In clinical psychiatry there is a longstanding belief that comorbid personality psychopathology adversely affects the outcome of treatment in major depression. Recent reviews (
Mulder, 2002;
Kool et al, 2005;
Newton-Howes et al, 2006), although contradictory, challenge these beliefs. Mulder's systematic review and the meta-analysis of antidepressant drug randomised controlled trials by Kool
et al report no adverse effect of comorbid personality disorders on the outcome of major depression. However, the meta-analysis of Newton-Howes
et al included all treatments for major depression and reported a small but significant adverse effect of personality disorder. These inconsistent findings may reflect differences in treatment outcome related to different forms of therapy:
Newton-Howes et al (2006) reported a trend for psychotherapies to produce a poorer outcome in patients with a personality disorder compared with treatment with antidepressant drugs.
We have longstanding interests in the prediction of treatment responses in depression (
Joyce et al, 2002,
2003) and have reported that comorbid personality disorder has little impact on outcome in patients treated with antidepressant medication (
Joyce et al, 2003;
Mulder et al, 2003,
2006). In this paper we examine whether personality disorder or traits as assessed by a clinician interview based on DSMIV, or a self-report of temperament and character (
Cloninger et al, 1993), have an impact on treatment response in patients with depression receiving psychotherapy. We also investigate whether the type of psychotherapy—in this study interpersonal psychotherapy and cognitive-behavioural therapy—has any impact.
RESULTS
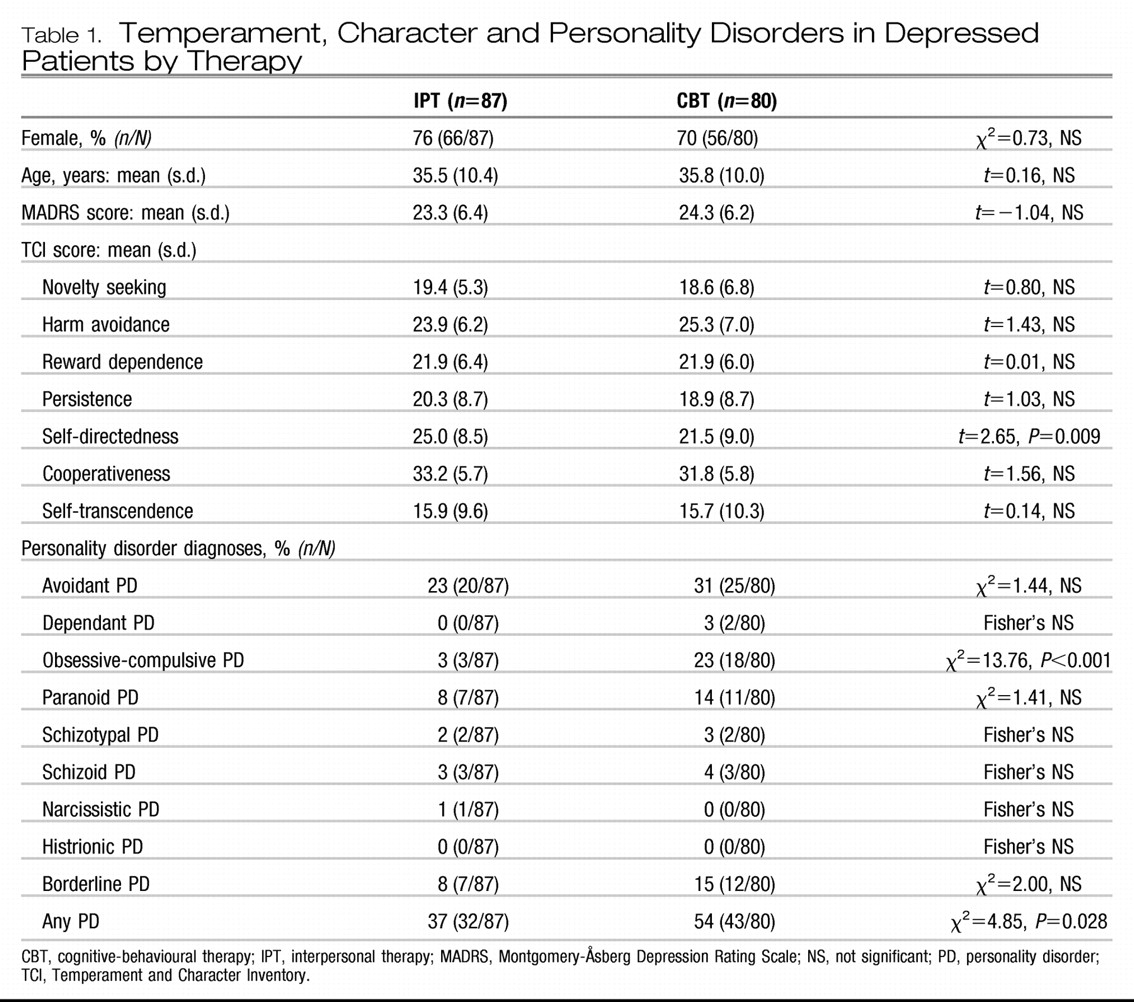
Table 1 shows the gender, age, depression severity, temperament, character and personality disorder status of the 87 participants randomised to interpersonal therapy and the 80 participants randomised to cognitive-behavioural therapy. The latter group scored lower on the self-reported self-directedness item from the TCI, were rated by a clinician as being more likely to have one or more personality disorders and had a higher rate of obsessive compulsive personality disorder.
Clinician-assessed personality disorder and treatment response
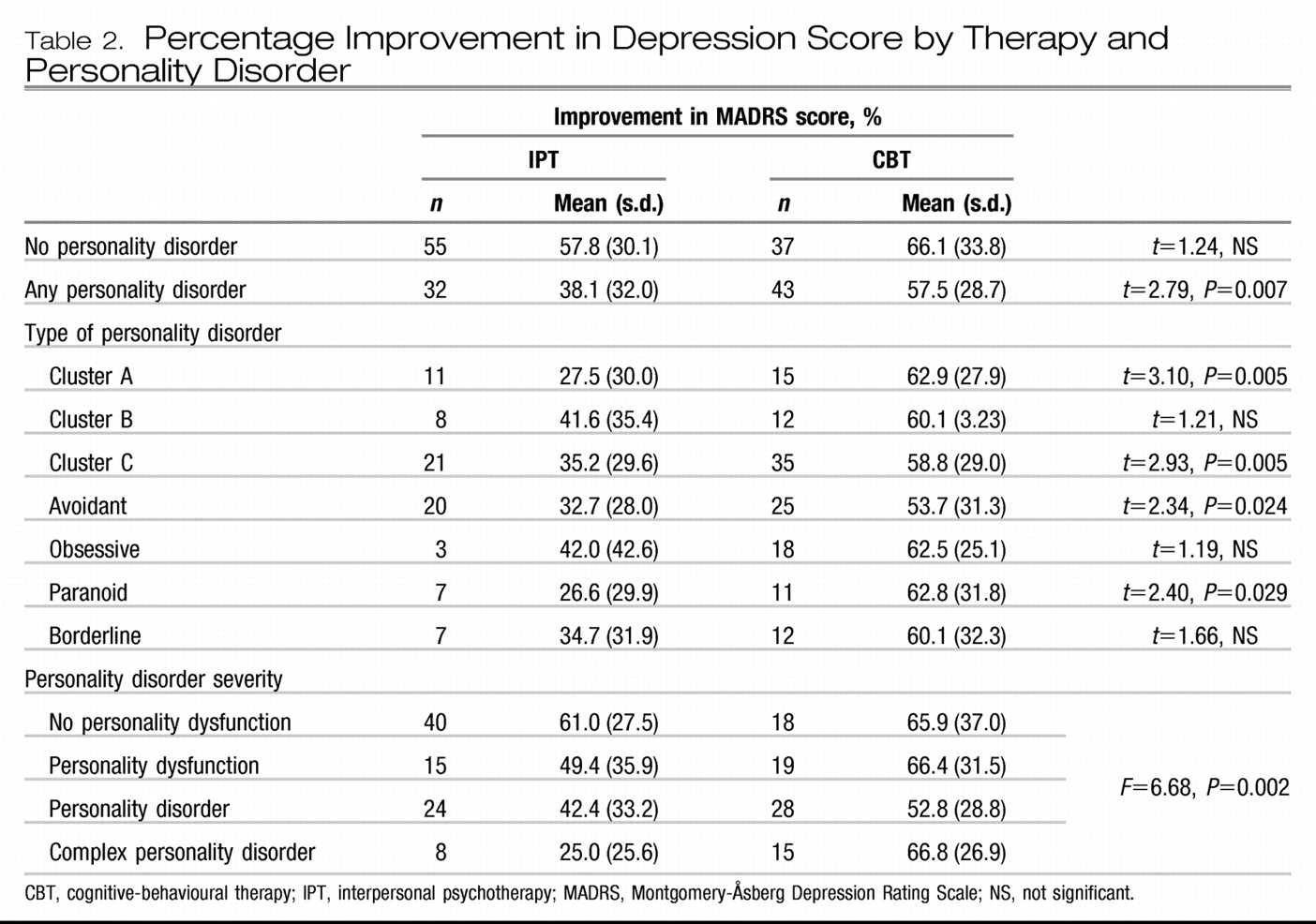
Table 2 shows the effect of clinician assessed personality disorder on treatment outcome by therapy. For participants without a personality disorder the two therapies produced comparable treatment responses. However, for participants with any personality disorder interpersonal psychotherapy had a poorer treatment outcome than cognitive-behavioural therapy. Although numbers are limiting when response is examined by specific personality disorder cluster, or by the four most common individual personality disorders, the results consistently show a pattern of personality disorder adversely affecting treatment outcome with interpersonal psychotherapy but not with cognitive-behavioural therapy. Statistically significantly poorer treatment response with interpersonal psychotherapy is found in those with cluster A and C personality disorders and in avoidant and paranoid personality disorders. Personality disorder severity shows a comparable finding, with more severe personality disorder adversely affecting response to interpersonal psychotherapy but not cognitive-behavioural therapy.
From
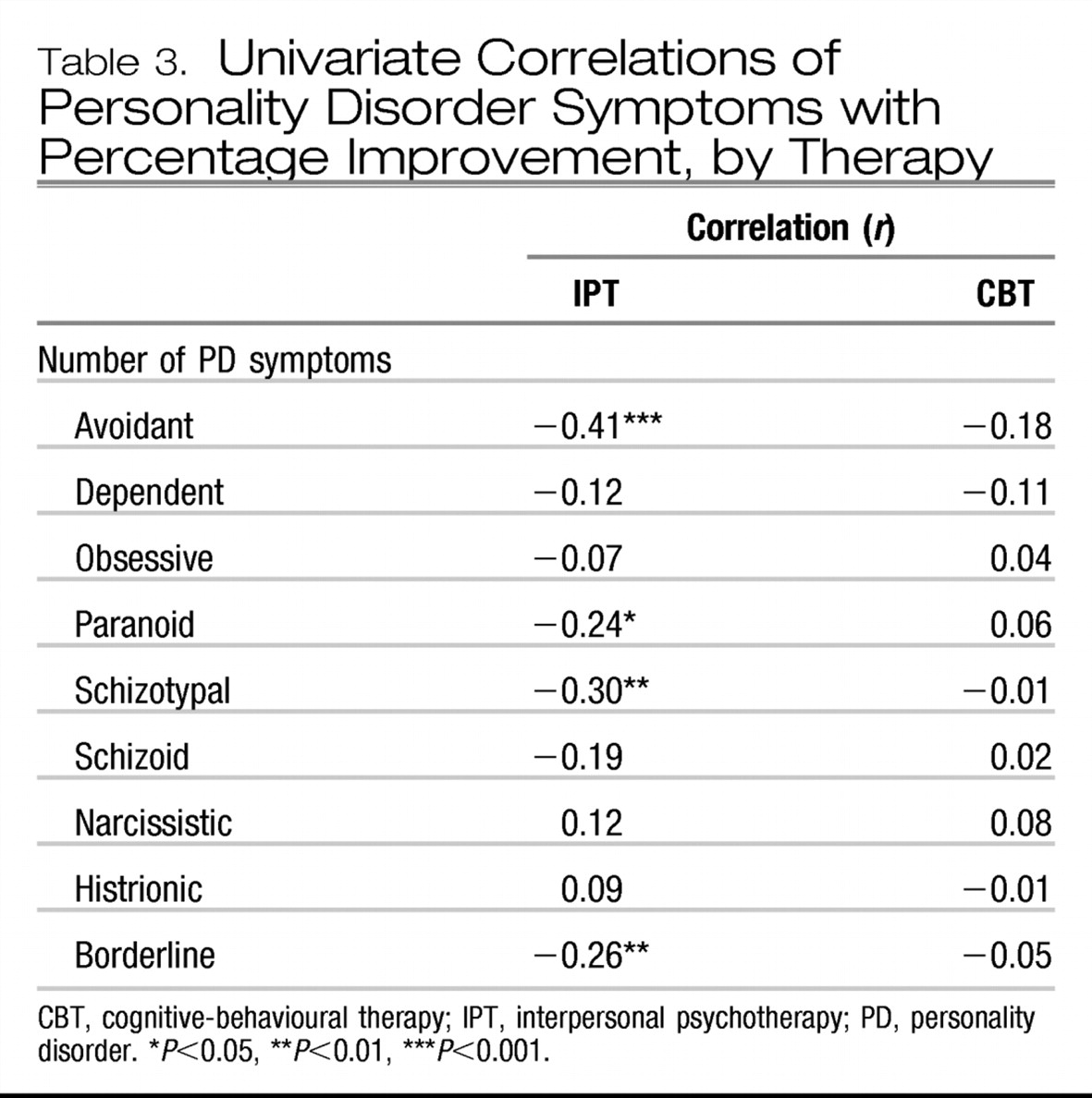
Table 3, which shows the univariate correlations of number of personality disorder symptoms with treatment response, by therapy, it can be seen that response to cognitive-behavioural therapy is unrelated to number of specific personality disorder symptoms. Conversely, a poorer response to interpersonal psychotherapy is seen in participants with more avoidant, paranoid, schizotypal or borderline symptoms.
Self-report temperament and character and treatment response
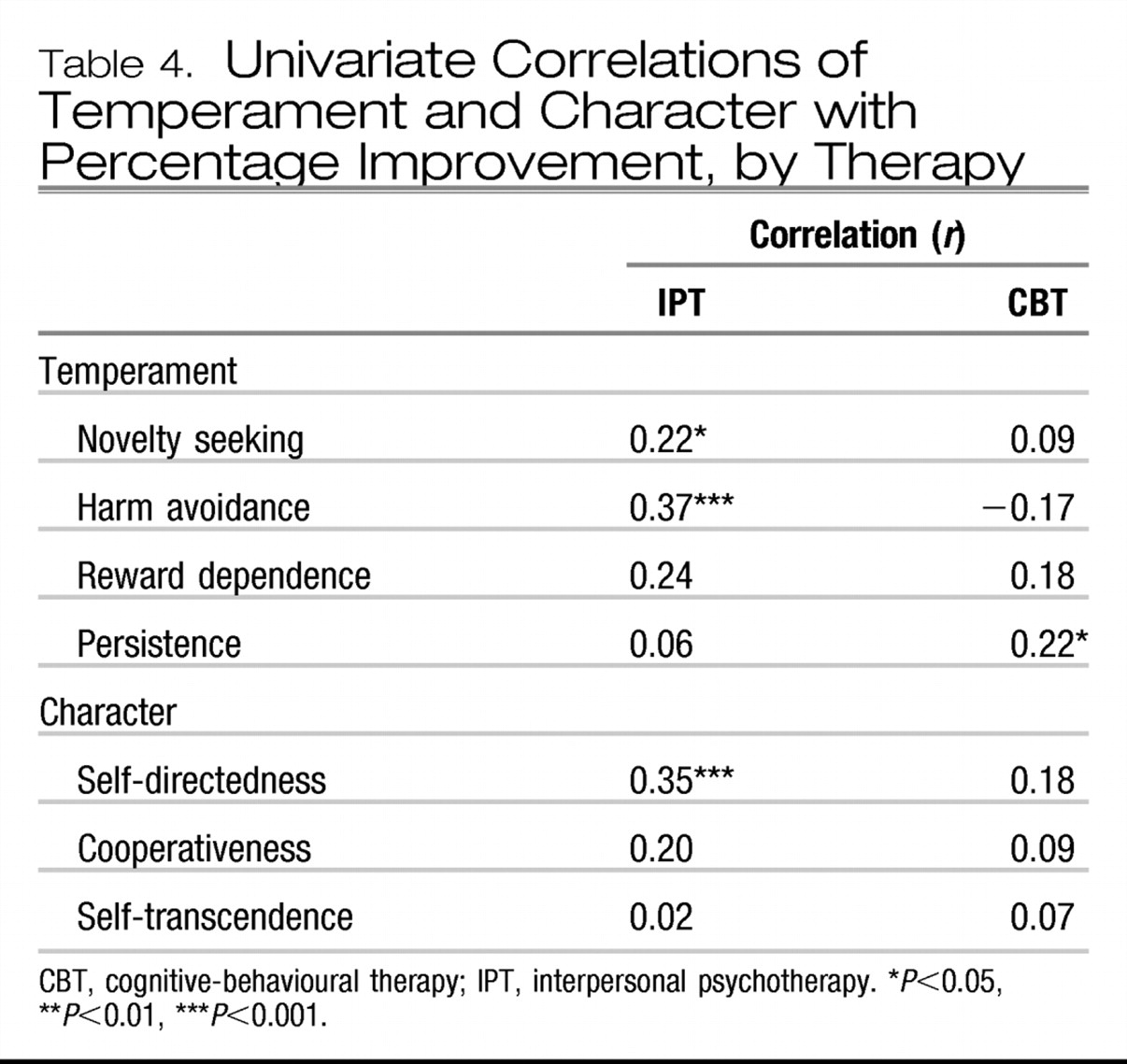
Table 4 shows the univariate correlations of self-report temperament and character with treatment response, by therapy. For cognitive-behavioural therapy only low persistence predicts a worse treatment outcome. For interpersonal psychotherapy high harm avoidance and low self-directedness strongly predict a poor treatment response; low novelty seeking and low reward dependence also significantly predict a poorer treatment response.
Relationships between personality disorder, temperament and character
Low self-directedness and low cooperativeness both correlated with total personality disorder symptoms (r=0.48, P< 0.001). Novelty seeking was positively correlated with cluster B personality disorder symptoms (r=0.25, P<0.01) and with borderline symptoms (r=0.22, P<0.01). Harm avoidance was correlated with cluster C personality disorder symptoms (r=0.47, P<0.001), plus avoidant symptoms (r=0.52, P<0.001), dependent symptoms (r=0.28, P<0.001), paranoid symptoms (r=0.31, P<0.001), schizotypal symptoms (r=0.32, P<0.001) and borderline symptoms (r=0.24, P<0.001). Low reward dependence was most strongly correlated with cluster A personality disorder symptoms (r=0.39, P<0.001) and schizoid symptoms (r=0.38, P<0.001).
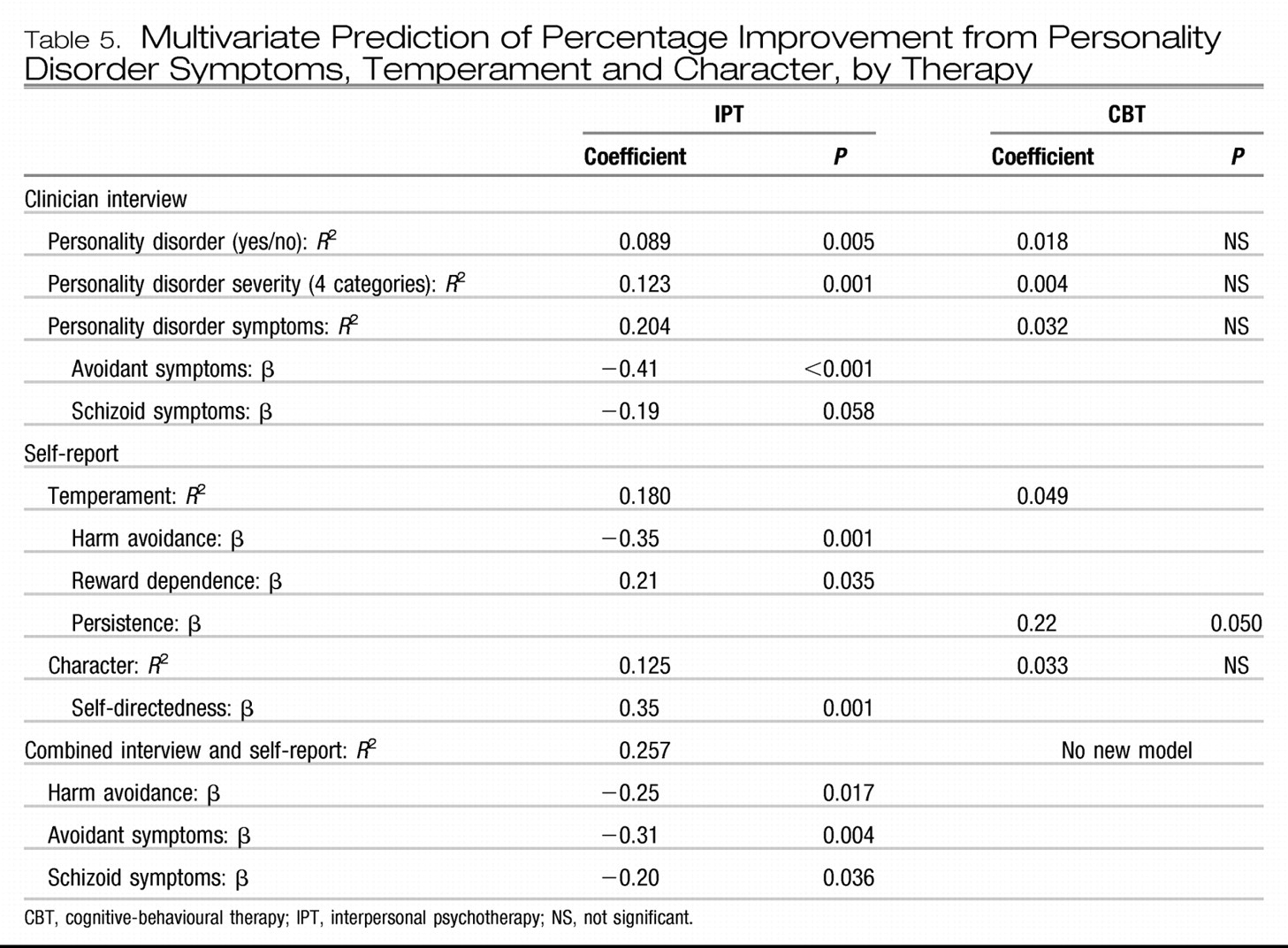
Multivariate prediction of treatment response by therapy
Table 5 shows the results of a series of stepwise multiple regressions predicting mean percentage improvement from personality variables by therapy. The first observation of note from this table is that personality minimally predicts outcome for patients randomised to cognitive-behavioural therapy. The corollary of these findings is that neither personality traits nor disorders have an adverse impact on the outcome of patients with depression treated with this therapy.
However, for interpersonal psychotherapy, personality can have a major impact on treatment response in patients with depression. A simple categorical personality disorder diagnosis (yes/no) explains 8.9% of outcome, with those with a personality disorder having a poorer outcome (see
Table 2). Using Tyrer's four-point measure of personality disorder severity (
Tyrer, 2005) explains 12% of treatment outcome, with a mean improvement of 61% in those with no personality dysfunction declining to a 25% improvement in those with complex personality disorder (i.e. disorders in at least two separate clusters). However, counts of personality disorder symptoms explain 20% of treatment response, with avoidant and schizoid symptoms predicting poor outcome.
The TCI similarly predicts response to interpersonal psychotherapy. Temperament explains 18% of treatment outcome, with high harm avoidance and low reward dependence predicting poor outcome (related respectively to avoidant and schizoid symptoms). Self-directedness explains 12.5% of the treatment outcome. Combining temperament and character scales does not improve on the 18% explained by temperament, as harm avoidance and self-directedness are negatively correlated 0.5.
Finally, the combination of clinician interview and the TCI explains 26% of treatment outcome, with both high harm avoidance and avoidant personality disorder symptoms (despite being correlated 0.52) and schizoid personality disorder symptoms being the significant variables.
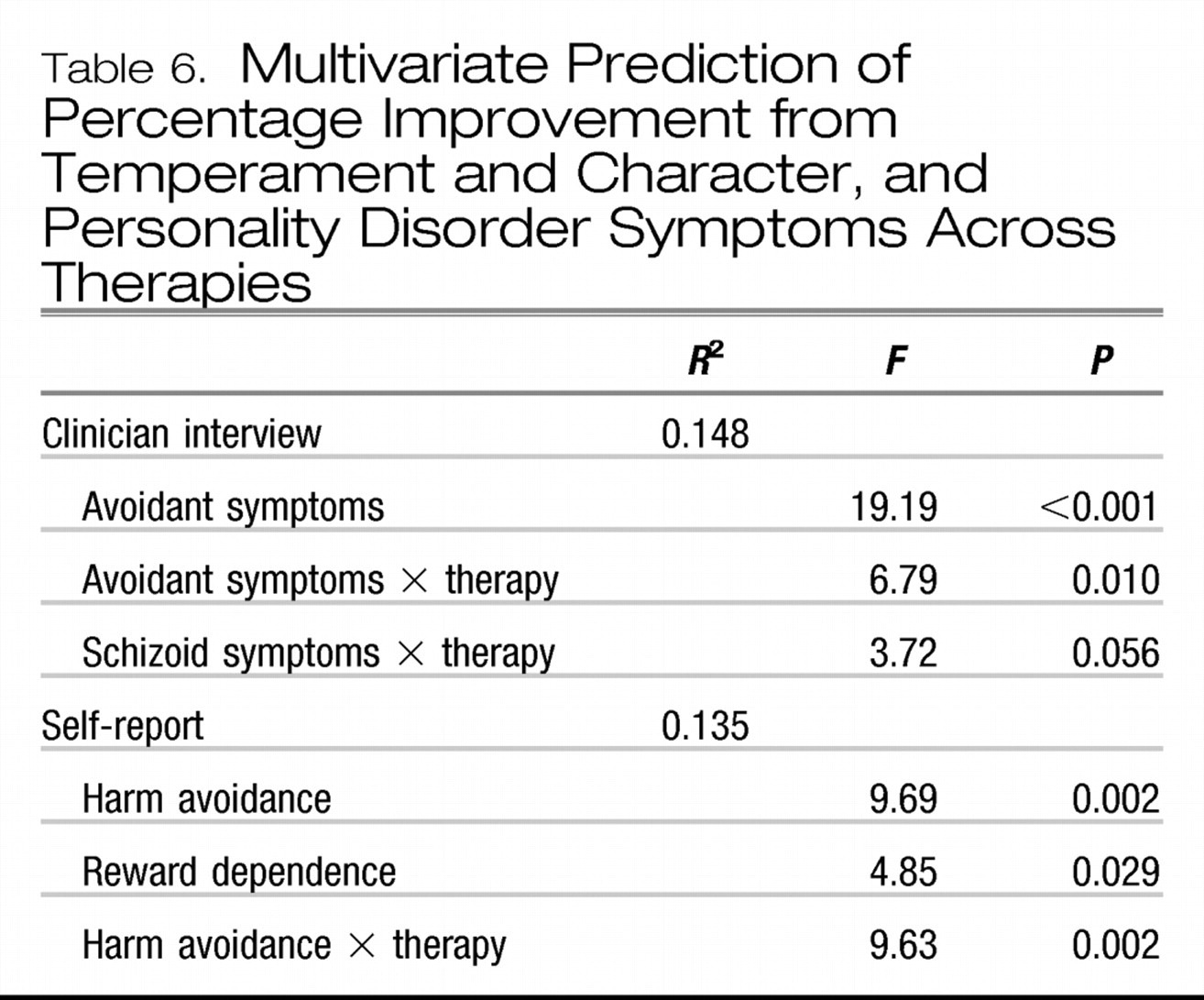
Prediction of treatment response across therapies
Table 6 shows the results of multiple regression across therapies for clinician interview and TCI data separately. From the clinician interview data it can be seen that high levels of avoidant personality disorder symptoms contribute to a poorer treatment outcome, and that for both high avoidant personality disorder symptoms and schizoid symptoms there is an interaction with therapy such that those with high personality disorder symptoms do worse with interpersonal psychotherapy.
The results with the TCI are generally similar, in that high harm avoidance and low reward dependence are associated with a poorer treatment outcome. There is also an interaction of harm avoidance with therapy, such that for those with high harm avoidance interpersonal psychotherapy is associated with a poorer treatment outcome.
Confounding by severity of depression
In the companion paper (
Luty et al, 2007) it was reported that interpersonal psychotherapy was associated with a poorer outcome in severe depression (MADRS score ≥30). We ran analyses again including severity and severity × therapy. The personality predictors and the severity × therapy findings remained in the final multiple regression, and the inclusion of the severity × therapy variable added approximately a further 3% to the variance explained by the personality predictors of outcome.
DISCUSSION
In this randomised clinical trial we found that neither personality disorder nor personality traits adversely affected the outcome when patients with major depression were randomised to cognitive-behavioural therapy. Conversely, the presence of any personality disorder did adversely affect treatment outcome for patients with major depression randomised to interpersonal psychotherapy. Not unexpectedly, a dimensional measure of personality disorder severity was more statistically powerful in explaining a poorer outcome with interpersonal psychotherapy than a categorical personality disorder diagnosis. Thus, whereas the categorical diagnosis explained 9% of treatment outcome, the dimensional model of personality disorder severity explained 12% of treatment outcome. Self-directedness from the TCI, which is a self-report measure of personality disorder severity, explains a comparable 12.5% of the treatment outcome with interpersonal psychotherapy.
When we moved beyond personality disorder or personality disorder severity, and examined combinations of personality disorder symptoms as dimensions, or temperament, then 18–20% of variance in outcome with interpersonal psychotherapy was explained. With the clinician interview the major determinant of outcome was avoidant symptoms and the secondary determinant was schizoid symptoms. With the TCI temperament scales the major determinant of poorer outcome was high harm avoidance and the secondary determinant was low reward dependence. Given that avoidant symptoms correlated with harm avoidance (0.52) and that schizoid symptoms correlated with low reward dependence (0.38), these are highly congruent findings. It is also noteworthy that a combination of clinician interview and self-report personality variables explains over 25% of the treatment outcome with interpersonal psychotherapy, which suggests that neither method of assessing personality fully captures the personality traits that are influencing the outcome of this therapy.
When outcome was assessed across therapies, personality variables interacted with therapy in predicting outcome. The major finding with clinician interview data was the interaction of therapy with avoidant symptoms, whereas the comparable finding with the TCI was the interaction of therapy with harm avoidance. Either way, this suggests that for patients with avoidant symptoms or high harm avoidance cognitive-behavioural therapy may be superior to interpersonal psychotherapy. Indeed, for patients with depression and avoidant personality disorder, cognitive-behavioural therapy was superior. These findings are congruent with the study by
Barber & Muenz (1996), whose analysis of data from the National Institute of Mental Health Collaborative Treatment of Depression Study showed cognitive behavioural therapy to be superior to interpersonal psychotherapy for patients with depression and avoidant personality. Their other finding, that interpersonal psychotherapy was superior to cognitive behavioural therapy in those with obsessive-compulsive personality (
Barber & Muenz, 1996), was not replicated by us; indeed, our results tended in the opposite direction.
Our results need to be considered in the context of the strengths and limitations of this randomised clinical trial. Although this is the largest direct comparison of interpersonal psychotherapy and cognitive-behavioural therapy for depression, for analyses of subgroups of patients with depression and specific personality disorders the numbers were perhaps marginal. However, the use of dimensional measures of personality, which tend to be more statistically powerful, produced significant results. The key outcome in this study was percentage improvement in depressive symptoms after 16 weeks of weekly therapy, and the results reported may not be relevant to the prediction of longer-term outcome.
Our finding that personality disorder does not have an adverse impact on treatment response to cognitive-behavioural therapy in depression is consistent with findings that personality disorder does not adversely affect treatment response to antidepressant drugs in depression (
Mulder, 2002;
Kool et al, 2005). However, it is therefore interesting that personality disorder does adversely affect treatment response to interpersonal psychotherapy. It is also interesting to speculate whether the latter finding extends to other “dynamic” psychotherapies, thus suggesting they should not be treatments of choice for depression in patients with personality disorders. This suggestion would be at odds with the traditional clinical belief that dynamic psychotherapies are indicated for patients with personality disorders.
The finding that high harm avoidance and/or avoidant personality symptoms interfere with the efficacy of interpersonal psychotherapy is consistent with findings that high negative affect or neuroticism is a negative prognostic factor in the treatment of depression. The more original finding that low reward dependence and/or schizoid symptoms decrease treatment response could be interpreted as evidence for interpersonal deficits (
Luty et al, 1998), which have been considered the most difficult of the interpersonal problem areas in which to effect therapeutic gain. An alternative way of interpreting the findings regarding schizoid symptoms is that interpersonal psychotherapy, which formulates depression within an interpersonal context, is not indicated in patients who have a low need for interpersonal contact (schizoid and/or low reward dependence).
Even though the two therapies had comparable treatment efficacy for depression, our findings that personality disorder does not adversely affect the outcome for depression treated with cognitive-behavioural therapy but does adversely affect the outcome of treatment with interpersonal psychotherapy suggests that these two psychotherapies may work for different patients or by different mechanisms.