A substantial proportion of patients with schizophrenia, estimated at 10% to 30% of outpatients, are considered resistant to standard antipsychotic treatment (
1–
3). In an inpatient population of one state psychiatric hospital, roughly one-half of patients with schizophrenia were determined to be treatment resistant on the basis of inadequate response to two different antipsychotic medication trials of at least six weeks' duration (
4). Treatment-resistant patients often exhibit persistent residual disability and impaired quality of life and incur significant health care costs despite sustained adherence with antipsychotic medications (
2).
Clozapine is the only antipsychotic medication with demonstrated efficacy for treating positive symptoms in treatment-resistant schizophrenia (
1,
5,
6). However, despite dissemination of evidence-based treatment guidelines for schizophrenia that strongly endorse the use of clozapine (
7–
9), the extent of its use in the United States remains well below the estimated prevalence of treatment-resistant schizophrenia (
10,
11).
Clinicians faced with a patient who does not respond to or cannot tolerate standard antipsychotic therapy are left with few treatment options. One option is to switch the patient to another antipsychotic agent in hopes that its receptor profile will prove beneficial (
12–
14). However, a considerable body of evidence demonstrates that first- or second-generation antipsychotic medications other than clozapine are unlikely to be efficacious in ameliorating residual positive or negative symptoms (
15–
17).
Another less conventional treatment strategy for treatment-resistant symptoms is to add a second (or third) antipsychotic medication. In addition to posing safety concerns and increasing health care costs, there is only modest empirical evidence, consisting primarily of case reports and open-label trials, for the efficacy and safety of antipsychotic combinations (
18,
19). The few randomized, double-blind studies of antipsychotic polypharmacy have involved clozapine augmentation and have reported mixed, but largely negative, results (
20–
24).
Little is known about how psychiatrists choose antipsychotic treatments for community-based outpatients who have experienced limited prior treatment response. In this report we describe how a nationally representative sample of psychiatrists modified the antipsychotic regimen for patients with treatment-resistant schizophrenia by either switching antipsychotic medications or adding another antipsychotic agent. We compared the characteristics of these two groups of patients and their treating psychiatrists and the psychiatrists' perceptions of the effectiveness of the treatment choice on clinical outcomes.
METHODS
SAMPLE
A nationally representative sample of psychiatrists was selected from the American Medical Association's Masterfile of Physicians and surveyed to assess their management of patients with treatment-resistant schizophrenia. Psychiatrists were excluded if they were in psychiatric residency training, residing outside of the United States, and older than 75 years or not involved in direct patient care. Selected psychiatrists (N = 1,150) were sent a prescreening postcard to determine whether they had treated four or more patients with schizophrenia in the last typical work month. Previous work indicates that psychiatrists who care for four or more patients with schizophrenia treat more than 90% of all patients with the disorder (
25,
26).
Excluding psychiatrists who reported treating fewer than four schizophrenia patients per month reduced the sample from 1,150 to 875. An additional 60 psychiatrists were excluded because the screening postcards were returned as “addressee unknown” and a follow-up telephone inquiry revealed no forwarding contact information. These exclusions resulted in a final sample of 815 psychiatrists who met eligibility criteria and had a deliverable mailing address. Among this sample, 473 psychiatrists responded to the survey, for a response rate of 58%.
The psychiatrists were asked to provide information on the last adult outpatient with schizophrenia in their appointment book who met the following criteria: under the psychiatrist's care for at least one year; had treatment-resistant positive psychotic symptoms in the past year, defined as delusions, hallucinations, disorganized speech, or disorganized behavior despite adherence with at least three months of treatment with antipsychotic medication; and between three and 12 months previously, the psychiatrist changed the patient's medication regimen (not including a dosage increase) to manage the treatment-resistant positive psychotic symptoms. Of the 473 survey respondents, 283 indicated that they had seen a patient who met all of these criteria. Among these 283 respondents, 20 were excluded because they were not currently giving a prescription to the patient for an antipsychotic medication, which left an analytic sample of 263 patients. Primary data collection was conducted from September 2003 to January 2004. All study procedures were approved by institutional review boards of the New York State Psychiatric Institute, the American Psychiatric Institute for Research and Education, and the University of Maryland School of Medicine.
SURVEY INSTRUMENT
Each psychiatrist provided a detailed description of the demographic and clinical characteristics of the patient, including age, gender, race, marital status, employment status, lifetime co-occurring psychiatric conditions, duration of treatment with the psychiatrist, and use of inpatient and out-patient mental health services in the past three months. Detailed information on the patient's psychopharmacologic treatment history was also provided and included all psychotropic medications prescribed immediately before the change in medication that was intended to address treatment-resistant positive psychotic symptoms.
The psychiatrist classified the type of medication change as switching antipsychotic medications (explicitly stated in the survey as not including a change in the route of antipsychotic administration or the addition of another medication), adding another antipsychotic medication or coprescription of two or more antipsychotics, or adding a nonantipsychotic psychotropic medication (for example, mood stabilizer, benzodiazepine, or antidepressant). The psychiatrist also provided his or her overall impression of the effectiveness of the change in suppressing the patient's positive psychotic symptoms, measured on a 5-point Likert response scale. Possible scores ranged from 1 to 5, with higher scores indicating greater effectiveness. In addition, the psychiatrist provided ratings of the patient's symptoms and psychosocial functioning both immediately before the medication change and three months after the medication change. Psychiatrists provided ratings of the patient's positive and negative psychotic symptoms using a Likert scale with possible values ranging from 1 to 4, with higher scores indicating more severe symptoms. Psychiatrists also provided a Global Assessment of Functioning (GAF) score (
27), representing their judgment of the patient's psychological, social, and occupational functioning. Possible GAF scores range from 1 to 100, with lower scores indicating more severe impairment. The psychiatrist also noted whether the patient had a psychiatric hospitalization in the three months before and after the medication change.
We also collected information on characteristics of the psychiatrist, including demographic traits (age, gender, and race) and practice characteristics (board certification, years in practice, geographic region, primary treatment setting, and caseload of patients with schizophrenia). In addition, psychiatrists provided information concerning the number of hours that they spent reading peer-reviewed journals, the number of meetings with pharmaceutical representatives, and the number of pharmaceutical industry-sponsored continuing education programs that they attended, all in the past month. In addition, the psychiatrists rated their familiarity with various clinical practice guidelines for the treatment of schizophrenia (for example, guidelines from the American Psychiatric Association, Schizophrenia Patient Outcomes Research Team, Expert Consensus Series, and Texas Medication Algorithm Project), using a Likert scale with possible values ranging from 1 to 7, with higher scores indicating greater familiarity with the guideline.
ANALYTIC PLAN
We compared patients for whom psychiatrists added another antipsychotic medication to their regimen with patients whom psychiatrists switched to a different antipsychotic agent. The associations between patient- and provider-related factors and the type of change in antipsychotic medication were analyzed by using chi square analyses for categorical variables and Student's t test for continuous variables.
We used analysis of covariance (ANCOVA) to analyze psychiatrists' perceptions of effectiveness (dependent variable) of the change (switch or add) in antipsychotic medication (independent variable), adjusted for patient age, gender, and race. For the analyses of psychiatrists' perceptions of changes in positive and negative symptoms and functioning (GAF) from three months before the antipsychotic change to three months after, we calculated a change score and conducted an ANCOVA on the change score as a function of the type of antipsychotic change while controlling for patient age, gender, race, and the baseline value of the dependent variable. We used logistic regression to assess whether there were differences in psychiatric hospitalization in the three months after the change in antipsychotic medication as a function of antipsychotic change type while controlling for patient age, gender, race, and psychiatric hospitalization in the previous three months. All analyses were weighted to account for survey nonresponse.
RESULTS
With respect to the last medication change made during the past three to 12 months to address treatment-resistant positive symptoms, of the 263 patients in the sample, 70 patients (27%) received an additional antipsychotic medication and 139 patients (53%) were switched to a different antipsychotic agent. Fifty-four patients (21%) who either had a nonantipsychotic psychotropic medication added to their regimen or could not be confidently classified into one of the two previous groups were excluded from the analyses.
Among the 70 patients for whom another antipsychotic agent was added, 81% received a second-generation agent other than clozapine, with aripiprazole added most frequently (23 patients, or 33%), followed by risperidone (ten patients, or 14%), quetiapine (nine patients, or 13%), olanzapine (seven patients, or 10%), and ziprasidone (eight patients, or 11%). Only one patient received clozapine adjunctively (1%), and ten patients (14%) received a first-generation agent. The added antipsychotic agent was not specified for two patients. Of the 139 patients who switched antipsychotic medications, 125 (90%) initiated treatment with a nonclozapine second-generation agent, with aripiprazole (30 patients, or 22%), olanzapine (26 patients, or 19%), and risperidone (26 patients, or 19%) each prescribed to approximately 20% of the patients and quetiapine prescribed to 17 (12%). Eleven patients (8%) switched to clozapine, whereas only one patient received haloperidol (1%). The antipsychotic agent to which two patients were switched was not specified.
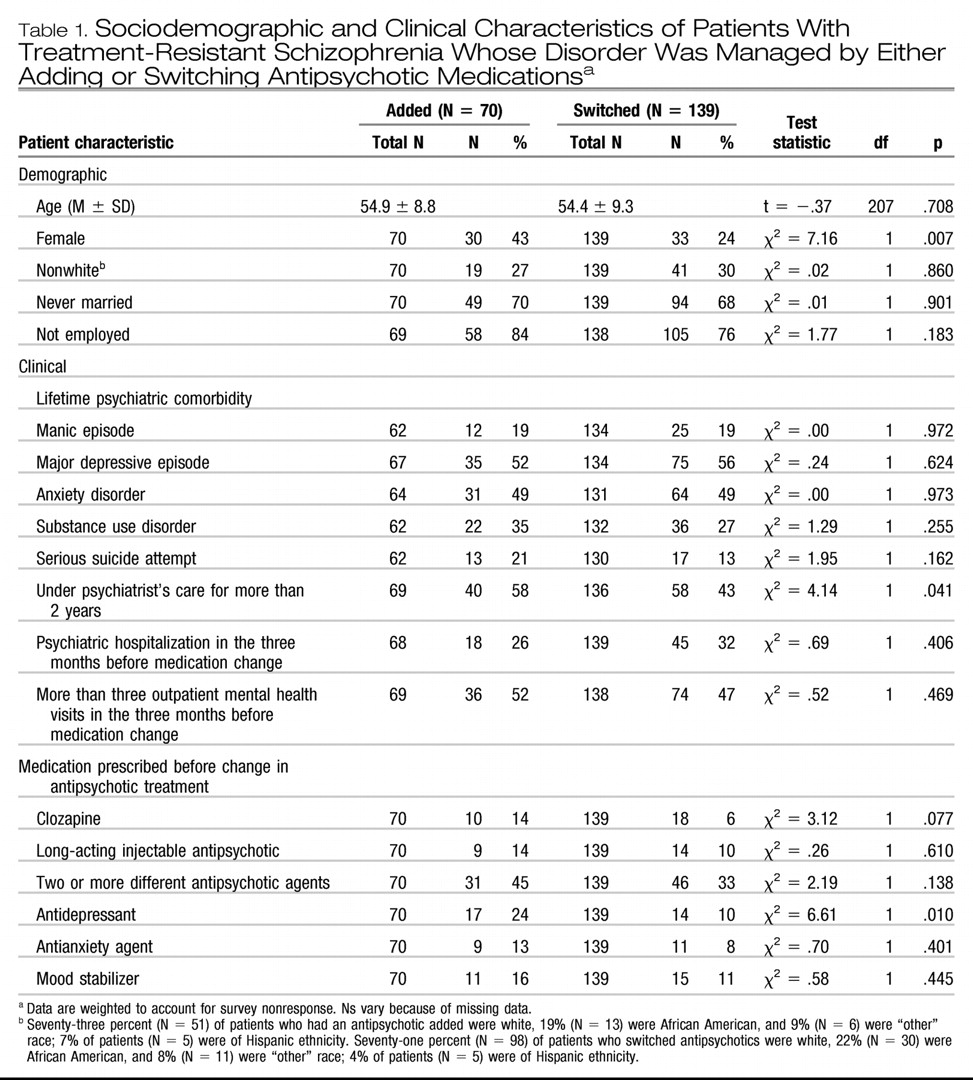
PATIENT CHARACTERISTICS AND ANTIPSYCHOTIC CHANGE
Table 1 shows results for patients who had another antipsychotic added and patients who switched antipsychotics, with respect to demographic and clinical characteristics, including psychotropic medications prescribed immediately before the change in antipsychotic medication. Compared with patients who switched antipsychotic medications, those who added an antipsychotic were more likely to be female, but no differences were seen between the groups related to patient age, race, marital status, or employment status. Overall, the mean age of patients was approximately 55 years in both groups, and a majority were white, had never been married, and were currently unemployed.
Compared with patients whose antipsychotic medication was switched, those who had another antipsychotic medication added had a similar and noteworthy burden of lifetime psychiatric co-occurring conditions and concomitant medication use. In both groups, upwards of one-half of all patients had experienced a major depressive episode or were diagnosed as having an anxiety disorder, and approximately one-third had a substance use disorder diagnosis. Past serious suicide attempt was reported for 21% of patients who added an antipsychotic medication and 13% of patients who switched antipsychotics (p = .162).
Type of change in antipsychotic medication was not related to use of inpatient or outpatient mental health services in the three months before the medication change, but patients who had an antipsychotic added were more likely to have received treatment from their psychiatrist for more than two years, compared with patients whose agent was switched (p = .041). Furthermore, patients who had an antipsychotic added were more likely than those whose antipsychotic was switched to have been given a prescription for an antidepressant medication (24% versus 10%, p = .010). However, similar proportions of both groups had been recently treated with clozapine, a long-acting injectable antipsychotic agent, multiple antipsychotic agents, antianxiety agents, or mood stabilizers (
Table 1). In a post hoc exploratory multivariate logistic regression analysis, the three patient characteristics that differed between the groups in bivariate comparisons remained significant independent predictors of adding versus switching antipsychotic medications.
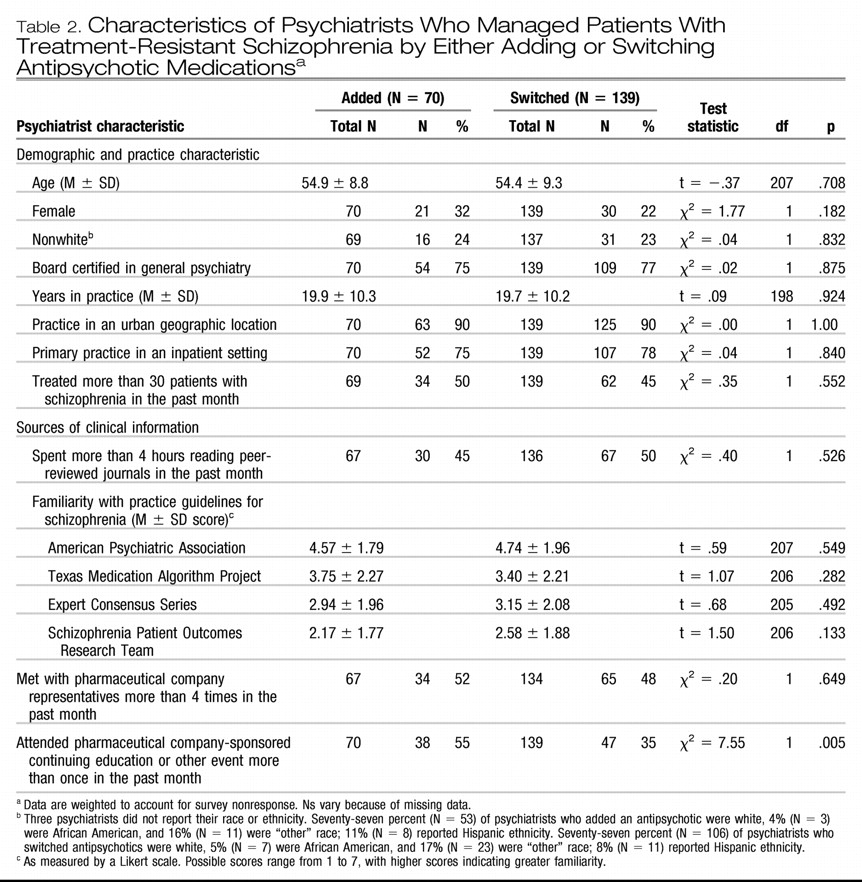
PSYCHIATRIST CHARACTERISTICS AND ANTIPSYCHOTIC CHANGE
As shown in
Table 2, psychiatrists who managed one of their patients with schizophrenia with treatment-resistant positive psychotic symptoms by either adding an antipsychotic or changing antipsychotic agents were similar in terms of their demographic and practice characteristics. A majority of all psychiatrists were male, white, and board certified, with a mean age of approximately 55 years in both groups. Most practiced in an urban area and in inpatient treatment settings. About one-half of both groups treated more than 30 patients with schizophrenia each month. Approximately one-half of psychiatrists from both groups reported spending more than four hours in the past month reading peer-reviewed journals, and they provided similar ratings of their familiarity with practice guidelines for schizophrenia. Although both groups reported similar levels of contact with pharmaceutical industry representatives, a larger proportion of psychiatrists who added, rather than switched, antipsychotics had attended more than one industry-sponsored continuing medical education session in the past month (p = .005).
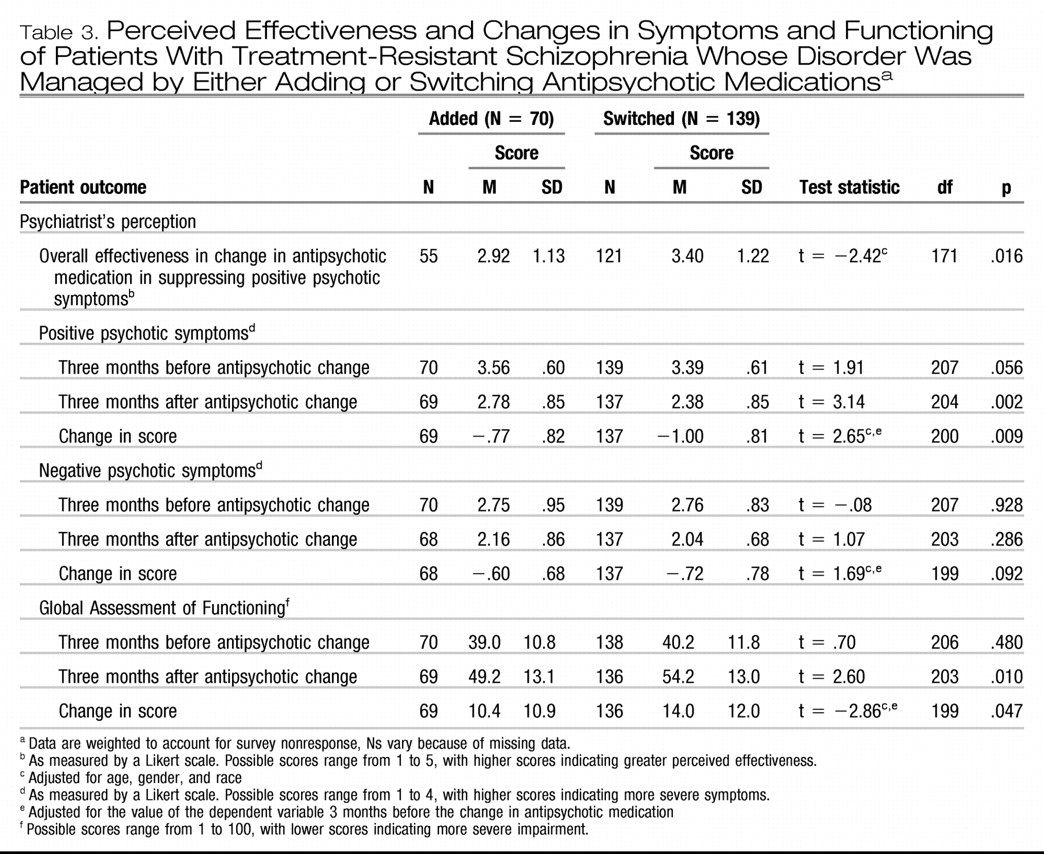
EFFECTIVENESS OF ANTIPSYCHOTIC CHANGE
As shown in
Table 3, psychiatrists who chose to switch antipsychotic medications perceived this strategy to be more effective, compared with psychiatrists who prescribed an additional antipsychotic for treatment-resistant positive psychotic symptoms (p = .016). Psychiatrists who switched antipsychotics also observed significantly greater reductions in positive psychotic symptoms (p = .009) and greater improvements in GAF scores (p = .047) among their patients, compared with psychiatrists who added another antipsychotic. These results were adjusted for patient age, gender, race, and the respective symptom or functioning measure three months before the medication change. There were no differences in psychiatrists' observed changes in negative psychotic symptoms as a result of the different medication management strategies.
Three months before the change in antipsychotic medication, a similar proportion of patients in each group received inpatient psychiatric care (
Table 1). However, during the three months after the change, a significantly larger proportion of the patients who had an antipsychotic added (13 patients, or 19%), rather than switched (12 patients, or 9%), received inpatient psychiatric care (χ
2 = 4.53, df = 1, p = .033). Logistic regression analysis showed that patients who had another antipsychotic added were three times as likely as patients who switched to a different antipsychotic agent to be hospitalized after the medication change (adjusted odds ratio = 3.05, 95% confidence interval = 1.08–8.56), when the analysis adjusted for patient age, gender, race, and psychiatric hospitalization in the prior three months.
DISCUSSION
In this study, we found that more psychiatrists responded to treatment-resistant psychotic symptoms among their patients with schizophrenia by switching rather than adding a new antipsychotic. Although psychiatrists in both groups found their approach to be only modestly effective, those who switched agents perceived that their strategy was more effective and resulted in greater improvements in positive psychotic symptoms and functioning, compared with psychiatrists who chose to prescribe an additional antipsychotic medication. Corroborating the treating psychiatrists' subjective assessments of symptoms and functioning, patients whose antipsychotic medication was switched also had a significantly lower likelihood of psychiatric hospitalization after the medication change than patients who had another antipsychotic added. Our results are consistent with several recent randomized controlled trials (
20–
24) that indicate coprescription of antipsychotic medications has limited effectiveness in the management of residual psychotic symptoms among patients with schizophrenia. Our results are also consistent with two case-control studies (
28,
29) of inpatients that found treatment with a variety of antipsychotic combinations conferred no benefit over treatment with monotherapy for symptoms, functioning, or length of hospital stay.
We found little evidence that patients given a prescription for an additional antipsychotic medication in routine practice were more seriously ill than those who had their antipsychotic switched to a different agent. Patients in both groups received similar psychiatrists' assessments of symptoms and functioning before the change in medication and did not differ on most other demographic and clinical characteristics.
Among the few differences in patient characteristics, female patients constituted a larger proportion of the patients who had an antipsychotic added, compared with those who had their antipsychotic switched. The reasons for this gender difference are unclear, especially in light of the generally lower tolerability of antipsychotic medications among women, compared with men (
30,
31). In addition, a greater proportion of the group that added rather than switched antipsychotic medications had the same psychiatrist for more than two years. It is possible that adding multiple antipsychotic medications tends to occur later in the course of treatment with one psychiatrist as switching strategies become exhausted. Unfortunately, detailed data concerning past antipsychotic treatment trials were not available to evaluate this hypothesis.
Although the study groups did not differ in their likelihood of having comorbid major depression, proportionately more patients who had an antipsychotic added rather than switched were treated with an antidepressant medication. The reason for this difference remains unknown, although it may reflect a general tendency of psychiatrists who add antipsychotic medications to engage in more aggressive pharmacological management.
The characteristics of the two groups of psychiatrists were similar in many respects. One potentially important exception is that compared with psychiatrists who switched antipsychotic medications, those who added another antipsychotic reported more frequent attendance at pharmaceutical industry-sponsored educational programs. Although this finding requires further exploration, interaction with pharmaceutical representatives and participation in continuing education programs sponsored by the industry has been found to influence prescribing behaviors (
32).
In our study, patients who had an antipsychotic switched and those who had one added tended to receive one of the recently approved and more heavily marketed and prescribed second-generation antipsychotic medications. The newest antipsychotic medication, aripiprazole, was the agent most frequently prescribed as adjunctive antipsychotic treatment. Only a small minority (8%) of patients with treatment-resistant positive symptoms who switched antipsychotic medications were switched to clozapine. Clozapine is the only antipsychotic medication with demonstrated efficacy for treatment-resistant schizophrenia, despite the required hematologic monitoring for agranulocytosis and less attractive side-effect profile (
33). Still, support for the benefits of clozapine comes from the recently published phase 2 of the Clinical Antipsychotic Trials for Interventions Effectiveness study, showing that clozapine is more effective than switching to olanzapine, risperidone, or quetiapine among patients who discontinue treatment because of lack of efficacy with a different second-generation agent (
34). Our results are consistent with other reports of underuse of clozapine in the United States (
35) and support recent calls to enhance service systems to facilitate its use among appropriate patients (
34).
The study presented here has several limitations. First, the ratings of clinical status and treatment were provided retrospectively by the treating psychiatrists. Although this method may introduce measurement bias, we sought to enhance the validity of the outcomes assessments by selecting the GAF, a commonly used measure of psychosocial function, and an objective measure of relapse (hospitalization) (
36). Second, as indicated above, no information was available concerning treatment history in the period immediately before the medication change reported in this study. Third, although we crafted language in the survey to assist psychiatrists in correctly describing the medication change, we cannot guarantee that some patients undergoing temporary cross-titration with two or more antipsychotics during a switch were misclassified as having another antipsychotic added. Also, because this is an observational rather than an experimental study, we cannot exclude the possibility that the study groups differed with respect to important but unmeasured factors that may account for the group differences in outcome. Finally, a considerable proportion of eligible psychiatrists declined to participate in the study, and many who did respond were not able to identify and report on a patient meeting the study's inclusion criteria. Consequently, we cannot exclude the possibility that selection biases have distorted the observed associations despite our attempt to use nonresponse weights to account for the bias.
CONCLUSIONS
This study represents one of the first investigations of the prescription decision-making process in treatment-resistant schizophrenia. Our findings suggest that despite the increasing frequency with which antipsychotic combinations are prescribed, psychiatrists do not perceive this treatment strategy to be particularly effective in terms of reducing psychotic symptoms, improving overall functioning, or reducing inpatient recidivism. Our findings underscore the need to disseminate and implement existing evidence-based therapies into routine clinical practice and to identify new treatments with favorable risk-to-benefit profiles to address treatment-resistant psychotic symptoms.