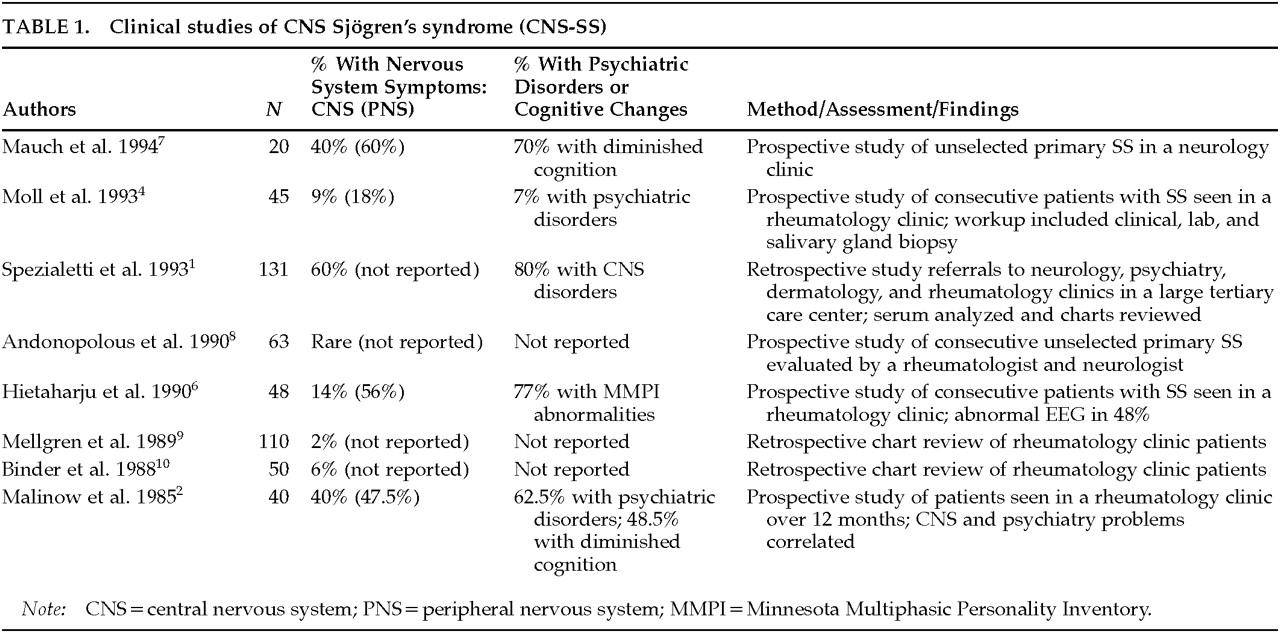
CNS Sjögren's Syndrome: An Underrecognized and Underappreciated Neuropsychiatric Disorder
Abstract
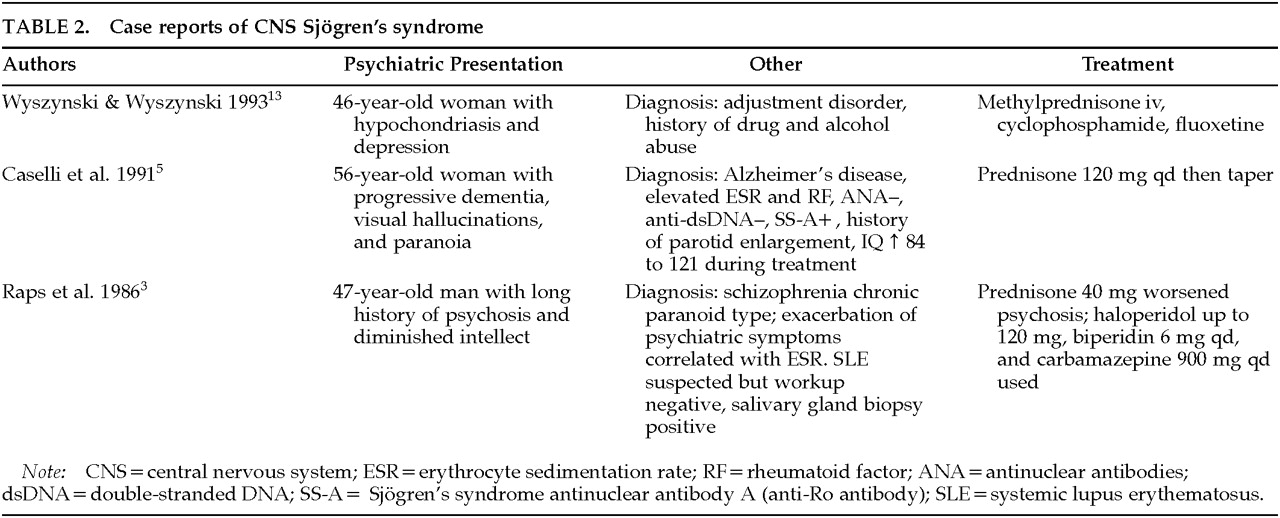
CASE REPORTS
Case 1. Ms. S. is a 54-year-old woman who reported a history of sarcoid but no psychiatric history prior to age 53. Five months prior to outpatient psychiatric referral, she had fallen. After a negative medical evaluation, she was transferred to a psychiatric facility and placed on loxapine and diphenhydramine to treat ideas of reference and bizarre ideation. Historical material provided by the patient that could be construed as psychological but that could also reflect underlying brain disease included the patient's questioning her sexual orientation after many years of a stable and previously satisfying married life and a recent increase in exploring new lines of work.Negative MRI and magnetic resonance angiogram (MRA) ordered during her medical hospitalization made CNS sarcoid appear unlikely. At her initial psychiatric outpatient presentation she was not psychotic, but her recent history included increased capacity for work (three jobs), decreased sleep, rapid speech, and ideas of reference. Diphenhydramine was decreased and loxapine switched to haloperidol.After 2 months of treatment with haloperidol, she began to exhibit symptoms consistent with a major depressive disorder. Consequently, she was begun on 10 mg of paroxetine. She subsequently briefly stopped haloperidol, but fearfulness and paranoid ideation recurred.Six months later, Ms. S. was admitted to the neurology service for evaluation of new-onset hemiparesis. MRI and MRA indicated vascular lesions and vasculitis. An antinuclear antibody (ANA) titer was positive at 1:1,280. SS-A (Anti-Ro antibody) was positive and SS-B (Anti-La antibody) negative. Other markers for systemic lupus erythematosus (SLE) were negative. Chart review revealed multiple clinic visits for sinusitis and conjunctivitis related to dry mouth and eyes.When she was started on prednisolone to treat purported pulmonary sarcoidoses, her paranoia remitted. At lower steroid doses, manic symptoms worsened and she began to exhibit bizarre behavior. She is currently being maintained on prednisolone at a dose of 7.5 mg qd. Her only psychiatric medication is divalproex 750 mg qd. The medical team is now questioning the diagnosis of pulmonary sarcoid. A lung biopsy would assist greatly in differentiating the caseating granulomatous process of sarcoid from the mononuclear inflammatory process often found in Sjögren's syndrome;11 however, because the patient has improved clinically, a biopsy has not been done.
Case 2. Ms. R. is a 47-year-old woman who presented to the psychiatry service for treatment of recurrent depression manifested by depressed mood, lethargy, diminished pain tolerance, and diminished libido. She also reported difficulty at work due to persistent fatigue and chronic cough. Six months earlier, she had responded to fluoxetine at a dose of 20 mg qd, but she stopped the medication because of side effects. Her depressive symptoms recurred and her work difficulty continued.At her initial outpatient psychiatric evaluation, she complained of fatigue, hopelessness, feelings of discouragement, a diminished libido, poor concentration, and short-term memory disturbance. A review of her medical history revealed 4½ years of persistent nonproductive cough, frequent sinus problems, a long history of recurrent urinary tract infections with possible interstitial cystitis, two episodes of easy bruising, arthralgias without joint effusions, and myalgias. She also had an extensive medical workup for a lung infiltrate that was negative on biopsy, although erythema of the mucosa was noted on bronchoscopy. She was begun on isoniazid for treatment of a presumed case of tuberculosis based on her history of TB exposure and having a positive tuberculin purified protein derivative test (PPD). Unfortunately, this treatment regimen was not effective. Focused questioning revealed subjective complaints of dry eyes and mouth. A previous ANA titer ordered by her primary care physician was positive at 1:320, as was double-stranded-DNA (dsDNA); however, other SLE markers were negative. Clinical evidence of inflammatory processes required to diagnose SLE was also absent. Tests of the complement system (C3 and C4) were negative. A diagnosis of fibromyalgia was considered, but the patient lacked the requisite number of tender spots found on physical examination of the joints and extremities.At the time of her presentation to the psychiatry service, an ANA titer was positive at 1:80 (speckled), but both SS-A (Anti-Ro antibody) and SS-B (Anti-La antibody) were negative. Venlafaxine was clinically effective but caused side effects that the patient could not tolerate. Buproprion was begun and partially relieved some depressive symptoms (frustration intolerance, hypersomnia, irritability, hopelessness, and guilt) but did not adequately address fatigue, myalgias, or cough.The patient had an unsuccessful trial of antireflux therapy for her chronic cough. Prednisone at 5 mg qd was started. After being treated with bupropion 300 mg qd for 3 months, her fatigue, myalgias, and cough improved, and her depressive symptoms improved further. Shirmer's test (to quantify tear production) was positive, and a gingival biopsy revealed chronic sialadenitis without a mucosal lesion. She is currently being maintained on prednisone 10 mg qd. Her only psychiatric medication is bupropion 300 mg qd.
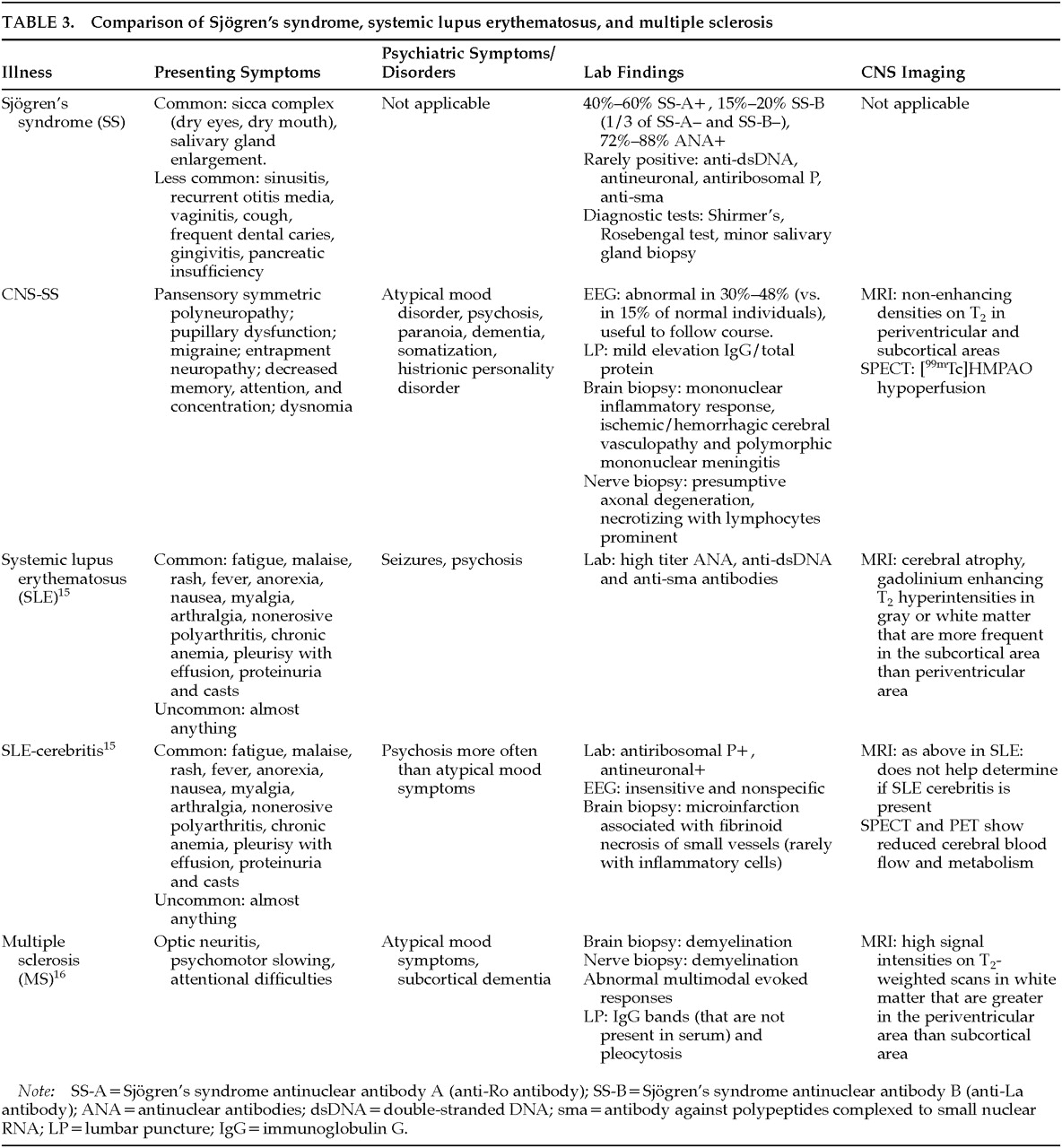
BACKGROUND
PATHOLOGY
DIAGNOSIS
MEDICAL WORKUP
PSYCHIATRIC ILLNESS
TREATMENT
CONCLUSION
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).