical comments, hostility, and rejection of the patient, or emotional over-involvement. Families with high EE have been found to be associated with higher relapse rates than those with low EE (48% versus 21% median relapse rates in 1 year) (
26). Although the different approaches to family therapy use varying combinations of education, support, therapy, and skills training, they all aim to reduce the extent of EE in the household.
Pilling et al. recently reviewed 18 randomized clinical trials of family interventions in schizophrenia with a total of 1467 participants published up to 1999 (
27). While the studies differed in a number of dimensions (e.g., use of control groups, type of intervention, outcome measures), a number of broad findings emerged. In particular, family interventions decreased the chance of relapse in comparison to standard care during and for a period of time following treatment. In terms of readmissions within 1 year, single family rather than group family interventions showed significant benefit. This effect was durable up to 2 years after starting treatment. Family interventions have also been found to improve treatment adherence and global adjustment. Overall, the longer the treatment (e.g., more than 10 sessions or longer than 6 months), the more efficacious the results.
While these studies demonstrated the value of family interventions, the entry requirements for participation required that the patient live with or have high levels of contact with family members with a high level of EE. Hence, the findings do not generalize to all people with schizophrenia. Nevertheless, although family therapy does not produce symptomatic improvement in the patient, it does have a potent effect in preventing relapse in a subgroup of patients at high risk of relapse. Family therapy could therefore be seen as an ideal accompaniment to individual CBT for this subgroup of patients.
Assertive community treatment
Assertive community treatment (ACT) was developed as a response to the program of closure of large psychiatric hospitals, which increased the need for intensive treatment for vulnerable psychotic patients in community settings (
28). ACT was designed to be delivered by a treatment team to high risk patients with severe mental illness. The team has a high staff/patient ratio and delivers services as needed 24 hours a day, 7 days a week; the crucial components of ACT are contact, support, and crisis management. The goals of ACT are to maintain contact, reduce symptoms and relapse, and improve social functioning and quality of life. A Cochrane review concluded that those receiving ACT were significantly more likely to remain in contact with services and less likely to be admitted to hospital (
28). There was no difference between ACT and control treatments on mental state or social functioning.
CBT could be added to the ACT program by developing symptom management strategies for delusions and hallucinations based on an individualized formulation. For example, team members could help the psychotic patient work with reality testing homework for delusions or practice strategies for coping with hallucinations.
Features of CBT for schizophrenia
The central notion of CBT is that the way in which people make sense of their environment (including psychotic experiences) influences their affect and behavior. CBT posits that people with emotional disorders such as depression see themselves or the world around them in negative and distorted ways, which lead to distress (depression and anxiety) and behavior (withdrawal) that serve to reinforce and maintain their negativity. For instance, a depressed person attempting to get ready for work spills coffee on her shirt and thinks to herself “typical of me, I am useless, I always mess things up, I may as well stop now before I make things worse.” This makes the person feel more sad, she goes back to bed, thus reinforcing the belief that she is useless. Through the use of a number of cognitive and behavioral strategies, people can be helped to evaluate and change their thoughts and behavior so that they are more adaptive and functional, thus reducing the distress they experience. CBT has been shown to be effective for conditions such as depression, and for anxiety disorders such as obsessive-compulsive disorder, post-traumatic stress disorder, and panic disorder.
Central to the CBT approach with schizophrenia is the importance of linking thoughts and feelings about current symptoms and then re-evaluating these thoughts in relation to these symptoms. However, without doubt, the crucial element in CBT for schizophrenia is the formation of a trusting therapeutic alliance. A focus on engaging the psychotic patient is maintained in every session. The patient’s model of symptom initiation and maintenance is always carefully explored before other explanations are considered. The agenda for each session is developed collaboratively but hallucinations and delusions are often high on the list. Patients often want to understand things better, feel more in control, or be able to use better coping skills. Confrontation and collusion are both avoided by maintaining a focus on framing questions and gathering evidence in a non-judgmental manner. Homework exercises are devised to test these possible explanations about the nature and cause of the psychotic symptoms Through the use of guided discovery, the psychotic patient can often give up dysfunctional explanations. For example, if the patient believes his voices come from Satan, he will probably feel more relaxed once he has considered some less frightening explanations.
Another feature of CBT for schizophrenia that distinguishes it from other types of psychosocial interventions is the importance it places on understanding the onset of psychotic symptoms using a stress vulnerability model (
29). This model emphasizes the notion that we all have the capacity to experience psychotic symptoms if we are placed under sufficient stress. However, owing to our individual genetic, physiological, psychological, and social vulnerabilities, we vary in our vulnerability to a psychotic breakdown. Another feature of CBT for schizophrenia that helps distinguish it from other more traditional CBT approaches is the emphasis placed on normalizing psychotic experiences (
14). Normalizing is also an important feature in helping patients with obsessive-compulsive disorder feel less anxious about frightening obsessional thoughts. Time is often spent looking at the prevalence of unusual experiences (e.g., voice hearing in the normal population) in order to eliminate catastrophic interpretations of what having these experiences may mean. Such normalizing explanations are reinforced through homework exercises including reading of handouts describing various phenomena, such as the relationship between sleep deprivation and hearing voices (
30). These explanations are based on an individualized formulation of the emergence of psychotic symptoms rather than being general educational statements about schizophrenia.
Patients often also have very distressing beliefs about what it means to have the diagnosis of schizophrenia. Therefore, time is also spent examining beliefs about the diagnostic label of schizophrenia to try to decatastrophize these thoughts by providing information about more optimistic views recently published concerning the long-term outcome of the illness. CBT work to improve adherence with medication arises out of these sessions attempting to understand the individual formulation of the patient’s schizophrenia. The patients view of taking antipsychotic medication should be carefully explored. Some patients are keen to comply having accepted the nature of the illness. Other patients comply despite a lack of full insight. The third group of patients either use antipsychotic medication erratically or completely refuse. Often this is because they simply cannot see the link between, for example, feeling persecuted and the taking of medicine. As understanding improves through the use of behavioral homework (e.g., diary monitoring of the activities of suspected persecutors), patients will often consider other explanations that are much more compatible with the use of medication. Such explanations often relate to the appreciation of the high levels of stress which they have been under in the prepsychotic period and subsequently. The medications can then be taken to help patients cope with stress while working on the psychotic experiences directly with CBT. Underlying attitudes often disrupt adherence, including such thoughts as “I’m not a pill person,” or “Tablets mean you are not coping well,” or “I am damaged—no tablet can help.” These attitudes are worked with directly using analysis of the evidence, positive logging, use of the belief continuum, operationalizing a negative construct, and the use of role play (
31). An example of the latter might be the patient playing the role of a doctor attempting to persuade one of his relatives to take steroids for a severe asthma attack. Sessions on adherence are sometimes best left until there has been a successful experience working on positive psychotic symptoms.
In working with delusions, it is best to begin with more superficial techniques such as peripheral questioning to outline the main areas of delusional impact. From there, behavioral homework can be used to lead to the generation of alternative explanations. Affects such as fear and anger can be reduced in intensity and avoidance tackled in session or out of session with the help of a case manager. Socratic questioning can then be useful as can work on linked underlying core beliefs (
32). An example of this might be a core belief, “I am evil,” that is linked to a religious delusion.
Case Vignette 1.
The following case vignette illustrates how the CBT therapist can introduce the process of reality testing (i.e., collaborative empiricism) with a paranoid patient.
Paranoid patient: The Mafia are observing me to decide how to kill me.
Therapist: You are obviously very frightened… there must be a good reason for this.
Paranoid patient: Do you think it’s the Mafia?
Therapist: It’s a possibility, but there could be other explanations. How do you know that it’s the Mafia?
Paranoid patient: Who else would persecute someone like this?
Therapist: Well, for us to find out together, we need to examine the evidence, although it might feel frightening to do this. I will help you to look into this a bit more.
Here the CBT therapist engages the patient in an open dialogue about the phenomena being experienced, leading to guided reality testing using straightforward behavioral exercises. In doing this, the patient’s avoidance is reduced and his anxiety starts to decrease as he considers other possible explanations, such as isolation, use of cocaine, lack of sleep, and mental illness.
By using the principle of collaborative empiricism, the therapist helped to develop a therapeutic alliance with the patient, which facilitated increased understanding of the origin and maintenance of the symptoms. Hallucinations and delusions are targets for engagement and reality testing. When receiving CBT, psychotic patients have a perceived ally who will take their experiences seriously and show an interest in what these strange and frightening experiences may mean.
Case Vignette 2.
With hallucinations, the first step is to use a voice diary to look for fluctuations in the experience of hearing voices. This is usually linked to certain behaviors or moods. The content of the voices is also recorded in the diary. Work proceeds to the development of improved use of coping and then to engaging the voices through rational responding and work on attitudes to the voices. The next vignette illustrates how the CBT therapist might use reality testing with a patient who is hallucinating.
Hallucinating patient: There are three voices talking.
Therapist: You seem to be very angry about this experience.
Patient: They are always talking about me—it is a form of torture.
Therapist: What do you think the voices might be?
Patient: I don’t know—maybe radiowaves or ultrasound.
Therapist: Can other people hear the voices? Patient: Probably… yes, they must be able to, they are so loud and clear at times.
Therapist: Well, let’s do an experiment. We will put on the tape recorder and attempt to record them.
The patient was very relieved to realize that others could not hear the voices as they often made embarrassing comments. The therapist also helped the patient to understand how the emotion of anger usually worsened the voices and how a more rational and less hostile response to the voices would make them less obtrusive. Following this, through the use of a voice diary, behavioral experiments were carried out to discover the most optimal coping strategies. In this case, being busy and being with others reduced voice intensity. This worked particularly well if the patient did not get angry with the voices. She would use rational responses including “It’s just stress… no one else can hear them… I will just keep busy or phone a friend.” CBT usually ends with the development of a clear understanding of the individualized relapse signature and action plan. To maintain benefits over the long term, booster sessions are likely to be needed (
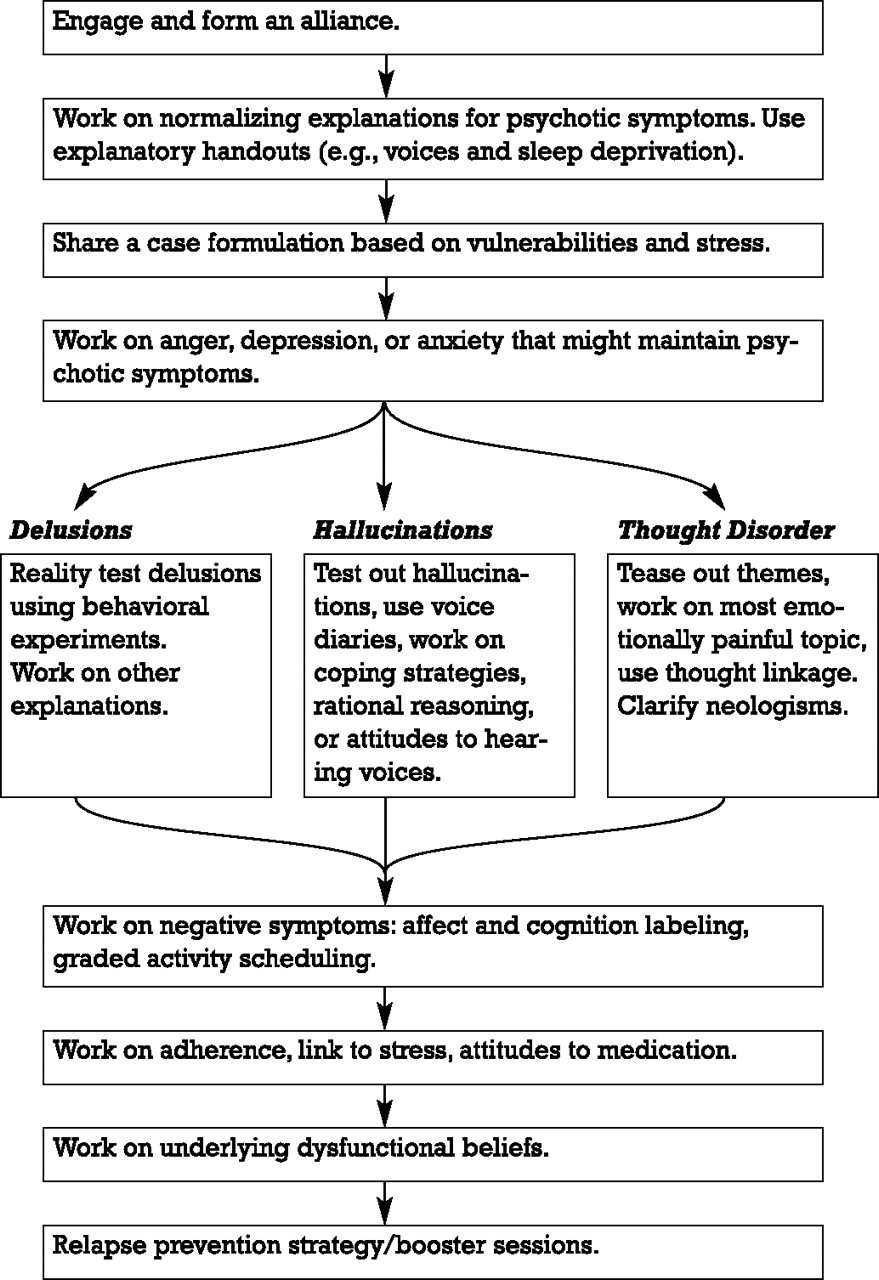
33). A full description of the techniques involved is beyond the scope of this review, but a flow chart of the various stages of therapy and basic techniques is provided in Figure 1.
Treatment studies
Recent reviews of the efficacy of CBT in schizophrenia have been positive (
27,
34), with a large effect size in residual positive symptoms at the end of therapy (ES = 0.65) and continued gains over time (ES = 0.93) (
35). The positive results in research settings are cost-effective (
36) and also appear to translate to clinical practice (
37). Benefits have been demonstrated predominantly for residual symptoms in adult patients in the community who received on average 20 sessions over 9 months, with follow-up 3–9 months later. Generally, the studies have recruited patients with longstanding or treatment-resistant psychosis, and all of the participants were also receiving antipsychotic medication.
A recent review by Pilling et al. included the results from eight randomized clinical trials (
27), while a review published by NICE in 2002 included 13 randomized clinical trials with data from 1297 patients (
13). While the studies differed on a number of dimensions, including duration of intervention, number of sessions, comparison treatment, and outcomes as well as follow-up, some clear findings emerged. CBT seemed to be particularly valuable in helping people with the overall symptoms of schizophrenia. It was reported to be more effective in improving overall symptoms at the end of treatment and at 9- to 12-month follow-up in comparison with standard care and other psychological approaches. When compared with active control interventions, such as professional befriending (emotional support and information exchange around neutral subjects), moderately strong effects were seen for both interventions at the end of therapy (
38). It is very important to note that the group who received CBT maintained their improvements, whereas the control group lost the benefits of the intervention and returned to pre-intervention levels of symptomatology. At follow-up, the CBT group were clinically significantly improved on overall symptoms, symptoms of schizophrenia, depression, and negative symptoms. There appeared to be no evidence of increased suicidal ideation or self-harming behavior in either group, but, owing to the generally low levels of suicide and self-harm within the follow-up period, there was insufficient evidence to draw conclusions. Interventions that lasted longer than 3 months were more likely to reduce the risk of relapse. The NICE review found that there was evidence that even brief CBT interventions improved treatment adherence and insight (
13).
While evidence is emerging concerning the value of CBT in schizophrenia, it is by no means compelling as yet. One possible reason for this is the speed with which this area has been developing. Because of the real and complex needs of people with schizophrenia, there has been great interest in developing and testing symptom interventions that may be of value and, consequently, a number of randomized clinical trials of CBT were undertaken in the 1990s. Tarrier et al. confirmed that the cognitive technique of coping strategy enhancement was more effective then problem solving (
39). Kuipers et al. was the first randomized trial to report a significant benefit for CBT over treatment as usual in terms of overall symptom improvement (
40). This effect proved to be durable at eighteen months (
41). Tarrier et al. tested CBT against supportive counseling and described an odds ratio of 7.8 in favor of CBT for a 50% improvement on positive symptoms (
9). However, at follow-up, CBT was no longer superior to supportive counseling, although both were superior to treatment as usual. CBT has been shown to provide additional benefit in the treatment of residual overall symptoms of schizophrenia over and above that provided by clozapine (
42). Indeed there is a firm theoretical basis for combining CBT with cognitively sparing atypical antipsychotic medication. However, the evidence from randomized clinical trials does not really tell us for which patients this approach is most suited. Generally, the trials have been done with patients with chronic symptoms, and it may be that it would be better to target people at high risk of relapse. The research data do not yet support the implementation of CBT for prodromal symptoms, first episode schizophrenia, acute relapse, those with comorbid conditions, such as substance abuse, personality disorder, or learning disabilities, or for psychotic symptoms in adolescents and elderly patients.
Furthermore, since the CBT treatment manuals for schizophrenia were developed in a pragmatic manner, they lacked the theoretical basis of an underlying cognitive model. Such models are necessary to explain the mechanisms of psychotic symptom onset and maintenance. Recently, however, more specific cognitive models for understanding what contributes to the emergence of specific symptoms, such as hallucinations and delusions, have been developed (
43–
46). These models make it possible to provide more targeted treatment approaches (
47). For instance, Beck and Rector (
43,
48) cover models for individual symptoms (hallucinations and delusions). These models describe the maintenance of hallucinations by safety behaviors and by passive attitudes leading to non-engagement. Behavioral experiments to work with these safety behaviors have been developed. It has also been shown that the content of hallucinations often corresponds to the patient’s negative automatic thoughts. Once patients have recognized this, it helps them realize that hallucinations are not externally generated. Delusions have been shown to arise without consideration of the available evidence. Disconfirmatory information searches do not occur unless the evidence is gradually considered during CBT. Similarly, a cognitive model describing the interplay between social deprivation, birth trauma, and negative core beliefs has been described for the illness of schizophrenia (
49). This has greatly helped patients to understand various factors in the causation of their own illness. Research into CBT models of symptom emergence and maintenance is ongoing.