WHAT IS MOTIVATIONAL INTERVIEWING?
First described by William Miller in 1983 (
1) and further developed in collaboration with Stephen Rollnick over the next three decades (
2–
4), motivational interviewing (MI) represents a general theory of behavior change associated with a set of positive attitudes (“spirit of motivational interviewing”) and pragmatic, operational-defined intervention techniques.
MI is robustly evidence-based and widely disseminated, with broad applications in the fields of addictions, health behaviors, psychotherapies, criminal justice, and other domains. A recent review noted more than 200 current research projects, with more than 100 clinical trials, using or directly investigating the effectiveness of MI (
5). In the United States, 47 states encourage the use of MI as a preferred treatment for substance abuse, and 8 states mandate the use of an empirically based treatment such as MI for addiction and/or mental health. “This widespread dissemination has led to a proliferation of MI adaptations as well as a burgeoning industry in training, continuing education, and certification of MI practitioners” (
5).
There are 11 books on MI, more than 800 publications, and 1,200 trainers in 43 languages (William Miller, personal communication). Four meta-analyses demonstrate effectiveness across multiple areas of patient behavior including substance abuse, smoking, obesity, and medication nonadherence (
6–
9).
New data on life expectancy and general medical health of psychiatric patients confirm the relevance of MI for psychiatrists: the life expectancy of patients with severe mental illness is 32 years less than that of age- and sex-matched control subjects, and the risk of death from cardiovascular disease is two to three times higher than that of control subjects (
10–
17). Despite this evidence and the compelling relevance of MI for general psychiatric practice, many psychiatrists have little appreciation for the principles and practice of MI.
This article defines and describes MI, summarizes the evidence base supporting its use for the treatment of addictions, and discusses how MI can be integrated into the routine practice of psychiatry to improve efficiency and effectiveness for a broad range of other conditions and psychotherapies. For example, in addition to the formal treatment of addictions, MI approaches can be used in routine practice by helping psychiatrists address the much more common problem of risky drinking (discussed in a separate section below) as well as other applications to everyday practice issues, e.g., adherence to medications (
18–
20), lifestyle modifications (diet, exercise, and smoking) (
21–
25), and increasing the efficiency and effectiveness of various psychotherapies (
26,
27).
Although the basic tenets of MI have remained intact over the last 25 years, Miller and Rollnick have revised the core definition several times. In 2002, they defined MI as a “directive, client-centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence” (
2). In the last few years, however, they have revised the concept of “directive counseling,” in favor of a style they name “guiding” which seems to better capture the essence of the approach they advocate. Thus, in 2008, MI was redefined as “a refined form of the familiar process of guiding” (
4). More recently, explaining probable changes to the definition of MI, they described one possible new definition of MI as “a person-centered counseling method for addressing the common problem of ambivalence about behavior change” (unpublished keynote address, Second International Conference on Motivational Interviewing, Stockholm 2010). This possible new definition represents only one possible version that may be revised substantially before publication of Miller and Rollnick's third edition of “Motivational Interviewing,” expected in 2011. Despite these modest changes in concept and definition, MI throughout the years has retained the essence of its innovative approach to behavior change.
With respect to the application of MI in the general medical and psychiatric setting, four general principles for the application of MI can be summarized by the acronym RULE:
resist the righting reflex,
understand the patient,
listen to the patient, and
empower the patient
To
resist the righting reflex, the clinician actively suppresses the reigning medical paradigm to tell patients what to do in an authoritarian manner, in contrast to helping patients express their own internal motivations for behavior change. Practitioners
understand patients through the use of open questions about unhealthy behavior, e.g., asking “what is good and what is not so good” about a specific behavior. The clinician who can
listen to the patient can more easily express accurate empathy and build trust and a working alliance for change. The practitioner helps
empower a patient by building a sense of self-efficacy, through communicating support and confidence in the patient's inherent ability to change.
In addition to the elements of RULE, MI also facilitates change by “rolling with resistance” (that is, not arguing directly with patients) and focusing dialogue on patient “change” talk. This focus on change talk leads to elicitation, clarification, and hopefully to resolution of a patient's inherent ambivalence about persisting unhealthy behaviors and about the desire, ability, reasons, needs, or commitment to change. At the most advanced levels, MI encourages positive change by eliciting “discrepancies” and then overt discussion about any differences that may exist between a patient's current behaviors and broader personal desires and values. Attention to this discrepancy (or inconsistency) functions as a powerful motivator for positive change. As discussed by Robert Cialdini in his authoritative review of the social psychology of persuasion and influence, “Psychologists have long understood the power of the consistency principle to direct human action … prominent theorists such as Leon Festinger, Fritz Hieder and Theodore Newcomb have viewed the desire for consistency as a central motivator of our behavior” (
28,
29).
The underlying approach of MI practice must always communicate a sense of collaboration, evocation, and respect for autonomy, or what is called the “spirit of motivational interviewing.” Collaboration suggests that practitioners and patients should be equal in any discussion about change, evocation means that ideas for changing unhealthy behaviors should come from the patient and not be directed by the clinician, and respect for autonomy indicates that professionals must support and communicate acceptance of the right of patients to change or not to change. Measures of the spirit of MI, by itself, have been shown to predict subsequent adaptive behavior change in patients with persistent unhealthy behaviors (
30).
MI challenges traditional intervention methods by suggesting that many patients already know what is best for them. MI recommends that professionals work collaboratively with their patients to make decisions about specific strategies for change, while acknowledging freedom of choice for patients. A menu of choices is one venue for offering recommendations while maintaining the patient's freedom of choice (
31).
MI has been shown to have particular strengths for treating addictions and for addressing problems of persistent unhealthy behaviors, especially with patients who are angry or resistant to change (
6). Although MI was originally developed as a treatment modality for alcohol and substance abuse, a growing evidence base supports its increasing use in specialized medical settings, such as hospital emergency departments, trauma centers, and obesity treatment programs as well as broad applications in primary care (
32).
The following clinical example from the actual experience of the first author provides readers with a sense of the style and techniques of MI, emphasizing the differences between MI and a more traditional psychiatric intervention.
The police brought a 40-year-old woman to the psychiatric emergency room because while intoxicated she threatened to kill her partner and herself. She had no history of violence or of legal or psychiatric problems. When she became sober the next day, she reported calmly that she was an alcoholic and was not violent and had no intention of hurting her partner or herself. She wanted to be discharged. The typical psychiatric approach to this problem would be a combination of education and confrontation; the psychiatrist would explain the dangers of alcoholism to the patient and encourage her to seek treatment, handing her a list of alcohol treatment centers.
In contrast, the actual MI conversation proceeded like this:
Patient: I am an alcoholic and don't want to change. I am not dangerous; just let me go home now.
Psychiatrist: OK, that's what we'll do. We can't force you to change. Can I just ask you a few questions and then we'll let you out of here.
[MI: Respect for autonomy—the psychiatrist respects the individual's right to change or not to make a change; collaboration—the psychiatrist is equal to the patient in power and asks permission for further inquiry.]
Patient: OK.
Psychiatrist: I'm interested in learning a little about your drinking. I understand you don't want to change. So I am assuming that the alcohol is mostly a good thing in your life. I am wondering if there is anything not so good about the alcohol in your life?
[MI: Elicit ambivalence.]
Patient: Well, they said my liver is not so good anymore. It's going to fail if I don't stop drinking.
Psychiatrist: OK, so that sounds like one part of the drinking that's not so good.
[MI: Explore ambivalence.]
Patient: Right.
Psychiatrist: But it doesn't sound important enough to make you want to change. I'm guessing that you don't care so much whether your liver fails or not.
[MI: Not at all sarcastic here; really respecting her autonomy.]
Patient: Well, I can't live without a liver.
Psychiatrist: OK. Then it sounds like you don't care so much whether you live or die.
[MI: Again, not at all sarcastic; simply reflecting content and respecting autonomy.]
Patient: No way! I love life!
Psychiatrist: Well, I'm not sure I understand then. On the one hand, you are very sure that you are not going to stop drinking, yet you also say you love life and don't want your liver to fail.
[MI: Develop discrepancy. Elicit change talk.]
Patient: Well, I know I'm going to have to cut down or stop sometime. This is just not the time.
Psychiatrist: OK. I hear what you are saying. You do want to stop drinking at some point, to save your liver and to save your life—it's just not the right time now.
[MI: Listen, understand, express empathy, and reflect feelings; respect autonomy.]
Patient: Right.
Psychiatrist: OK. Can I ask another question or two? … If you do think you're going to stop at some point, I wonder what thoughts you've had about when and how you might want to stop drinking? Would you want or need any help if and when you decided to cut down or stop drinking?
[MI: Open questions for understanding; encourage change talk.]
This conversation led quickly to discussion about where and when the patient might go for help. She developed a specific action plan for health. Of course, this patient may not have followed through with her action plan, but the interaction using an MI approach seemed much more likely to lead to change than the more traditional educational/confrontational one.
This review will now turn to the evidence supporting the use of MI for treatment of addictions, then discuss the use of MI in general psychiatry practice for addressing the more widespread and underrecognized problem of risky drinking, and, finally, discuss the integration of MI principles and techniques into the more routine general practice of psychiatry.
RISKY DRINKING: RECOGNITION AND MANAGEMENT IN ROUTINE PSYCHIATRIC PRACTICE
Although alcohol dependence is a familiar concept to psychiatrists, risky drinking may be less familiar. At the very least, established criteria for risky drinking are less well known by psychiatrists, other physicians, and the general public. A brief review of the concept of alcoholism will differentiate the concepts of alcoholism and dependence from the concept of risky drinking and help explain the reason that psychiatrists should routinely address risky drinking in clinical practice.
With the demise of prohibition in the 1930s, new policies were needed to deal with drunkenness (
50). The search for a solution shifted away from a broad societal focus on alcohol as a toxic substance to anybody who consumed it toward an individual focus rooted in individual vulnerability, at that time labeled alcoholism. By the 1940s, well after prohibition ended, a confluence of factors highlighted the concept and catapulted it into the popular consciousness. Alcoholism became the focus of a national organization, a research institute, and medical and media attention. On the positive side, this concept increased medical research on the topic and led to more enlightened treatment of alcoholics. On the negative side, by creating a dichotomous entity, alcoholic or not alcoholic, the model had the potential to be misleading. Although people understood alcoholism as a severe and serious disease, they concluded that nonalcoholics do not need to concern themselves with how much they drank. Alcohol, the substance, was no longer the central problem and neither was the environment in which alcohol was served (restaurants and saloons) or the policies that influenced access; the focus shifted to a small number of individuals who were uniquely vulnerable to alcohol—alcoholics.
In this era, research with alcoholics documented that excessive drinking led to a variety of negative consequences, but only among patients who presented for specialized alcohol treatment. Studies of the association between alcohol and harm in the general population were not initiated until the 1960s. The most recent comprehensive, population-based survey shows that 71% of the U.S. civilian, noninstitutionalized population either does not drink or is drinking below the risky drinking threshold (
51) (
Figure 1). It also shows that a diagnosis of alcohol dependence applies to 3.8% of the population (
52). That leaves about 25% of U.S. adults who are not alcohol dependent but drink too much. They have either already experienced alcohol-related harm or, compared with the 71%, are at elevated risk for future alcohol-related harm.
Those statistics mean that for each individual in the population who is alcohol dependent, six other individuals drink too much but are not dependent. That 6:1 ratio has enormous implications. First, it suggests that the bulk of alcohol-related harm in the United States is associated with individuals who are not alcoholic or alcohol dependent. Second, it broadens our understanding of the fundamental problematic nature regarding excessive alcohol consumption. If we focus exclusively on the alcohol-dependent portion of the population, we may be ignoring a majority of society's alcohol problems.
What kinds of risks accrue from drinking too much? From the point of view of mental health, the risk of interest is alcohol dependence. Clearly, individuals who pursue risky drinking with focus and intensity are more likely to become dependent. For those individuals, competent practitioners need to know diagnostic criteria. From the point of view of public health, however, the risk is not so singular. Although alcohol dependence can be a severe and disabling disease, it is only one chronic disease outcome associated with drinking too much. Even when risky drinking is not accompanied by dependence, it regularly results in a wide variety of diseases and injuries, ranging from increased accidents (e.g., motor vehicle accidents or accidental overdose) to violence and many chronic diseases (
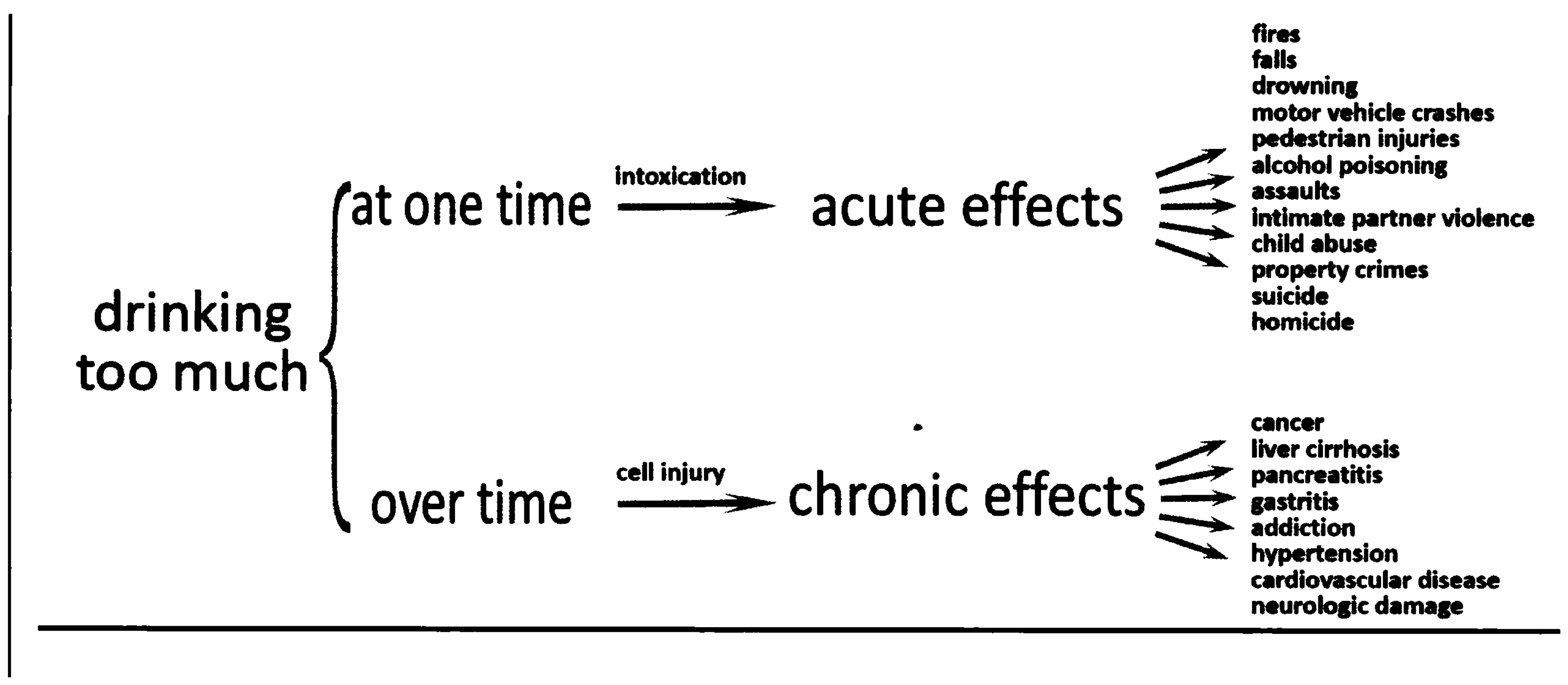
Figure 2).
When patients drink too much at one time, i.e., on a single occasion (“binge drinking”), the increased blood alcohol concentration (BAC) affects the brain, leading to impaired judgment, increased risk taking, and decreased muscle control (
53). The combination frequently leads to a variety of acute negative consequences. One example of a subacute problem of risky drinking would be fetal alcohol syndrome. From a chronic perspective, when people drink too much over time, cells in a variety of tissues throughout the body are damaged, leading to a variety of chronic diseases.
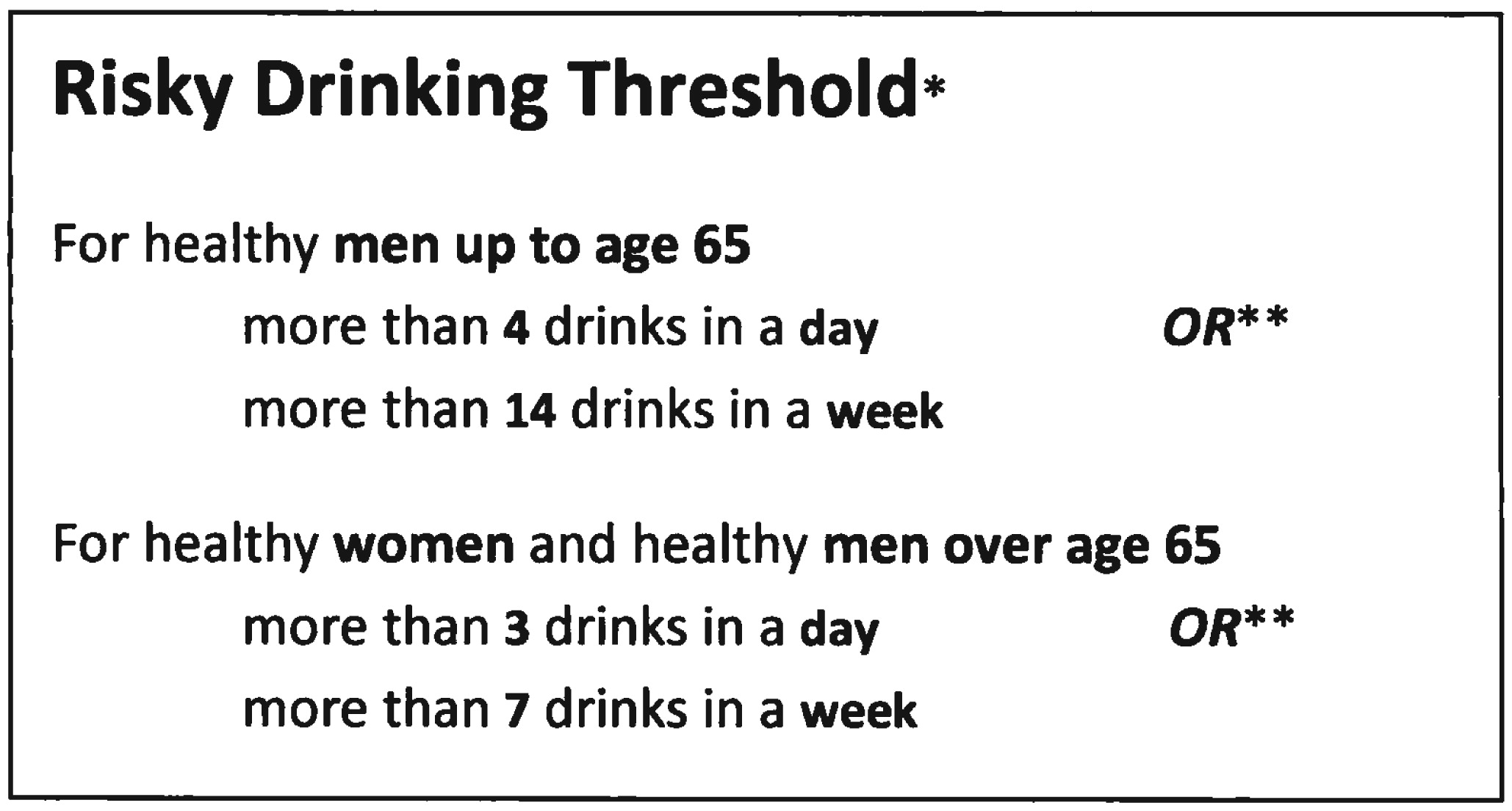
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) has proposed a risky drinking threshold that accounts for both the acute and chronic effects of alcohol, making it a reasonable cut point for dividing populations into groups that do and do not need an alcohol intervention, brief or otherwise. However, consumption below that threshold should not be considered low-risk drinking. The term
moderate drinking is avoided here because it has no uniform definition among health professionals (
54) and is widely misunderstood by the public (
54–
56). The NIAAA based its daily consumption limit at a level that would produce BACs of 0.08 g/dl from a single drinking occasion, clearly a risky level. However, it is also clear that levels just below that threshold, say levels that produced a BAC of 0.06 or 0.07, are also risky. A recent emergency department study found that patients who drank at levels below the NIAAA daily thresholds accounted for 50%–85% of the acute injury visits for falls, transport-related events, and interpersonal violence (
57). The U.S. Dietary Guidelines provide a more appropriate upper limit for low-risk drinking for the general population. They recommend up to two drinks a day for healthy men aged ≤65 years and up to one drink a day for healthy women regardless of age and healthy men aged >65 years (
58).
There are several reasons for psychiatrists to screen all their patients for risky drinking. Risky drinking may
2.
interact with medications to produce side effects or influence treatment efficacy,
3.
be a mode of self-medication,
4.
be a confounding factor for common psychiatric consultations, e.g., depression,
5.
be a factor in suicide attempts and suicide,
6.
be more prevalent in psychiatric practices than in the general population and other medical practices, and
7.
be the easiest way to identify patients early who are at the highest risk for future alcohol dependence.
Evidence is strong that screening with brief intervention is efficacious and effective (
59,
60), and it is recommended as a routine clinical preventive service (
61). Because the majority of screen-positive psychiatric patients will not typically be alcohol dependent, even psychiatrists who do not specialize in addiction treatment will be able to help them with as little as a few minutes of counseling. They will not need counseling for dependence but for behavior change. Some familiarity with the methods and approach of MI can be very helpful for the practicing psychiatrist interested in helping his or her patients decrease risky drinking behaviors.
The goal of screening is to quickly identify whether a patient's alcohol consumption is an issue that needs further evaluation. Although many alcohol screening instruments are available, most of them focus on identifying the DSM diagnoses of alcohol abuse and alcohol dependence and are, therefore, not useful in screening for risky drinking. The three self-report instruments described below are appropriate for identifying risky drinkers. Patients who receive positive screening results are either alcohol dependent or risky drinkers who are not dependent. Therefore, further evaluation will be necessary to identify which patients are dependent and so require more than a brief intervention. All three instruments are supported by research and easy to use.
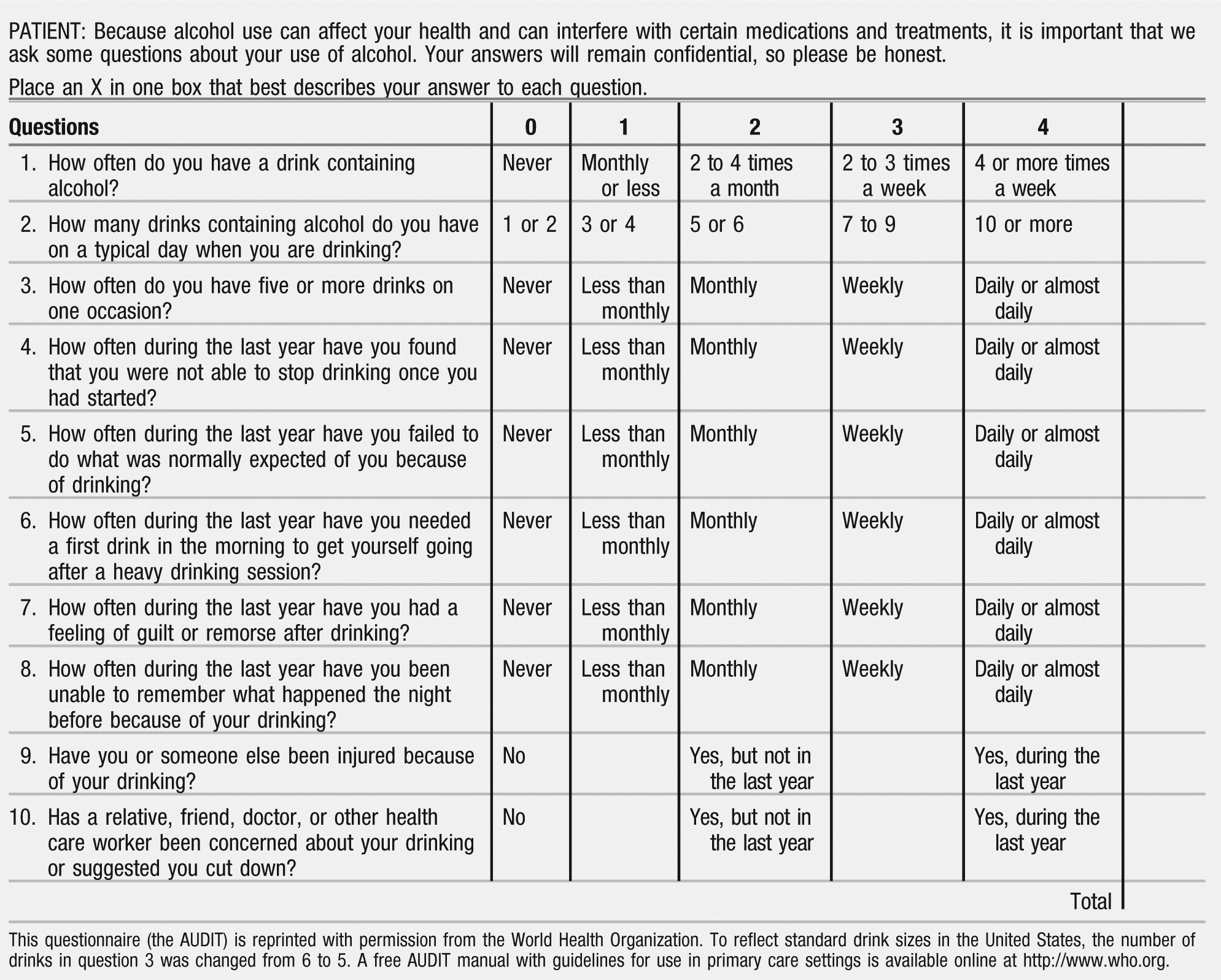
The Alcohol Use Disorders Identification Test (AUDIT) (see Appendix 1) was developed as part of an international study of alcohol screening and brief intervention sponsored by the World Health Organization (
62) and has been extensively studied (
63–
66). It has 10 self-report questions that measure the level of risk in three domains: alcohol consumption during the past year, alcohol-related harm, and alcohol dependence symptoms. It identifies four groups of people: abstainers and low-risk drinkers, those at risk because they drink excessively, those who have already experienced problems related to their drinking, and those who are likely to be alcohol dependent. The AUDIT is scored on a scale of 0–40 with a score of ≥8 as the most common threshold for a positive result. A manual for using the AUDIT is available online from World Health Organization. The AUDIT can be administered in 2–3 minutes through an interview, by the patient on paper, or by computer.
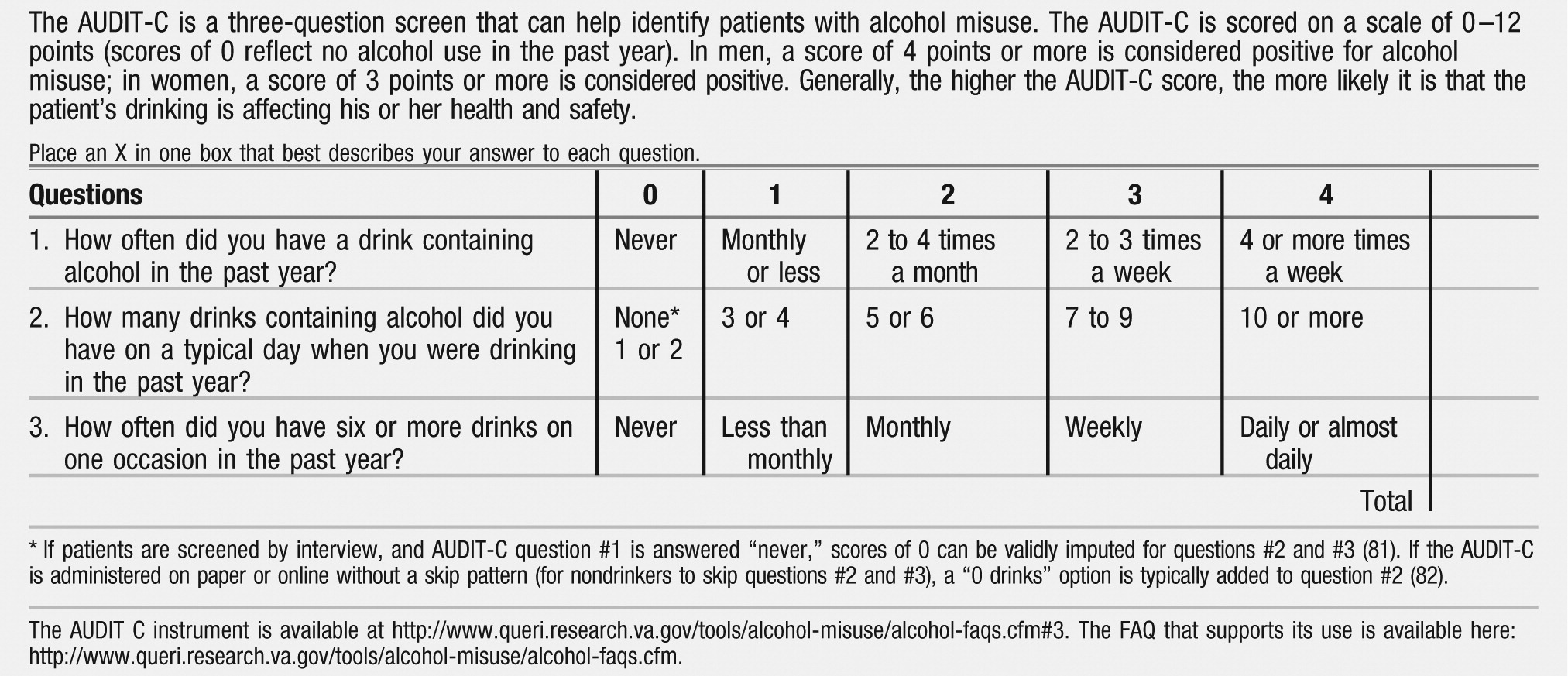
The AUDIT-C is a shorter instrument and uses the three AUDIT alcohol consumption questions to measure alcohol consumption during the past year (
67,
68) (see Appendix 2). It is scored on a scale of 0–12, with scores of 0 indicating no alcohol use in the past year. For men a score ≥4 and for women a score ≥3 is typically considered positive for risky drinking. Higher scores indicate that drinking is more likely to be affecting the patient's health or safety. The instrument and a detailed, useful FAQ is available from the U.S. Department of Veterans Affairs.
The final screening option is a one-question instrument that focuses on binge drinking: “When was the last time you had more than x drinks in 1 day?” (x=5 for men; x=4 for women). Patients who report having had the requisite number of drinks in the last 3 months are considered to have positive results. Although the instrument is short, its validity has been evaluated (
69,
70), and NIAAA recommends its use.
BRIEF ACTION PLANNING (B.A.P.): A MOTIVATIONAL INTERVIEWING TOOL FOR ROUTINE PSYCHIATRIC PRACTICE
Brief action planning (B.A.P.) is one application of MI that has been developed and disseminated and may be useful for general medical as well as routine psychiatric practice. Originally developed by the lead author as a self-management support and motivational tool for the Health Resources Services Administration (HSRA)/Institute for Healthcare Improvement
10 Health Disparities Collaboratives (
http://www.healthcarecommunities.org/), B.A.P. was promoted by the American Medical Association in 2008 (Appendix A, “Physician Tip Sheet for Self-Management Support” in reference
76) and soon will be included by the Commonwealth Fund for its Tool-Kit on the Medical Home. It has been disseminated by programs of the Centers for Disease Control and Prevention, HRSA, the Robert Wood Johnson Foundation, and the Veteran's Administration and used in the Improvement in Patient Care Program of the Indian Health Service. Workshops or courses on B.A.P. have been presented at recent scientific sessions (77–79). Early evidence supporting its efficacy was presented at the First International Conference on Motivational Interviewing (Interlaken 2008) (
80) and the Institute of Psychiatric Services (
81).
The tool is organized around three core questions and four supporting skills (see Appendix 3), all of which are grounded in the scientific literature of self-management support, stage of change theory, MI, and atheoretical communication and psychotherapy research. B.A.P. has high face validity and is generally well accepted by most practitioners because of its simplicity and practicality.
The basic application of B.A.P. is relatively easy to teach and use. It serves as a useful motivational tool to help many patients, especially those who may be relatively ready, with support and focused encouragement, to make action plans for health. For effectiveness as a motivational tool, however, B.A.P. must be used in a patient-centered manner, aligned with the spirit of MI.
What about those patients who are more ambivalent, more angry, or more refractory to change, those patients with persistent unhealthy behavior? Strategic application of 13 other well-defined communication and MI skills enables practitioners to use B.A.P. effectively with these patients with more complex problems. For these patients, advanced skills can be integrated in a stepped-care manner into the basic B.A.P. template. This stepped-care application of MI is called comprehensive motivational interventions (CMI™). CMI skills are described in a textbook (
82,
83) and web-based learning programs (
http://www.comprehensiveMI.com).