There are many important questions regarding the nature of laughter and its occurrence as disease. In particular, the neuropathology of laughter remains ill defined. Laughter appears to result from a variety of neurological lesions. We report an unusual and extreme case of a patient who had involuntary laughter and inappropriate hilarity present for most of the day for over two decades. We further review the literature on the origin and neuropathological basis of the behavior and suggest an approach to clinical disorders of laughter.
CASE REPORTA 67-year-old man presented for evaluation because of a 20-year history of unremitting laughter. His illness began after the rupture of an anterior communicating artery aneurysm with subsequent bifrontal injury from surgical retraction and clipping of the aneurysm. Postoperatively he developed hydrocephalus, which had necessitated placement of a ventriculoperitoneal shunt. Since recovering from his two operations, the patient had not been able to stop laughing. To the utter annoyance of his family and friends, the patient spent most of the day laughing, even when he felt sad. His laughter intruded in all of his conversations and was triggered by the most trivial and inconsequential stimuli. Only sleep provided respite from laughing. In recent months, his laughter had become even more disturbing to his family. Furthermore, because of inability to stop laughing, the patient had not been able to work. His past medical history was otherwise positive for many attempts to control his laughter with psychoactive drugs.
On examination, he was an alert man who would quickly burst into laughter with the slightest provocation. His Mini-Mental State Examination
4 score was 22/30; he missed five orientation questions and three recall items. Language examination was normal, and he generated a list of 11 animals/minute. On memory testing, he could not recall any of 4 words at 5 minutes but did better on recognition testing. He was intact in visuospatial skills, calculations, and praxis; however, his interpretations of idioms and proverbs were concrete, and alternating programs were performed with difficulty. Examination of his cranial nerves disclosed a left lateral rectus palsy, present since childhood; a hyperactive gag reflex; and a brisk jaw jerk. His gait was wide-based, with mild spasticity in the lower extremities. The reflexes were brisk in the lower extremities, with bilateral upgoing toes. He had no glabellar, snout, or grasp reflexes.
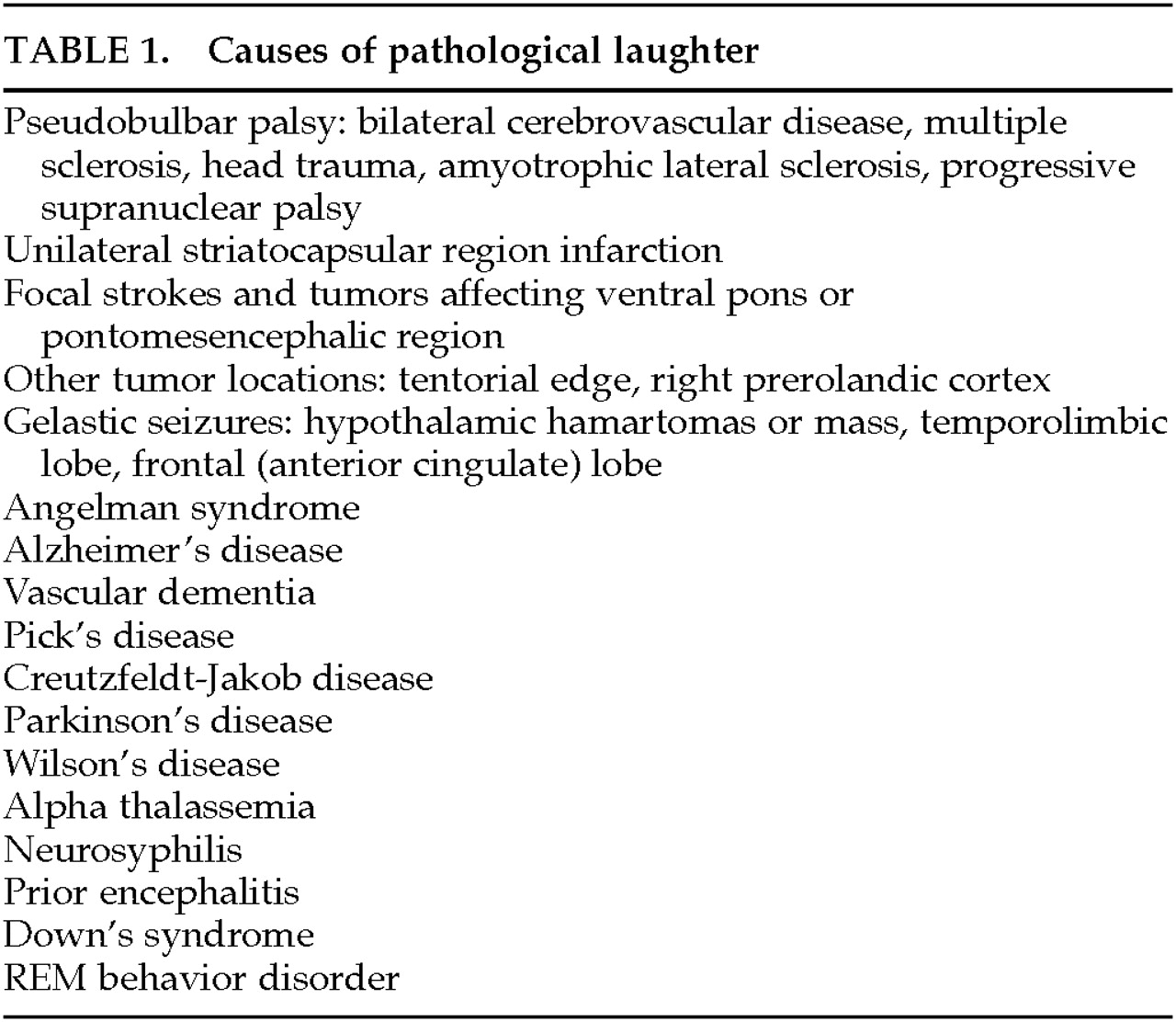
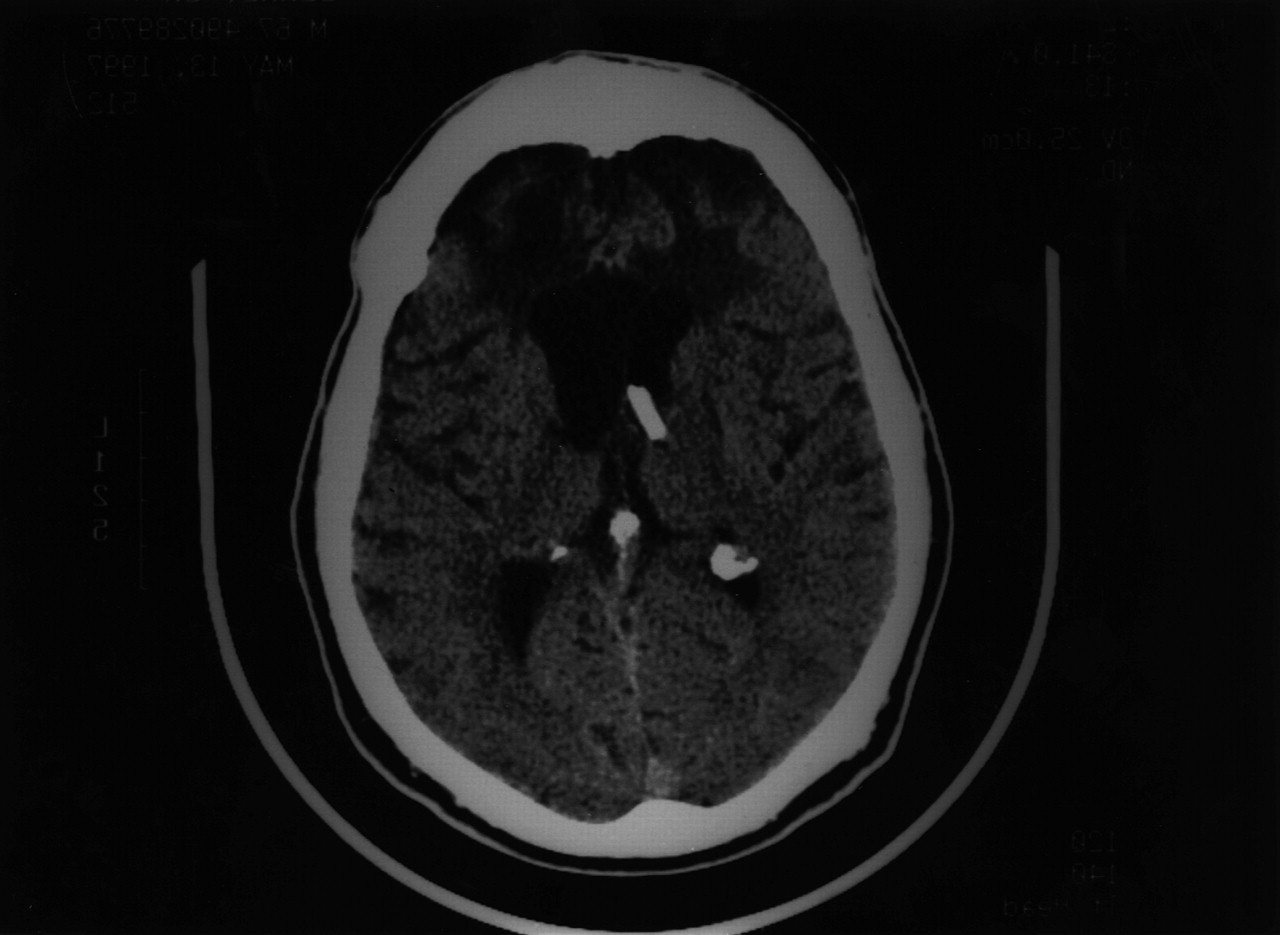
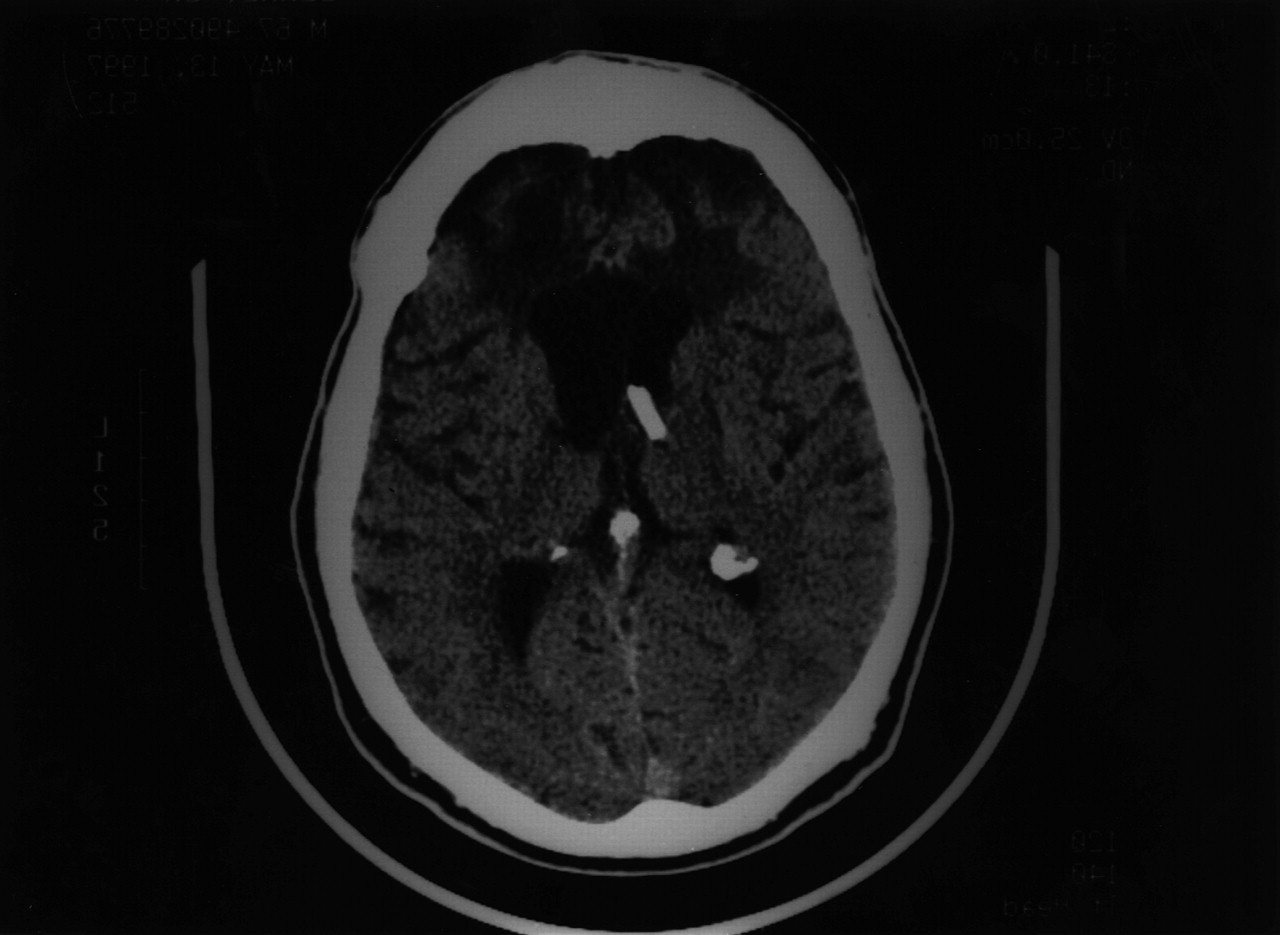
CT scans of the brain showed bifrontal encephalomalacia, an aneurysm clip in the anterior circle of Willis, and a right ventricular shunt (
Figure 1). PET scans disclosed medial bifrontal hypometabolism (
Figure 2).
The patient was started on fluoxetine at 10 mg qd, which diminished his episodes of laughter but did not abolish them. Pathological Laughter and Crying Scale scores,
5 obtained retrospectively, decreased from 26 before treatment to 15 after 2 weeks on fluoxetine. A neurosurgical assessment concluded that his shunt had been nonfunctional for many years.
DISCUSSION
For more than two decades, this patient could not keep from laughing even when he did not detect humor. His examination disclosed memory impairment, frontal-executive dysfunction, and a gait disorder with lower extremity pathological reflexes, consistent with his bifrontal encephalomalacia and hydrocephalus. His involuntary laughter was secondary to pseudobulbar palsy and may have been facilitated by disinhibition of the anterior cingulate gyrus.
Understanding the origin and nature of laughter facilitates understanding the disorders of laughter. Laughing in humans has no close equivalent in other animals. The ability to laugh emerges in about the third or fourth month of life, long after the ability to cry and smile. Laughter does not have the same origin and purpose as smiling.
6 The smile emerged from the silent, bared-teeth display in primates and conveys social affinity, reassurance, sympathy, or greeting.
2 Laughter, on the other hand, emerged from the relaxed, open-mouth display in primates and occurs during rough-and-tumble play in chimpanzees.
Laughing is the physiological opposite of crying. Although the upper half of the face is indistinguishable from the crying face, the lower face and respiratory pattern are the reverse of crying. In laughter, there is opening of the mouth, pulling back and up of the corners of the lips, slight raising of the upper lip, and deep inspirations followed by short, interrupted spasmodic expirations (expiratory clonus).
7 These movements originate from a bulbar, lower brainstem center for laughter that is under higher cerebral control; laughter does not occur in anencephalic children.
7Laughing is also the psychological opposite of crying. It conveys a lack of distress, a recognition that the “danger” is not real.
2 Laughter needs a receptive social context where assertive behaviors, such as tickling or rough play, are recognized as mock aggression or mock seriousness. In humans, the appreciation of the incongruity of mock aggression may have led to the appreciation of incongruity in mirth or humor. An incongruous relationship between what is perceived and what is expected is the essence of humor.
1 Laughter may serve to promote the social exploration of perceptive/cognitive mismatch, the ability to see things in a different light. Furthermore, laughter is rewarding to the humorist and encourages him or her to continue to provide incongruous information.
8Disorders of laughter are distinct from disorders of mirth or humor, such as moria or witzelsucht. Moria (foolish or silly euphoria) and witzelsucht (a tendency to inappropriate jokes) occur with frontal lobe disorders such as neurosyphilis.
7,9 Patients with these disorders have a habitual routine of jokes and witticisms, but they are paradoxically insensitive to humor. The right orbitofrontal region may be the neuroanatomical substrate for these behaviors.
9The most common disorders of laughter are associated with pseudobulbar palsy.
7,10 Although less common than pathological crying, pathological laughter in pseudobulbar palsy can be triggered by trivial stimuli, it can be incongruent with the underlying mood, and it can be intermixed with crying. Features of pseudobulbar palsy may include dysarthria, dysphagia, bifacial weakness, increased mandibular reflex, preserved or increased palatal reflexes, and weak tongue movements, but preserved coughing, yawning, laughing, and crying. Pseudobulbar affect is secondary to bilateral interruption of supranuclear innervation of bulbar motor nuclei of the lower face and brainstem centers.
11 Bilateral strokes, multiple sclerosis, and severe brain trauma, usually greater in the right hemisphere, are the most common causes of this syndrome.
7,10–12Pathological laughter can also result from unilateral brain lesions in the absence of pseudobulbar palsy. Ceccaldi et al.
11 reported inappropriate laughter for 1 to 2 months after unilateral subcortical infarctions involving the striatocapsular region,
11 and other investigators report laughter following unilateral strokes in the lenticulocapsular area and in the right pontomesencephalic region.
13,14 A sudden display of laughter, “
le fou rire prodromique,” may precede acute strokes involving left internal capsule-thalamus,
15 left basal ganglia,
16 or ventral pons, especially on the left.
17,18 Laughter sometimes precedes other manifestations of tumors around the brainstem, such as a trigeminal neurinoma or a clival chordoma in the prepontine cistern compressing pontomesencephalic structures.
19,20 Posterior fossa lesions have produced laughter on elicitation of an intention tremor or on initiation of eye movements.
21 Finally, transient laughter may rarely result from unilateral lesions outside the capsular and ventral pontine regions, such as a hemangiopericytoma impinging on the right peduncle and a right glioblastoma in the prerolandic cortex.
22,23Gelastic (laughing) seizures are another neurological cause of laughter. Ictal laughter is stereotyped, is not precipitated by external stimuli, and is usually less than 30 seconds in duration. Gelastic seizures usually originate from the left hemisphere, whereas dyscrastic (crying) seizures usually originate from the right hemisphere.
24 Gelastic seizures most commonly result from hypothalamic hamartomas, sometimes with release of gonadotropins and other hormones.
25–28 These seizures may abate with resection of the hamartoma, but not with focal cortical resection.
29,30 Hypothalamic extension of other tumors can also produce laughing seizures.
31 In addition, gelastic seizures can be complex partial seizures of temporal lobe origin or of frontal lobe (anterior cingulate) origin.
26,32 Electrical stimulation in temporal regions can produce bursts of laughter accompanied by feelings of mirth or the subjective feeling of merriment.
26 In other studies, gelastic seizures have originated from the left frontal region,
33 the right frontal region,
34 the left anterior cingulate gyrus,
26 or the right anterior cingulate gyrus.
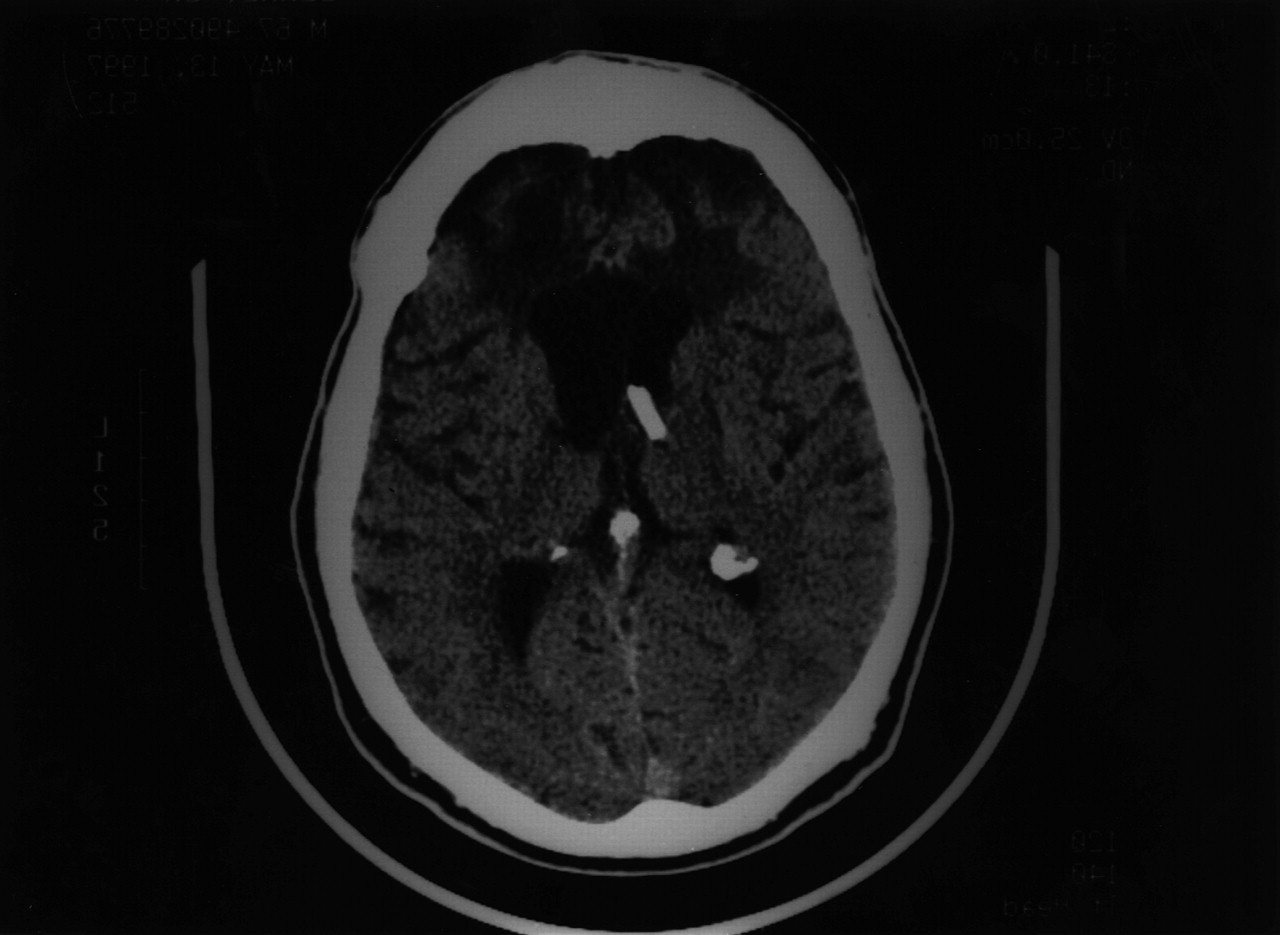
35Abnormal laughter may result from a number of other disorders (
Table 1). Angelman syndrome is a genetic disorder usually caused by maternal deletions at 15q11–q13 and characterized by mental retardation; seizures; microcephaly and other dysmorphic features; stiff, puppetlike movements; and frequent bursts of laughter.
36,37 Although it usually occurs between the ages of 2 and 16 years, Angelman syndrome can occur in adults up to 53 years of age and may relate to left frontal hypoperfusion.
38,39 Alzheimer's disease is associated with inappropriate laughter in as many as 14 percent of patients, possibly consequent to the presence of subcortical atrophy.
40 Yamada et al.
41 reported a 54-year-old woman with pathologically proven Pick's disease who was mute except for episodes of spontaneous chuckling incongruent to the situation. Creutzfeldt-Jakob disease,
42 alpha thalassemia with mental retardation,
43 Parkinson's disease,
10 and Wilson's disease can manifest with pathological laughter.
10 Finally, in REM behavior disorder, laughing spells occur at night, often during a stage of admixed REM and concomitant low-voltage mixed-frequency brain waves.
20These diverse conditions associated with pathological laughter suggest a neuroanatomic circuitry for the production of laughter (as shown in
Figure 3). First, the anterior cingulate gyrus endows experiences with emotional consciousness and is partially under frontal cortical control.
44 The anterior cingulate is also involved in the expression of emotion, particularly emotional vocalizations such as laughter. Second, the amygdalae in the temporal lobes feed back to the anterior cingulate for the emotional coloring of perceptions, and the temporal (parahippocampal and fusiform) cortex integrates perceptions with prior experiences. Third, the caudal hypothalamus, the central coordination center for internal emotional changes, is an effector of laughter.
7 Fourth, the ventral pontomedullary center for laughter coordinates emotional vocalization, facial expression, and expirations.
7,45 Finally, bilateral corticobulbar tracts tonically suppress laughter and oppose extrapyramidal connections for emotional expression. In addition, unilateral capsular lesions may produce temporary synkinetic laughter from crossover of activated but damaged voluntary motor pathways to these extrapyramidal pathways for laughter.
15We postulate that our patient had unusually severe pathological laughter from pseudobulbar palsy plus bilateral release of the anterior cingulate gyrus from frontal cortical control. This model differs from crying in the higher level of cortical integration required for laughter.
7 This model also can generate testable predictions regarding specific lesions that could produce pathological laughter.
The formulation presented here provides a framework for beginning to understand the disorders of laughter. Important clinical distinguishing features include
1.
Presence of associated feelings of mirth or humor, as in some seizures from anterior cingulate gyrus or temporal lobes.
2.
Precipitation by trivial or paradoxical stimuli, as in pseudobulbar palsy.
3.
Presence of acute neurological deficits as in capsular or peripontine lesions.
4.
Presence of mixed laughter-crying, as in pseudobulbar palsy.
5.
Occurrence as brief bursts or spells, as in gelastic seizures.
6.
Presence of other associated features, such as stimulus-specific laughter in some posterior fossa lesions and precocious puberty with hypothalamic hamartomas.
Pathological laughter is disturbing for most patients and demands intervention. The Pathological Laughter and Crying Scale is a reliable instrument for quantifying and monitoring response to treatment.
5 Pathological laughter may respond to tricyclic antidepressants, such as nortriptyline (25–100 mg/week).
5 Recent studies indicate that fluoxetine, fluvoxamine, sertraline, and other selective serotonin receptor inhibitors can ameliorate involuntary laughter, as in our patient.
46,47 Treatment with antidepressant medications is of particular benefit in patients with pathological laughter from pseudobulbar palsy from cerebrovascular disease or multiple sclerosis.
10 Antiepileptic mood stabilizers such as carbamazepine, valproate, or gabapentin have had modest success in decreasing laughter unless it is due to gelastic seizures. Other therapeutic possibilities include lithium, other antimanic therapy, and surgical management of focal lesions. Clearly, more work needs to be done on the management of this syndrome.