This is not to say that we intend to recommend specific intervention models, as the literature does not currently support this. The heterogeneity of traumatic events and their aftermath defies any specific guidelines, and there is a need for flexibility of interventions and adaptations to specific circumstances. We, therefore, address this issue by asserting several general principles for successful intervention or policies, attempting to formulate these principles in a way that will allow their smooth translation to specific circumstances. Thus, we believe that there are central elements or principles of interventions, ranging from prevention, to support, to therapeutic intervention that are supported by the empirical literature and can be termed “evidence-informed.” It is highly unlikely that we will have an adequate representation of randomized controlled trials of interventions for major disaster events or terrorist attack in the near to mid-term future, if ever. Therefore a major step in promoting the development of effective, efficient, and sustainable interventions is to ensure that, to the extent possible, they are informed by empirical evidence and meet standards of reasonable support from published studies of relevance to disaster environments.
There are several ways in which stressful events may reach traumatic proportions for individuals and communities. First, the sheer physical, social, and psychological demands of situations involving mass casualty may be overwhelming—either directly (by the extent of pain, injury, destruction or devastation) or because of their grotesque and incongruous elements (e.g., bodily disfigurement, school children being starved or massacred, people jumping from the burning Twin Towers, bodies floating in a New Orleans street) or by their symbolic implications (beheading of prisoners) or personal relevance (e.g., assuming that an act of terror could reach one's own neighborhood) (
Reissman, Klomp, Kent, & Pfefferbaum, 2004). Second, the devastation of resources can impoverish the capacity of individuals and communities' to cope with a traumatic situation and recover from its consequences, especially where individuals or communities already have depleted psychosocial and economic resources due to prior trauma, a history of psychiatric disorder, or socioeconomic disenfranchisement (
Hobfoll, 1998). The loss, or threatened loss, of attachment bonds that occurs in disasters and instances of mass casualty comes close in its intensity and effect to the previous elements of witnessing horrors and direct personal threat. Many traumatic events involve powerful reactivation of attachment systems and ensuing agony and distress (such as looking for relatives in the rubble of an earthquake or searching casualty lists). Third, and linked to the former, is the loss of territory, or safety within a territory—either via relocation—or indirectly, as people's previously secure base is infiltrated by threat and horror. In many instances of disaster and mass casualty, the ongoing violence, aftershocks, massive failure to provide aid, and the secondary losses that follow the initial phase mean that there may be no clearly demarcated period that can be termed post-trauma. Finally, the potentially damaging effects of traumatic events on people's sense of meaning, justice, and order often have extremely stressful effects. Many trauma survivors struggle with challenges to sense of meaning and justice in the face of shattered assumptions about prevailing justice in the world due to the way in which they were either exposed to traumatic events (e.g., being sent to a war they perceive as senseless, being an innocent victim) or treated during the post-traumatic aftermath (e.g., via discriminatory distribution of resources). It is on the basis of these principles that we came to seek, identify, and describe the basic, practical recommendations that follow.
PROMOTION OF SENSE OF SAFETY
The principle of promotion of sense of safety comes from several avenues of investigation relating to both objective reality and perceived reality. It is the nature of disasters and mass violence that people are forced to respond to events that threaten their lives, their loved ones, or the things they most deeply value (
Basoglu, Salcioglu, Livanou, Kalender, & Acar, 2005;
Briere & Elliot, 2000;
de Jong, 2002a,
2002b;
Hobfoll et al. 1991;
Ursano, McCaughey, & Fullerton, 1994;
van der Kolk & McFarlane, 1996). Young children, parents, and caretakers are especially challenged by a mutual sense of disruption of a “protective shield” that underlies much of early child development and family life (
Pynoos, Steinberg & Wraith, 1995). As such, it is not surprising that negative post-trauma reactions are common in large percentages of populations, across the full spectrum of age ranges that are exposed to disasters or mass violence. Hence, it is not unexpected that disaster-affected populations have been found to have high prevalence rates of mental health problems, including acute stress disorder, posttraumatic stress disorder (PTSD), depression, anxiety, separation anxiety, incident-specific fears, phobias, somatization, traumatic grief, and sleep disturbances (
Balaban et al., 2005). These negative post-trauma reactions tend to persist under conditions of ongoing threat or danger, as studies in a variety of cultures have shown (
de Jong et al., 2001;
de Jong, Mulhern, Ford, van der Kam, & Kleber, 2000;
Neria, Solomon, & Dekel, 2000;
Porter & Haslam, 2005;
Yzermans & Gersons, 2002). To the extent, however, that safety is introduced, these reactions show a gradual reduction over time (
Ozer, Best, Lipsey, & Weiss, 2003;
Silver, Holman, McIntosh, Poulin, & Gil-Rivas, 2002). Moreover, even where threat continues, those that can maintain or re-establish a relative sense of safety have considerably lower risk of developing PTSD in the months following exposure than those who do not (
Bleich, Gelkopf, & Solomon, 2003;
Grieger, Fullerton, & Ursano, 2003).
When people are confronted with ongoing threats of this magnitude they will naturally respond with deeply embedded psychophysiological and neurobiological reactions that underscore the brain's cortical and subcortical responses as well as peripheral fight, flight, or freeze reactions (
Ursano et al., 1994;
van der Kolk & McFarlane, 1996). Biological adaptation to extreme stress is necessary for survival in a Darwinian sense (
Hobfoll, 1998;
van der Kolk & McFarlane, 1996), and hence, it is not surprising that these reactions are deeply embedded in the brain (
Charney, Friedman, & Deutch, 1995;
Panksepp, 1998;
Yehuda, 1998;
Yehuda, McFarlane, & Shalev, 1998). There is also a developmental neurobiology to their ontogenesis (
Pynoos, Steinberg, Ornitz, & Goenjian, 1997). Translational research highlights that promoting a sense of safety is essential in both animals and humans to reduce these biological responses that accompany ongoing fear and anxiety (
Bryant, 2006). The implication of this pattern is that promoting safety can reduce biological aspects of posttraumatic stress reactions (
Bryant, 2006).
Parallel to these physiological reactions, cognitive processes that inhibit recovery also occur and are exacerbated by ongoing threat.
Foa (1997) has suggested that spontaneous or natural recovery following exposure to a trauma is associated with maintenance of a balanced view about the dangerousness of the world. A belief that “the world is completely dangerous” is held to be a primary dysfunctional cognition that mediates development of PTSD (
Foa & Rothbaum, 1998). Because trauma memories are often encoded in the context of overwhelming emotion and confusion,
Ehlers and Clark (2000) posit that such memories are easily and involuntarily triggered by a wide range of reminders and often subjectively feel as if they are happening “right now,” even if safety is restored. This model holds that corrective information is needed in the aftermath of trauma to ensure that individuals can appraise future threat in a realistic manner. Consistent with this view, convergent evidence indicates that people who are likely to develop subsequent disorders are more likely to exaggerate future risk (
Ehlers, Mayou, & Bryant, 1998;
Smith & Bryant, 2000;
Warda & Bryant, 1998). If actual safety is not restored, reminders will be omnipresent and contribute to an ongoing sense of exaggerated threat, preventing a return to a psychological sense of safety (
Ehlers & Clark, 2000;
Nortje, Roberts, & Moller, 2004).
There are several intervention strategies that will promote a psychological sense of safety. These can be instituted on individual, group, organization, and community levels.
On an individual level, studies of exposure therapy have found that a key to therapeutic success is to interrupt the post-traumatic stimulus generalization that links harmless images, people, and things to dangerous stimuli associated with the original traumatic threat (
Bryant, Harvey, Dang, Sackville, & Basten, 1998;
Foa & Rothbaum, 1998;
Gersons, Carlier, Lamberts, & van der Kolk, 2000;
Resick, Nishith, Weaver, Astin, & Feuer, 2002). This is done through both imagined exposure and real-world, in-vivo exposure in ways that re-link those images, people, and events with safety (“The bridge that collapsed was threatening, but all bridges are not” “That night was unsafe, but all nights are not unsafe.”). Interventions have also utilized reality reminders, teaching contextual discrimination in the face of trauma and loss triggers, assisting in developing more adaptive cognitions and coping skills, and grounding techniques to enhance people's sense of safety (
Hien, Cohen, Miele, Litt, & Capstick, 2004;
Najavits, 2002;
Najavits, Weiss, Shaw, & Muenz, 1998;
Resick & Schnicke, 1992). Such interventions have been used for individuals and small groups and can be applied after screening in post-disaster and mass violence situations. When working with children, in addition to utilizing these components, the reversal of regression in their ability to discriminate among indications of danger is another core therapeutic objective (
Goenjian et al., 1997;
Goenjian et al., 2005;
Layne et al., 2001;
Pynoos et al., 1995).
Evidence from frontline treatment of trauma in combat situations also supports the centrality of promoting safety and has implications for individual and more organizational and large group intervention. Hence, safety must be approached as a relative state, and even in disaster or combat zones where total safety cannot be achieved, the extent that safety is enhanced will aid people's coping. In studies of combatants in Israel, one of the key principles of immediate treatment of combatants who were experiencing acute stress reactions was bringing them to relative safety, out of the line of fire (
Solomon & Benbenishty, 1986;
Solomon, Shklar, & Mikulincer, 2005). This breaks the automaticity of the threat-survival physiology and associated cognitions (
Solomon et al., 2005).
On a public health level, how to establish safety may appear obvious, in that we should bring people to a safe place and make it clear that it is safe. The promotion of a sense of safety is very similar to Bell's and Pynoos's principle of reestablishing the protective shield, which is a key principle of their respective work in community and disaster psychiatry on health behavior change in large populations and communities (
Bell, Flay, & Paikoff, 2002;
Pynoos, Goenjian, & Steinberg, 1998). In reality, the restoration of confidence in a protective shield in both adults and children requires repeated attention and can be a slow process (
Lieberman, Compton, Van Horn, & Ippen, 2003;
Pynoos et al., 2005).
Interventions to enhance safety must include a social systems perspective. Although social support has a major positive impact, as we will detail, in the aftermath of large-scale community trauma it may have the opposite impact. When complete information about mass trauma is lacking (a common occurrence following disasters and mass violence), people tend to share rumors and “horror stories” about the event.
Hobfoll and London (1986) termed this the “pressure-cooker” effect. While this is probably intended to gain support, it has been found that increasing doses of this type of “support” are positively correlated with psychological distress (
Hobfoll & London, 1986;
Pennebaker & Harber, 1993). In fact, those individuals who are sought out as support providers may be most vulnerable to this additional over-exposure. Intervention should, therefore, recommend limiting the amount of this type of talking about the trauma if doing so makes one more anxious or depressed.
Related to the factor of social support are worries concerning attachment networks. Information about the survival and safety of friends and relatives is the first to be sought during the immediate aftermath of disasters and terrorist acts (see, for example,
Bleich et al., 2003). Because fears concerning the safety of relatives may be greater than those concerning the self, intervention must aid identification of loved ones and their condition as an utmost priority. Thus, even prior to people's need to be connected to others for social support as we discuss later, their concern for the safety of their family may be even more primary.
Safety, by extension, involves safety from bad news, rumors, and other interpersonal factors that may increase threat perception. In that sense, providing continuous and unbalanced information about hypothetical sources of additional stress (e.g., enumerating all the possible scenarios of terrorism, such as poisoning wells, destroying crops) undermines survivors' sense of safety. Leadership must provide an accurate, organized voice to help circumscribe threat, and thereby increase the perception of safety where there is no serious extant threat (
Shalev & Freedman, 2005).
Finally, media and the use of media by public officials are important foci of intervention. President Bush's speech and actions following the events of September 11th were largely seen as increasing Americans' belief in his leadership (
Bligh, Kohles, & Meindl, 2004). However, a societal source of fear regarding safety in the aftermath of mass violence can also include government-issued messages. Although the intent of such messages is to keep the public informed and to increase their knowledge as to how to act, if not carefully orchestrated, those messages may increase anxiety and make people less clear about what is expected of them. Unfortunately, such messaging is also often used to serve political ends. For instance, it has been suggested that one factor contributing to George W. Bush's election in 2004 was the media attention, and the attention focused on terrorism by those seeking election—given to imminent terrorist threats (
Cohen, Ogilvie, Solomon, Greenberg, & Pyszczynski, 2005). This evidence highlights that communities may have difficulty maintaining a sense of safety in the aftermath of mass violence if government agencies and elected officials strategically elevate the community's sense of danger because this provides a political advantage. One might think that the media and politicians are beyond our influence, but organizations such as the American Psychological and American Psychiatric Associations, and their counterparts in other countries, are often looked to in times of mass trauma and should be ready to address these questions and take a stand on use of the media to produce fear or sensationalize. Likewise, broadcasting is controlled by laws and governing boards (e.g., Federal Communications Commission) that should be prepared prior to disaster or terrorism occurrence on such issues.
The media may be another significant societal-level obstacle to establishing a sense of safety. Media may report events in ways that inadvertently decrease a sense of safety or that are intentionally unclear as to the degree of safety because marketing research suggests that uncertainty and fear promote increased viewing of the news. Additionally, it is common for media to repeatedly display images of threat that can serve to reduce the community's perception of safety. Thus, media-related factors may impede recovery since a dose-response effect has been found in multiple studies linking exposure to televised images of the traumatic event to greater psychological distress (
Ahern et al., 2002;
Nader & Pynoos, 1993;
Neria et al., 2006;
Pfefferbaum et al., 2002;
Schlenger et al., 2002;
Silver et al., 2002;
Torabi & Seo, 2004). Although it is difficult to determine the causal relationship between media viewing and fear, these findings are consistent with the proposal that media exposure influences fear in the community. Additionally, young children are likely to have difficulty understanding that an event has ended, believing that replays on the local news represent new incidents or continued threat (
Fremont, 2004;
Lengua, Long, Smith, & Meltzoff, 2005;
Pfefferbaum et al., 2002). For this reason, media should be educated that enhancing safety perceptions in a community can be achieved by media coverage that strategically conveys safety and resilience rather than imminent threat. Additionally, effective mental health response following disasters should include encouraging individuals to limit exposure to news media overall and to avoid media that contain graphic film or photos if they are experiencing increased distress following viewing. This includes education of parents regarding limiting and monitoring news exposure to children.
PROMOTION OF CALMING
Exposure to mass trauma often results in marked increases in emotionality at the initial stages. Some anxiety is a normal and healthy response required for vigilance. Hence, there is no reason to be alarmed at somewhat heightened levels of arousal or, paradoxically, numbing responses that provide some needed psychological insulation during the initial period of responding (
Breznitz, 1983;
Bryant, Harvey, Guthrie, & Moulds, 2003). The question is whether such arousal or numbing increases and remains at such a level as to interfere with sleep, eating, hydration, decision making, and performance of life tasks. Such disruptions of necessary tasks and normal life rhythms are not only impairing, but potential precipitants of incapacitating anxiety that may lead to anxiety disorders. Moreover, extremely high levels of emotionality, even during immediate post-trauma periods, may lead to panic attacks, dissociation, and may portend later PTSD (
Bryant et al., 2003;
Shalev et al., 1998). Further, although initial arousal and numbing may be adaptive, prolonged states of heightened emotional responding may lead to agitation, depression, and somatic problems (
Harvey & Bryant, 1998;
Shalev & Freedman, 2005). In addition, in some studies heightened heart rate in the early post-trauma phase has been demonstrated to be associated with long-term PTSD symptoms (
Bryant et al. 2003;
Shalev, 1999). Given such problems, it is important that intervention include the essential ingredient of calming.
More homogeneous studies of personal trauma, such as rape, demonstrate that the majority of individuals initially show symptoms that, if persistent, would be indicators of PTSD. This initial severe emotionality is a normal way of responding. However, most individuals return to more manageable levels of emotions within days or weeks. Those that do not return to these lower manageable levels of responding are at considerable risk for eventual development of PTSD (
McNally et al., 2003;
Shalev & Freedman, 2005). Further, even if their hyperarousal, increased emotional lability, and distress symptoms do diminish, such heightened emotional states are likely to interfere with sleep (
DeViva, Zayfert, Pigeon, & Mellman, 2005;
Ironson et al., 1997;
Meewisse et al., 2005) and daily functioning, such as concentration and social interaction. This hyperarousal can have a major effect on risk perception, such that the external environment is perceived as potentially harmful beyond any proportion to the available objective information. As described above, once a context or a situation has been perceived as threatening, neutral or ambiguous stimuli are more likely to be interpreted as dangerous. In response to elevated levels of fear, a process of avoidance may begin that initially may be adaptive. However, as the avoided stimuli increase in number and type, the ensuing avoidance may strongly interfere with individuals' and families' capacities to effectively engage in salutogenic human interactions in the aftermath of disasters. Finally, physiological demands may compete with other mental resources on priorities in attention and action, causing decrements in functioning precisely when optimal functioning is so critical.
A major reason why psychological debriefing (such as Critical Incident Stress Debriefing) has been criticized in recent years is that it serves to enhance arousal in the immediate aftermath of trauma exposure. There is convincing evidence that these early interventions are not effective in preventing subsequent psychological disorder (
McNally et al., 2003). It has been suggested that requiring people to ventilate in the immediate aftermath of trauma can increase arousal at the very time that they are required to calm down and restore equilibrium after the traumatic experience. It is possible that this increase in arousal may be the cause of debriefing exacerbating some people's stress reactions after trauma (
Bisson, Jenkins, Alexander, & Bannister, 1997;
Hobbs, Mayou, Harrison, & Worlock, 1996).
The Expert Consensus Guideline Series: Treatment of Posttraumatic Stress Disorder notes that anxiety management can be a key psychotherapeutic treatment for patients (
Foa et al., 1999;
National Institute for Clinical Excellence, 2005). Most successful trauma-related psychosocial and psychopharmacological treatments target calming of extreme emotions associated with trauma as an essential therapeutic element (
Davidson, Landerman, Farfel, & Clary, 2002;
Foa, Keane, & Friedman, 2000;
Friedman, Davidson, Mellman, & Southwick, 2000), as does frontline treatment of combatants with acute stress reactions (
Solomon, 2003). Even treatments that focus on exposure do not conclude until the individual has attained a state of mastery or calming over the aversive memory (
Foa & Rothbaum, 1998;
Jaycox, Zoellner & Foa, 2002). They allow for increased emotionality during early phases of treatment, but provide individuals with the skills to achieve a relaxed state as a critical treatment goal.
Treatments for calming range from direct, targeted treatments to more indirect approaches. Direct approaches are generally recommended for those with severe agitation and “racing” emotions or extreme numbing reactions. Therapeutic grounding is used to remind individuals that they are no longer in the threat-trauma condition and that their thoughts and feelings are not dangerous in the way the disaster or terrorist attack was. This is important because those developing PTSD are likely to be re-experiencing the trauma in their imaginations and dreams. Breathing retraining is a simple technique that is used to get individuals to breathe deeply and avoid hyperventilating or dissociating (
Foa & Rothbaum, 1998). Deep breathing counters anxious emotionality. In one novel intervention, following the threat of attack, a phone-based intervention successfully employed diaphragmatic breathing and a modified cognitive-restructuring technique to reduce anxiety in Israeli citizens (
Somer, Tamir, Maguen, & Litz, 2005). Deep muscle relaxation is a more involved, but still simple, treatment for teaching relaxation and is included in stress inoculation training (
Bernstein & Borkovec, 1973;
Foa & Rothbaum, 1998;
Veronen & Kilpatrick, 1983). Yoga also calms individuals and lowers their anxiety when facing traumatic circumstances, while muscle relaxation and mindfulness treatments that help people gain control over their anxiety are being applied that draw from Asian culture and meditation (
Carlson, Speca, Patel & Goodey, 2003;
Cohen Warneke, Fouladi, Rodriguez, & Chaoul-Reich, 2004;
Somasundaram & Jamunantha, 2002;
van de Put & Eisenbruch, 2002). Similarly, imagery and music paired with relaxed states has been found to be successful in calming and aiding sleep among those threatened by cancer (
Roffe, Schmidt, & Ernst, 2005).
Although there has been little systematic research on pharmacological approaches to induce calming, there are also a number of medications that hold promise for this purpose, such as anti-adrenergic agents, antidepressants, and conventional anxiolytics (
Friedman & Davidson, in press;
Pitman et al, 2002). At the same time, these must be used cautiously, for although benzodiazepines may have an initial calming effect, they may increase likelihood of later PTSD (
Gelpin, Bonne, Peri, Brandes, & Shalev, 1996).
Stress inoculation training (SIT) is a type of cognitive behavioral therapy (CBT) that can be thought of as a toolbox, or set of skills, for managing anxiety and stress (
Hembree & Foa, 2000;
Meichenbaum, 1974). SIT typically consists of education and training of coping skills, including deep muscle relaxation, breathing control, assertiveness, role playing, covert modeling, thought stopping, positive thinking, and self-talk. The rationale for this treatment is that trauma-related anxiety can generalize to many situations (
Rothbaum, Meadows, Resick, & Foy, 2000). A number of studies have found SIT to be effective both with women who have survived sexual assault and accident survivors (
Foa, Rothbaum, Riggs, & Murdock, 1991;
Hickling & Blanchard, 1997;
Kilpatrick, Veronen, & Resick, 1982;
Rothbaum et al., 2000). Important to this discussion, SIT has also been found to be effective with soldiers experiencing combat stress reactions in much greater numbers, suggesting its effectiveness as a public health tool in disasters and situations of mass casualty (
Solomon, 2003). Likewise, a brief version of exposure therapy has been adapted to secondary prevention of PTSD with accident and assault survivors and found to be effective (
Bryant et al., 1998;
Bryant, Harvey, Guthrie, & Moulds, 2003;
Bryant, Sackville, Dang, Moulds, & Guthrie, 1999;
Foa, Hearst-Ikeda & Perry, 1995).
For both those who develop more severe stress reactions and the general population of exposed individuals, “normalization” of stress reactions is a key intervention principle to enhance calming. When individuals interpret their experience in distressing ways (e.g., “I'm going crazy,” “There's something wrong with me,” “I must be weak”), such pathologizing of their own common responses is likely to increase anxiety associated with these reactions. For instance, effective treatment of soldiers with acute stress reactions involves communicating the message that “You are neither sick nor crazy. You are going through a crisis, and you are reacting in a normal way to an abnormal situation” (
Solomon, 2003). Provision of accurate information, survivor education about reactions, and application of cognitive therapy approaches may help calm survivors by helping challenge negative thinking.
Several recent studies examined the role of positive emotions in coping with stress, trauma, and adverse life circumstances and have implications for intervention. More specifically,
Fredrickson (2001) and
Fredrickson, Tugade, Waugh, & Larkin (2003) suggest that positive emotions which include joy, humor, interest, contentment, and love have a functional capacity to broaden a “thought-action” repertoire and lead to effective coping. For this reason, it may help to encourage people to increase activities that foster positive emotions (
Biglan & Craker, 1982;
Zeiss, Lewinsohn, & Munoz, 1979), as well as reduce or eliminate watching, listening to, and reading information that produces negative emotional states (i.e., news). This may be difficult for people because they feel a need to be vigilant and remain updated. For those with minor to mid-level problems of anxiety, limiting media exposure to once in the morning, afternoon, and early evening (but not near bedtime) may be sufficient. Those with more severe emotionality may agree to getting news reports from a friend or family member that give the facts without the images and hyperbole used in much media reporting.
Another important intervention for calming that can be broadly applied is to provide training and structure for problem-focused coping. At the same time, these techniques will build a sense of efficacy and support hope.
Hobfoll and colleagues (1991) underscored that following mass trauma people are likely to interpret the challenges of disaster and mass violence circumstances as one enormous unsolvable problem. Here, it is critical to assist and guide individuals to break down the problem into small, manageable units. This will increase sense of control, provide opportunities for small wins, and, practically speaking, decrease the real problems people are facing (
Baum, Cohen & Hall, 1993). Problem-solving appraisal is consistently associated with reports of approaching and attempting to resolve problems as well as the awareness, utilization, and satisfaction with helping resources. It is also associated with a positive self-concept, less depression and anxiety, and vocational adjustment.
Because problem-solving appraisal can be learned and such training is effective (
D'Zurilla & Goldfried, 1971), it is a potentially fruitful area for intervention development (
Silver et al., 2002). Once new skills are learned, encouraging individuals to apply skills can increase and sustain the efforts needed for recovery. By intervening and providing a structured approach to building efficacy, individuals can come to focus their attention on the task and may even increase their effort in the face of a challenge (
Bandura, 1986). Later in this paper, we address the issue of self-efficacy directly, but it is important to note that the calming effect of increased sense of control and predictability is an important aspect of such interventions.
It should be noted further that some frequent ways of calming might be counter-productive and eventually increase distress and decrease the sense of mastery and control. Hence, benzodiazepines have shown to increase the likelihood of PTSD among symptomatic trauma survivors (
Gelpin et al., 1996), despite an immediate calming effect. Because of their calming effects, benzodiazepines continue to be widely used clinically in the treatment of anxiety disorders, and attention must be given to maintaining calmness in populations for whom such medications are part of their pre-mass-casualty treatment. This is especially relevant because those with pre-mass-casualty anxiety disorders are at particular risk for further negative psychological impact if exposed to mass-casualty trauma. Having similarly soothing activity, alcohol can be used to “self-medicate” and lead to potential misuse and other alcohol-related behaviors. Finally, the use of lies, or “spinning” information in order to calm a population or a group of rescued individuals, ultimately undermines credibility and is counter-productive.
Many of the interventions discussed in this section are of a more individual intervention nature. However, many can be translated to group and community-based interventions. For example, psychoeducation has been at the heart of a number of post-disaster interventions that have been shown to be effective in reducing PTSD (
Goenjian et al., 1997,
2005). Large-scale community outreach and psychoeducation about post-disaster reactions should be included among public health interventions to promote calming. Psychoeducation serves to normalize reactions and to help individuals see their reactions as understandable and expected. Normalizing and validating expectable and intense emotional states and promoting survivors' capacities to tolerate and regulate them are important intervention goals at all levels. Disaster survivors should avoid pathologizing their inability to remain calm and free of the expectable intense emotions that are the natural consequences of such threatening and tragic events. These goals can be accomplished to a great extent through media and community (e.g., church, schools, and businesses) processes.
Along with psychoeducation about reactions, anxiety management techniques can be taught that are directly linked with specific post-disaster reactions (i.e., sleep problems, reactivity to reminders, startle reactions, incident-specific new fears). For instance, sleep hygiene, guidelines for media exposure, and relaxation training techniques can all be packaged through media presentation. This may be particularly important as people often may fear going out or be advised not to go out in the immediate to mid-term post-disaster or mass-trauma phase and so will be linked to television and radio for news and advice. Interactive websites and computer programs can also be used. It will be critical in this regard to communicate at the same time what the signs of more severe dysfunction are so that people also do not underpathologize their symptoms and know where to turn for professional assessment and treatment.
In any such psychological intervention, it should not be underestimated that people's agitation and anxiety are due to real concerns, and actions that help them directly solve these concerns are the best antidote for the vast majority. This follows because real initial resource losses and the secondary losses that occur downstream of the original event are the best predictors of psychological distress (
Freedy, Shaw, Jarrell, & Masters, 1992;
Galea et al., 2002;
Hobfoll, Canetti-Nisim, & Johnson, 2006;
Ironson et al., 1997). Hence, psychological intervention should not be seen as a substitute for interventions that directly relieve threat or that furnish the material resources needed for recovery and restoration of losses incurred.
PROMOTION OF SENSE OF SELF-EFFICACY AND COLLECTIVE EFFICACY
The importance of having a sense of control over positive outcomes is one of the most well-investigated constructs in psychology (
Skinner, 1996). Self-efficacy is the sense that individual's belief that his actions are likely to lead to generally positive outcomes (
Bandura, 1997), principally through self-regulation of thought, emotions, and behavior (
Carver & Scheier, 1998). This can be extended to collective efficacy, which is the sense that one belongs to a group that is likely to experience positive outcomes (
Antonovsky, 1979;
Benight, 2004).
In their trauma models,
Foa and Meadows (1997) and
Resick and Schnicke (1992) underscore that following trauma exposure people are at risk for losing their sense of competency to handle events they must face. This begins with events related to the original trauma, but quickly generalizes to a more fundamental sense of “can't do.” It is a central goal of all successful treatments to reverse this negative view regarding the ability of the self, the family, and the social group to overcome adversity. The best evidence suggests that it is not so much general self-efficacy, but the specific sense that one can cope with trauma-related events that has been found to be beneficial (
Benight & Harper, 2002). For example, in a national Israeli sample, despite feeling in constant danger, 75% of participants stated that they would function efficaciously following a terror attack (
Bleich et al., 2003). Trau-ma-related self-efficacy pertains to the perceived ability to regulate troubling emotions and to solve problems that follow in the domains of relationships, restoration of property, relocating, job retraining, and other trauma-related tasks (
Benight et al., 2000;
Benight, Swift, Sanger, Smith, & Zeppelin, 1999). In line with this thinking, interventions spanning from prevention of burnout (
Freedy & Hobfoll, 1994) to work with victims of trauma (
Resick et al., 2002) are founded in part on the proposition that people must feel that they have the skills to overcome threat and solve their problems.
Several interventions lend themselves to post-disaster and mass violence environments and can be applied to the individual, group, organization, and community levels. Individual and group-ad-ministered CBT have been designed to promote the individual as expert, focusing on imparting skills to the individual, rather than invoking an expert therapist who retains all the relevant expert knowledge (
Follette & Ruzek, 2006). CBT encourages active coping and good judgment about when and how to cope, elements that are critical in raising or regaining self-efficacy. In their work with Turkish earthquake survivors,
Basoglu and colleagues (2005) developed an efficacious single session CBT treatment that aimed at enhancing sense of control over traumatic stressors. A number of programs have made the difficult transition of translating CBT to low and middle-income countries and have found success when they have carefully translated intervention within the socio-cultural ecologies of the target countries (
Hinton, Hsia, Um, & Otto, 2003;
Hinton, Um, & Ba, 2001a,
2001b;
Otto et al. 2003;
Saltzman, Layne, Steinberg, Arslanagic, & Pynoos, 2003). If we keep in mind that most victims were living normal lives prior to the disaster or mass trauma, we can see that the task may be more one of reminding them of their efficacy than of building efficacy where there was none.
When working with children and adolescents, there is a developmental course in the schematization of self-efficacy, efficacy of others (e.g., protective figures), and efficacy of social agencies in response to danger. Addressing such developmental interruptions and promoting normal and adaptive progression is an important component of post-disaster and mass casualty childhood interventions (
Saltzman, Layne, Steinberg & Pynoos, 2006). Teaching children emotional regulation skills when faced by trauma reminders and enhancing problem-solving skills in regard to post-disaster adversities are especially important components of post-disaster interventions that have been shown to be effective (
Goenjian et al., 1997,
2005).
Self-efficacy cannot occur in a vacuum; it requires successful partners with whom to collaborate, join, and solve the often large-scale problems that are beyond the reach of any individual (e.g., when larger systems fail or create bureaucratic obstacles to recovery). Tied to perceived self-efficacy is the construct of collective efficacy (
Benight, 2004;
Sampson, Raudenbush, & Earls, 1997). People in mass casualty situations are aware that they will often sink or swim together. This fact has underscored work by the World Health Organization (WHO) in dealing with refugees fleeing traumatic circumstances, where a key principle of service delivery is the promotion of self-sufficiency and self-government (
de Jong & Clarke, 1996). In this regard, activities that are conceptualized and implemented by the community itself may contribute to a sense of community efficacy. These may include religious activities, meetings, rallies, collaboration with local healers, or the use of collective healing and mourning rituals (
de Jong, 2002b, p. 73). Hence, one of the major mental health interventions following the tsunami in Asia were community efforts to support rebuilding fishing boats that allowed fishermen to resume their daily activities. Similarly, for children and adolescents, restoration of the school community is recognized byWHO and the United Nations Children's Fund (UNICEF) as an essential step in reestablishing a sense of self-efficacy through renewed learning opportunities, engagement in age-appropriate, adult-guided memorial rituals, and school-initiated pro-social activity, where children can see grief appropriately modeled and fully participate in planning and implementation of activities (
Saltzman et al., 2006).
A competent community provides safety, makes material resources available for rebuilding and restoring order, and shares hope for the future (
Iscoe, 1974;
McKnight, 1997). Collective efficacy may be most poignant on the family level, where psychological, material, or social losses are most likely to be felt deeply by loved ones. Families are also often the main source of social capital within any community, and the main provider of mental health care after disasters, especially among rural populations (
de Jong, 2002b).
Murthy (1998) argues that the family must often substitute for professional care and so should be considered a primary axis for intervention. Thus, competent communities promote perceptions of self-efficacy among their members, foster the perception that others are available to provide support, and support families who, in turn, provide sustenance to their members. Holding the perception that others can be called upon for support mitigates the perception of vulnerability and emboldens individuals to engage in adaptive activities they might otherwise see as risky (
Layne et al., in press).
Two aspects of self-efficacy and collective efficacy are critical, but are often omitted from intervention and planning. The first of these is that self- and collective efficacy require behavioral repertoires and skills that are the basis of the efficacy beliefs (
Bandura, 1997).
Saltzman and colleagues (2006) found that people must feel they have the skills to overcome threat and solve their problems. Indeed, self-efficacy beliefs that are not reinforced by ongoing successful action are likely to be quickly compromised (
Bandura, 1997;
Ozer & Bandura, 1990). For instance, soldiers, emergency service workers, and first responders must learn self- and collective efficacy as well as belief in their leaders, themselves, and their group as a unit (
Chen & Bliese, 2002;
Ginzburg, Solomon, Dekel, & Neria, 2003;
Keinan, Friedland, & Sarig-Naor, 1990;
Solomon, 2003;
Solomon, Margalit, Waysman, & Bleich, 1991). Not surprisingly, research indicates that this is best developed by practice involving increasingly difficult situations in which increments of success build to a reality-based appraisal of efficacy (
Keinan et al., 1990;
Meichenbaum, 1974).
The second aspect of self- and collective efficacy, one that is often ignored, is that empowerment without resources is counter-productive and demoralizing (
Rappaport, 1981). Research on disasters and trauma has repeatedly found that those who lose the most personal, social, and economic resources are the most devastated by mass trauma (
Galea et al., 2002;
Ironson et al., 1997;
Neria et al., 2006). However, research also suggests that those who are able to sustain their resources have the best ability to recover (
Benight, 2004;
Galea et al., 2003;
Norris & Kaniasty, 1996). As outlined in Conservation of Resources (COR) theory (
Hobfoll, 1988,
1998,
2001), self- and collective efficacy are themselves personal resources that are likely to be diminished by mass trauma (
Benight et al. 1999;
Benight, Swift, Sanger, Smith, & Zeppelin, 1999), and they are made effective by their being central management resources that “manage” or orchestrate other personal and environmental resources that people possess (
Hobfoll, 2002).
Lack of understanding of the link between efficacy beliefs, behavioral skills, and practiced repertoires as well as access to resources leads to serious attribution and intervention errors. Hence, people will wrongly assume that they, and not circumstances, are the failure, and intervention will over- or under-estimate people's capabilities. People not only need the belief that they can effectively evacuate, gain access to temporary housing, and find a job on their return, they require linkage to resources to act on these beliefs and the skills required to meet their goals. Thus, it is not surprising that attempts to send trauma victims home with self-help pamphlets is likely to backfire (
Turpin, Downs, & Mason, 2005), as it assumes that they possess the skills and resources necessary to enact what is suggested to them in the form of “self-help.” These outcomes will, therefore, be greatly influenced by population vulnerability factors, such as poverty, ethnic minority status, and already depleted resource reservoirs (e.g., due to prior exposure and psychiatric history) (
Hobfoll, 1998). These related beliefs, skills, and resources, in fact, mutually influence one another. Because mass trauma is, typically, an unpracticed experience for all but trained personnel, and because of the unequal distribution of resources in society, there will almost always be holes in the fabric of this belief-behavior-resource linkage that intervention must attend to, whether on the individual, family, or group level.
Finally, it must be underscored that because disasters and situations of mass violence may undermine already fragile economies, efforts to return things to “normal” may be doomed to failure. Because of this,
de Jong (2002b) suggests that public mental health programs need to collaborate with development initiatives (i.e., processes of change leading to better living conditions and more secure livelihood) to help local populations enhance their survival capacities and increase their resiliency and quality of life. For example, following an earthquake in Iran, interventionists worked with communities, providing resources and guidance to help restore sanitation services that lead to empowerment and restored dignity among citizens (
Pinera, Reed, & Njiru, 2005). Benight and colleagues (
Benight, 2004;
Benight et al., 2000) have noted that the more that victims of mass trauma are truly empowered, the more quickly they will move to survivor status. This may be especially true of children. While parents and society quite naturally try to protect children, even for children the rule should be to encourage as much self- and collective efficacy as possible and for intervention to be cognizant of the dangers of over-protectiveness. Adolescents, in particular, can play a key role in community recovery. Admittedly, although the evidence supporting promotion of community development and empowerment is mainly qualitative (
de Jong, 1995;
Paardekooper, 2001), the principle underpinning this approach has strong empirical support, and its translation to intervention deserves fuller investigation.
PROMOTION OF CONNECTEDNESS
There is a tremendous body of research on the central importance of social support and sustained attachments to loved ones and social groups in combating stress and trauma (
Norris, Friedman, & Watson, 2002;
Vaux, 1988). Social connectedness increases opportunities for knowledge essential to disaster response (e.g., “Where is the nearest grocery store?” “Is safe water available?”). It also provides opportunities for a range of social support activities, including practical problem solving, emotional understanding and acceptance, sharing of traumatic experiences, normalization of reactions and experiences, and mutual instruction about coping. This, in turn, can lead to sense of community efficacy that we discuss elsewhere in this paper (
Benight, 2004). Nevertheless, there is actually little empirical research on how to translate this to intervention. Hence, although this is perhaps the most empirically validated of the five principles, interventionists and policymakers will have to be creative in translating this evidence to intervention.
Solomon, Mikulincer, and Hobfoll (1986) noted that prior to development of severe emotional distress, combatants experience loneliness and become emotionally distant from those around them, indicating that the lack of social connections is a risk factor in the very onset of PTSD. Following the attack of September 11th in New York and following terrorist attacks in Israel, one of the most common coping responses was to identify and link with loved ones (
Bleich et al., 2003;
Stein et al., 2004). Delay in making connections to loved ones was a major risk factor following the London bombings of 2005 (
Rubin, Brewin, Greenberg, Simpson, & Wessely, 2005). Research on disasters and terrorist attacks in the United States (
Galea et al., 2002;
Weissman et al., 2005), Israel (
Bleich et al., 2003;
Hobfoll et al., 2006), Mexico (
Norris, Baker, Murphy, & Kaniasty, 2005), Palestine (
Punamäki, Komproe, Quota, El Masri, & de Jong, 2005), Turkey (
Altindag, Ozen, & Sir, 2005), and Bosnia (
Layne et al., in press) indicates that social support is related to better emotional well-being and recovery following mass trauma. This key salutogenic role played by social support is sustained through the post-trauma period extending for months (
Galea et al., 2003) and years (
Green et al., 1990;
Solomon et al., 2005). Other evidence from the field on this issue comes from several mental health professionals with a high level of on-site mass trauma experience. They emphasize that fostering connections as quickly as possible following mass trauma and assisting people in maintaining that contact is critical to recovery (
Litz & Gray, 2002;
Shalev, Tuval-Mashiach, & Hadar, 2004;
Ursano, Fullerton, & Norwood, 1995).
Connecting with others is clearly of fundamental importance to children and adolescents as well, and facilitating their reconnection with parents and parental figures is a primary goal in disaster-related interventions (
Hagan, 2005). For instance, reunion with at least one family member following immigration to the United States after the Pol Pot genocide in Cambodia was linked with lower levels of chronic posttraumatic stress, depression, and substance abuse in surviving adolescents compared to those not reunited with family members (
Kinzie, Sack, Angell, Manson, & Rath, 1986). Of particular note, Cambodian youths living with war-exposed family members fared better than their counterparts living with non-war-exposed foster families. In light of such findings, some trauma-focused interventions directly seek to increase the quantity, quality, and frequency of supportive transactions between trauma survivors and their social fields (
Gottlieb, 1996). A group intervention implemented with war-exposed Bosnian adolescents directly targeted social support via psychoeducation and skills-building. Interventions included (a) enhancing knowledge of specific types of social support (e.g., emotional closeness, social connection, feeling needed, reassurance of self-worth, reliable alliance, advice, physical assistance, and material support); (b) identifying potential sources of such support; and (c) learning how to appropriately recruit support (
Layne et al., 2001). Notably, consumers identified this support-seeking skill as one of the most valuable program elements (
Cox, Davies, Burlingame, Campbell, & Layne, 2005).
The complexity of the social support process is highlighted in the social support, deterioration, deterrence model (
Kaniasty & Norris, 1993;
Norris & Kaniasty, 1996). Developed through careful research on several disasters in the United States, Poland, and Mexico,
Kaniasty and Norris (1993) note that at the same time that social support facilitates well-being and limits psychological distress following mass trauma, parallel social support loss cycles occur. Hence, although initial periods are characterized by a high degree of support, support systems quickly deteriorate under the pressure of overuse and the need of individuals to get on with their own lives (
Raphael, 1986). This makes those who begin with marginal levels of social support especially vulnerable.
Moreover, it is important to remember that potential supporters may actually act in an undermining, rather than a supportive fashion, and this can be especially destructive (
Andrews, Brewin, & Rose, 2003;
Hobfoll & London, 1986;
Pennebaker & Harber, 1993). Negative social support (e.g., minimizing problems or needs, unrealistic expectations regarding recovery, invalidating messages) is a strong correlate to long-term post-trauma distress.
Relating these findings to intervention policy, it is paramount that interventions identify those who lack strong social support, who are likely to be more socially isolated, or whose support system might provide undermining messages (e.g., blaming, minimalization). Keeping them connected, training people how to access support, and providing formalized support where informal social support fails will be important. It will be more difficult to reconnect people to social support in cases of evacuation and destruction of homes and neighborhoods. This means that intervention in these cases should be a priority, as natural support networks will have disintegrated (
de Jong, 2002b;
Sattler et al., 2002).
Large-scale interventions in the majority of countries consistently find that efforts to promote social support networks in temporary refugee camps are effective (
de Jong, 2002b). Work by
de Jong (2002b) suggests the concept of treating temporary sites as villages rather than camps. Villages have village councils, welcoming committees, places of worship, places to go for services, meeting places, entertainment, a soccer field, and places for teens to congregate under supervision. Further, citizens of the village, rather than outsiders, fill the social roles and do so within their natural cultural traditions and practices. If people spending most of their time alone in their own tents, they are not as likely to be as connected to others as if they have things to occupy their time, social responsibilities, and people to share their experiences. This relates again to the issues of self-and collective efficacy noted earlier. It also acts to preserve social structures that help keep communities intact and preserve rules, order, and social supervision (i.e., the rule of law) (
Erikson, 1976).
There are also unhealthy sides of the support process that intervention policy must heed.
Giel (1990) noted that following mass trauma, previous in group-out group divisions, even those that may have been socially resolved, may again become salient as people use power to gain access to much needed resources. Racial, religious, ethnic, social, and tribal divisions can become active in the process of vying for favored application of resources to those in each group. Work on terror management theory (
Landau, Solomon, Greenberg, Cohen & Pyszczynski, 2004;
Pyszczynski, Solomon, & Greenberg, 2003) finds that as mortality salience increases, people become more distrustful of “others,” more jingoistic, and less tolerant. This means that just when added social support is needed, social undermining may transpire instead. Supporting this theory,
Hobfoll and colleagues (2006) noted that during a period of high levels of terrorism both Jews and Arabs became more xenophobic as PTSD increased. Unfortunately, politicians may actually attempt to capitalize on such divisions to increase support from “their” group, as has also been shown in Sri Lanka (
Somasundaram & Jamunantha, 2002).
Despite the research gap between the natural positive influence of social support and the influence of intervention-created social support, there is enough experiential evidence post September 11th in New York (
Simeon, Greenberg, Nelson, Schmeidler, & Hollander, 2005) and from WHO experience with refugees (
van Ommeren, Saxena, & Saraceno, 2005) to make this a “best practices” suggestion, with a clear call for more careful research on the issue. As
Wandersman and Nation (1998) noted for communities with more slow-brewing trauma (e.g., an areas found to be industrial waste sites or having a high rate of crime), supporting social connections is critical to individual, family, and community well-being (see also,
Landau & Saul, 2004).
INSTILLING HOPE
There is strong evidence for the central importance of retaining hope following mass trauma. Hence, those who remain optimistic (
Carver & Scheier, 1998) are likely to have more favorable outcomes after experiencing mass trauma because they can retain a reasonable degree of hope for their future. Instilling hope is critical because mass trauma is often accompanied by a “shattered worldview” (
Janoff-Bulman, 1992), the vision of a shortened future (
American Psychiatric Association, 1994), and catastrophizing, all of which undermine hope and lead to reactions of despair, futility, and hopeless resignation-that feeling that “all is lost.” Because mass trauma is usually an experience people are not trained for or experienced with, it outstrips their learned coping repertoires. Without knowledge about how to cope, it is natural that hope is one of the first victims.
Hope has recently and most commonly been defined in psychology as “positive, action-oriented expectation that a positive future goal or outcome is possible” (
Haase, Britt, Coward, & Leidy, 1992) and, similarly, a thinking process that taps a sense of agency, or will, and the awareness of the steps necessary to achieve one's goals (
Snyder et al., 1991).
Hobfoll, Briggs-Phillips, and Stines (2003) challenged these perspectives, however, as overly based on “rugged individualism” and ignoring the reality that people who experience mass trauma, lifetime poverty, and racism often face. Such an action-oriented view of hope is decidedly Western, even upper-middle class and white. Hope for most people in the world has a religious connotation and is not action-oriented (
Antonovsky, 1979). That is, although hope is internally experienced, it is naturally an outgrowth of the real circumstances in which people find themselves. Nevertheless, what is amazing about the human spirit is that many people, who have been down so long that everything else looks like up, often do retain a sense of optimism, self-efficacy, and belief in both strong others and a God who will intervene on their behalf (
Antonovsky, 1979;
Lomranz, 1990;
Shmotkin, Blumstein, & Modan, 2003).
Perhaps the best theoretical work on hope in the face of mass trauma remains the pioneering work of
Antonovsky (1979) in his examination of Holocaust survivors. The hopeful state that Antonovsky describes is termed “a sense of coherence,” which he defined as “a pervasive, enduring though dynamic feeling of confidence that one's internal and external environments are predictable and that there is a high probability that things will work out as well as can reasonably be expected” (p. 123). A major difference between this viewpoint and the efficacy-based views of hope is that Antonovsky's belief is based on past experience and often is the result of the belief that outside sources act benevolently on one's behalf. He did not emphasize self-agency, which he called an expressly upper-middle class, Western view. Antonovsky emphasized that people, including those in the West, often find hope, not through internal agency or self-regulation, but through belief in God (
Smith, Pargament, Brant, & Oliver, 2000), a responsive government (a belief that may be diminishing), and superstition belief (e.g., “I'm always lucky; things usually work out for me”).
The danger of hinging hope on an internal sense of agency alone was made apparent after Hurricane Katrina, where a natural disaster coupled with a technological disaster in responding dealt a dual blow to poor residents of New Orleans in particular. Many did not evacuate, not because they lacked internal agency, but because they had little reason to hope for a positive outcome of evacuating due to a lack of external resources. This means that it is critical to provide services to individuals that help them get their lives back in place, such as housing, employment, relocation, replacement of household goods, and payment of insurance reimbursements. In a study of veterans with combat-related PTSD, employment status was found to be the primary predictor of hope (
Crowson, Frueh, & Snyder, 2001). Likewise, one of the strongest predictors of PTSD for victims of Hurricane Andrew was the inability to secure funds to rebuild their homes (
Ironson et al., 1997). Moves by the state of Mississippi to force insurance companies to pay for damages following state law is a critical mental health intervention. On a smaller scale, mental health professionals can develop advocacy programs to aid victims to work through red tape and the complex processes involved in the tasks that emerge following mass disaster. Lack of such efforts after the Exxon-Valdez oil disaster led to long-term psychological distress and ongoing resource loss cycles (
Arata, Picou, Johnson, & McNally, 2000). Again, by joining with individuals, rather than just doing for them, self-efficacy can be raised in the process, as well as a sense of hope.
Hope can be facilitated by a broad range of interventions, from individual to group to mass media messaging. On an individual level, several studies have shown that those showing early signs of severe distress benefit from CBT that reduces individual's exaggeration of personal responsibility, something that severely impedes hope due to the fear that one will continue to do badly because the problem is an internal, stable trait (
Bryant et al., 1998;
Foa et al., 1995). The Learned Optimism and Positive Psychology Model (
Seligman, Steen, Park, & Peterson, 2005) adopts the goals of identifying, amplifying, and concentrating on building strengths in people at risk. They distilled therapeutic components that can be applied to strength-building and prevention in which they concentrate on enhancing hope and disputing the catastrophic and exaggerated thinking that undermines hope. Trauma-focused treatment with adolescents has similarly shown the efficacy of addressing ongoing trauma-generated expectations, beyond symptom response, with forward looking exercises that promote developmental progression to instill hope and renewed motivation for learning and future planning (
Saltzman et al., 2006). Additionally, the very act of individual intervention by a mental health professional communicates the message that, with treatment, things will get better (i.e., “I'm an expert and I believe that you can succeed”). Interventionists are encouraged to normalize people's responses and to indicate that most people recover spontaneously (
Foa & Rothbaum, 1998;
Resick et al., 2002), as this in itself instills hope against distressing thoughts (e.g., “I'm going crazy,” “I'm inadequate,” “My reaction is a sign that I can't take it.”). Early intervention can also foster hope by using such techniques as guided self-dialogue (
Foa & Rothbaum, 1998;
Meichenbaum, 1974) to underscore and restructure irrational fears, manage extreme avoidance behavior, control self-defeating self-statements, and encourage positive coping behaviors.
Decatastrophizing is another important intervention component that is critical to preserving and restoring hope. Many people catastrophize in order to adaptively prepare for the worst. Early CBT interventions have been found useful in counteracting these cognitive schemas (
Bryant et al., 1998;
Foa et al., 1995). Resick's (
Resick et al., 2002) Cognitive Processing Therapy works to correct erroneous cognitions related to catastrophizing and self-labeling with traits that spell ultimate failure in coping. Paradoxically, envisioning a realistic, yet challenging, even difficult outcome may actually reduce people's distress, compared to envisioning an exaggerated catastrophic outcome. For instance, acknowledging that one's home will take months to rebuild may need to be accepted, but the assertion that “I will never have a home again” is maladaptive. Hence, intervention at all levels should communicate that catastrophizing is natural, but that it should be identified and countered by more fact-based thinking.
Benefit-finding, often associated with increased hope, appears to be a common process among individuals facing a myriad of threatening events, and it has been shown to predict mental health adaptation months and even years later (
Antoni et al., 2001;
King & Miner, 2000;
McMillen, Smith, & Fisher, 1997;
Stanton, Danoff-Burg, Sworowsky, & Collins, 2001). Still undefined is whether this phenomenon is best conceived as a selective evaluation, a coping strategy, a personality characteristic, a reflection of verifiable change or growth, a manifestation of an implicit theory of change, or a temporal comparison. Caution should be taken in designing interventions that promote seeing benefit in trauma, as even well-intentioned efforts to encourage benefit-finding are frequently interpreted as an unwelcome attempt to minimize the unique burdens and challenges that need to be overcome. Moreover, some research has found benefit-finding to be related to greater PTSD, greater xenophobia, and greater support for extreme retaliatory violence (
Hobfoll et al., 2006). It is suggested that interventions focus more on highlighting already exhibited strengths and benefit-finding, rather than promoting benefit-finding prior to individuals' readiness.
On a community level, group or large-scale interventions may be more impactful and efficacious than individual interventions. For instance, group interventions for mass trauma offer the advantage that many of the problems are shared by hundreds or thousands of people, and so coping worksheets that identify common problems gain efficiency that might otherwise take many sessions in individual therapy. On a larger scale,
Adger and colleagues (2005) point out that social-ecological resilience is an important determinant in recovery from disasters, particularly the ability of communities to mobilize assets, networks, and social capital both to prepare for and respond to disasters. This underscores how community processes interface with individual hope. The media, schools and universities, and natural community leaders (e.g., churches, community centers) can enhance hope by helping people focus on more accurate risk assessment, positive goals, building strengths that they have as individuals and communities, and helping them tell their story, following
Seligman and colleagues' (2005) learned optimism and positive psychology model. In this regard, just as CBT directs individuals not to dwell on self-blame and to move into a problem-solving mode, this same set of directives can be recommended broadly, as so many people in such situations share these kinds of feelings and thoughts. The advantage of a community model over the individual, in this regard, is that the group (e.g., mosque, school, business organization, chamber of commerce, Rotary Club) can develop hope-building interventions, such as helping others clean up and rebuild, making home visits, organizing blood drives, and involving members of the community who feel they cannot act individually because of the magnitude of the problem.
SUMMARY AND CONCLUSIONS
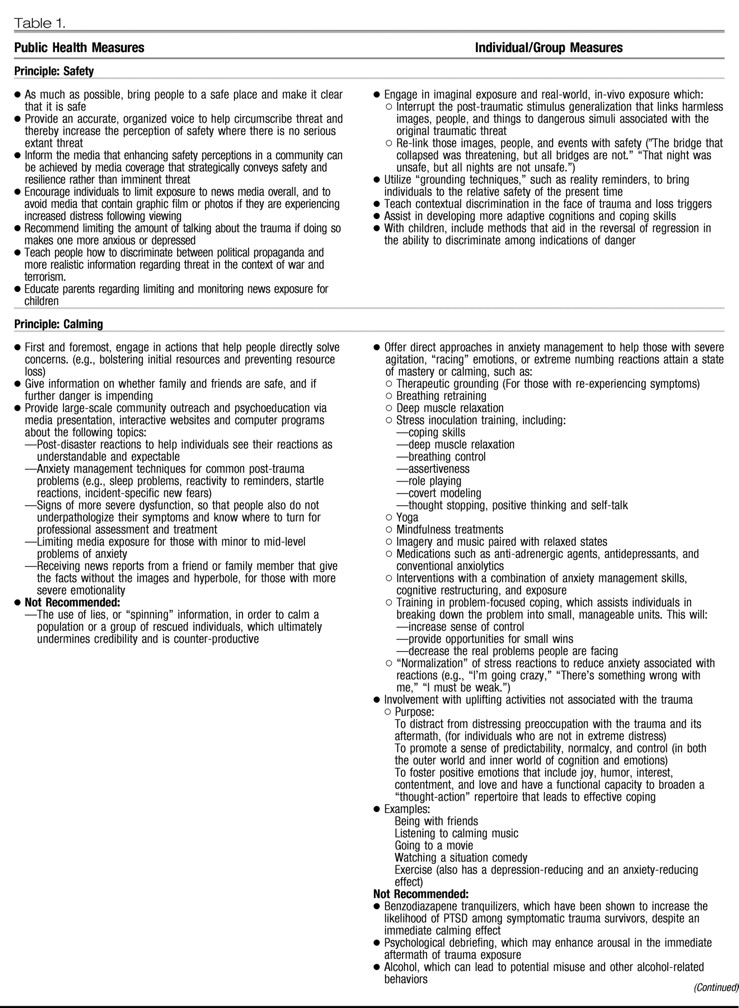
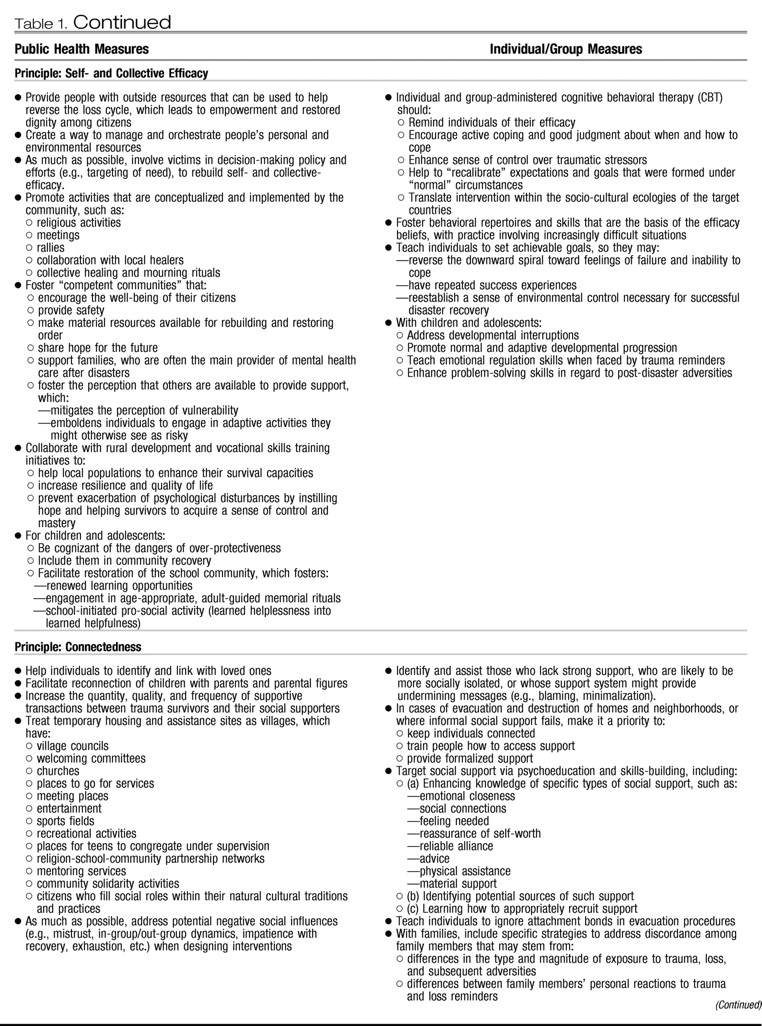
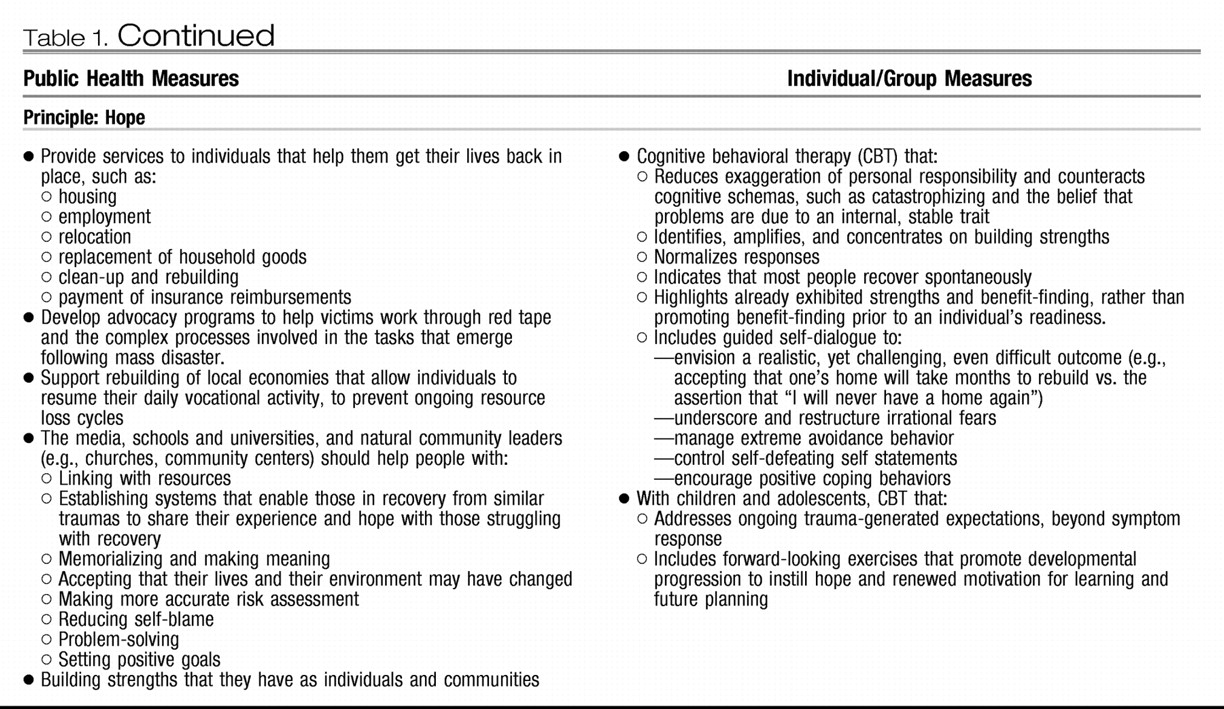
We have outlined five key principles of early to mid-level intervention following disaster and mass violence. These principles are seen as central core elements of intervention and will help in the process of setting policy and designing intervention strategy. They apply to all levels of intervention, from those focusing on the individual to those that are broadly community based. Clearly, we already have effective clinical interventions for survivors who develop PTSD (
Foa et al., 1999;
Resick et al., 2002) and for whom such treatment is accessible and acceptable. What is needed are more broad-scale interventions that inform primary and secondary prevention, psychological first-aid, family and community support, and community support functioning (
de Jong, 2002a;
Eisenbruch, de Jong, & van de Put, 2004) (See
Table 1).
The scale of recent disasters and incidents of mass violence also underscores that these interactions must be available to large numbers of individuals, at levels that quickly outstrip the available individual-level therapists who are local or may be dispatched to a region. Clearly, what we have referred to as intervention includes actions that must go well beyond the bounds of psychotherapy. This means that intervention must be conducted not only by medical and mental health professionals, but also by gatekeepers (e.g., mayors, military commanders, school teachers) and lay members of the community. Stopping the cycle of resource loss is a key element of intervention and must become the focus of both prevention and treatment of victims of disaster and mass trauma, and this includes loss of psychosocial, personal, material, and structural (e.g., jobs, institutions, organizations) resources (
Hobfoll, 1998).
We believe that there are many ways to operationalize these principles, and they should be applied in the design of more carefully detailed interventions that must fit the ecology of the culture, place, and type of trauma. These should be tested to the extent possible in pilot programs, refined, retested, and finally examined with analyses that examine their components. It will be important to examine a full spectrum of potential indicators of psychological distress and impaired functioning in these studies. Depressive disorder, somatoform disorder, and other anxiety disorders show elevated risk ratios after disasters and should be addressed as well as PTSD, in addition to a range of psychosocial problems (
de Jong, Komproe, & van Ommeren, 2003). Moreover, each of these principles reflects an important outcome in its own right. Hence, interventions that enhance and preserve sense of safety, calming, self- and communal efficacy, connectedness, and hope will have achieved important successes in the post-disaster period.
It is also critical that we remain modest in our claims about what interventions can accomplish towards prevention of long-term functional and symptomatic impact. While we believe that the provision of interventions based on these principles will be effective, it is unknown to what extent such interventions will be associated with significant improvements in functioning. As occurred in the case of the stress debriefing literature (e.g.,
Raphael & Wilson, 2000), overstatement of the proposed effects of an intervention prior to evidence of its impact may lead to implementation of programs of limited effectiveness and block the development of more efficacious programming. It is also important that interventions consider the preferences of recipients as a disaster response is planned, as well as the particular ecology of that disaster. These principles will not lead to a one-treatment-fits-all approach.
Post-disaster and mass casualty interventions must also be subjected to economic modeling and cost-benefit analyses. Such interventions, given the numbers of potential recipients who may be involved, will demand considerable revenues and resources. For this reason, there will be a need to design multi-layered interventions, with costly (per case) individual-level interventions for the most seriously impaired and less costly (per case) intervention for larger groups and communities. For instance,
Basoglu and colleagues (2005), in an attempt to develop a brief treatment for disaster survivors, found that a single session of modified behavioral treatment in earthquake-related PTSD produced significant treatment effects on all measures at post-treatment. More generally, media-, telephone-, and internet-based interventions hold promise as cost-effective ways of promoting sense of safety, efficacy, connectedness, calming, and hope and are likely to supplement more traditional forms of response (cf.,
Ruzek, 2006;
Ruzek, Maguen, & Litz, in press).
Clearly, the major weakness of our recommendations is that there are few clinical trials or direct examinations of the principles we have recommended in disaster or mass violence contexts. What we have done is to carefully review the empirical literature from many fields, compare it to the broad experiences we have as experts involved in work on disasters, terrorism, war and other mass casualty situations, and make informed judgments and recommendations. Currently, governments, public health agencies, and aid organizations are without any roadmap for intervention. It is our combined judgment that there will not be a blueprint that will be based on direct evidence (i.e., randomized, controlled trials) in this field in the reasonable future. Indeed, many of us feel that the chaotic and varied nature of disasters and mass casualty situations will prevent our ever having a clear, articulated blueprint based on strong, direct, empirical evidence. Hence, we believe that our empirically informed review and principles are the best strategy for the near and medium range future. Clearly, it is not the only way the literature can be interpreted, but we believe it is a sound effort that can have major public health impact.
Finally, in applying these principles internationally, it will be critical to consider local culture and custom at all stages of design and implementation (
de Jong, 2002a). We believe that there is international, multicultural evidence for each of the general principles, but how they are translated into practice and the degree, for example, of emphasis on individual versus collective process will vary greatly from East to West and from industrialized to non-industrialized world. In each case, applying the principles of ecological congruence will be paramount (
Hobfoll, 1988).