What's Up with Bipolar Disorder?
Abstract
Current and proposed DSM-5 definitions of bipolar disorder
Bipolar I disorder
Bipolar II disorder
Bipolar spectrum
DSM-5—proposed revisions
Duration of hypomania
A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 4 days and present most of the day, nearly every day, that is clearly different from the usual non-depressed mood (24).
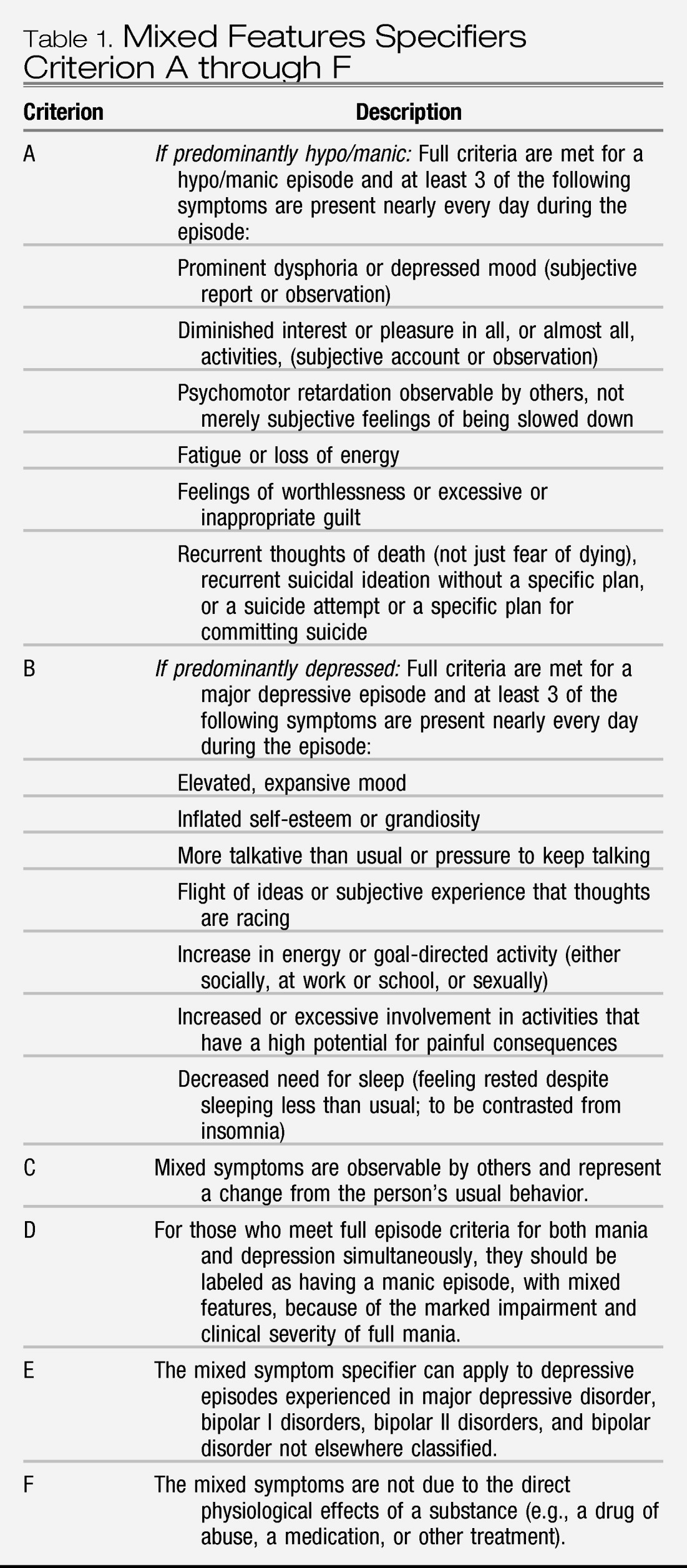
Mixed features specifier
Hypo/manic Criterion A: addition of activity/energy
A distinct period of abnormally and persistently elevated, expansive, or irritable mood AND abnormally and persistently increased activity or energy. Symptom lists (Criterion B) would be essentially not changed (25).
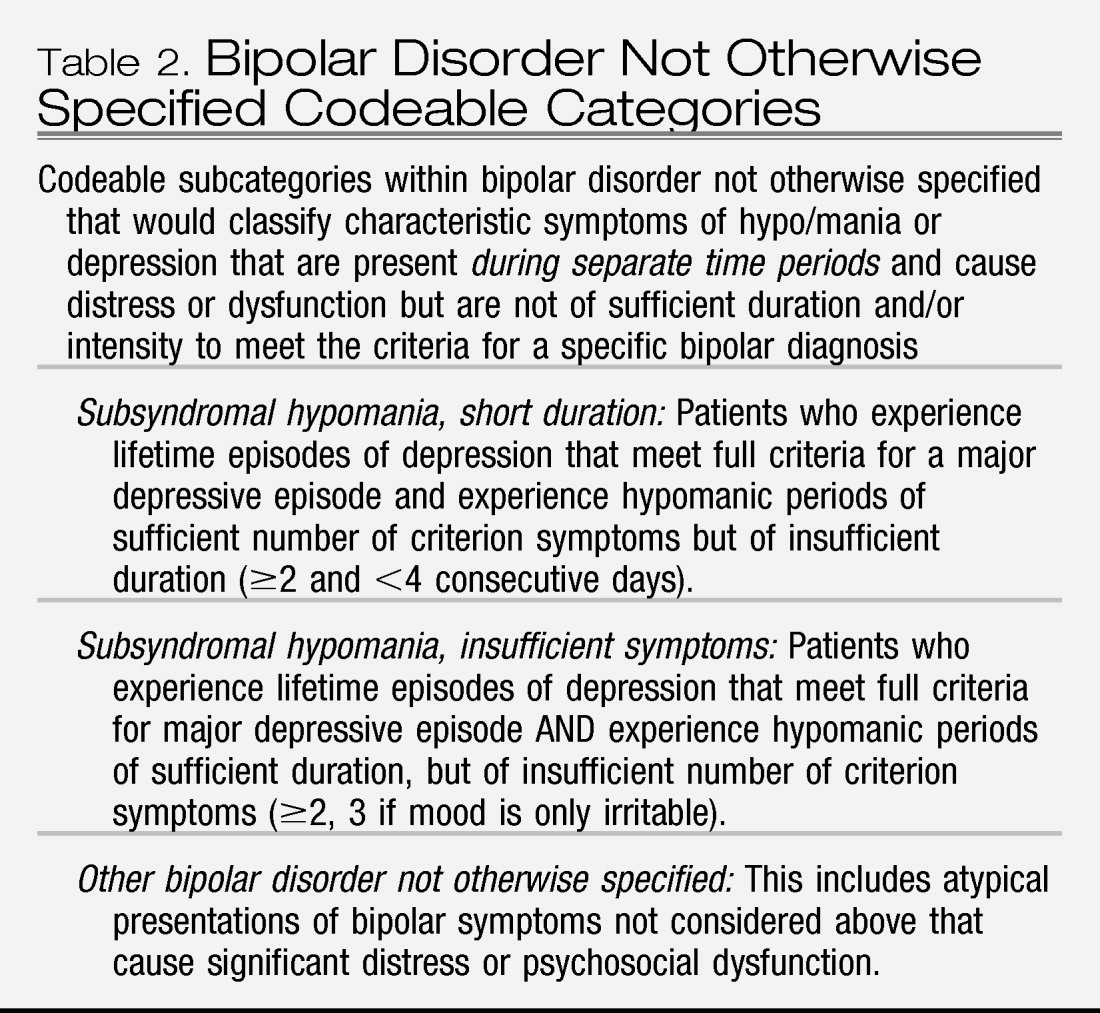
Bipolar disorder not otherwise specified revised to include specific types
Treatment innovation
Future innovations
Possible role of inflammatory and cellular processes in bipolar disorder
Summary
Acknowledgment
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

