Acquired brain injury (ABI) may be complicated by neuropsychiatric syndromes such as depression, mania, psychosis, and disinhibition.
1 Patients experiencing these symptoms may be referred to mental health systems that lack the expertise or resources to identify and manage the complex array of neurobehavioral factors.
2 In patients with preexisting psychiatric disorders, ABI may change the clinical presentation and treatment response of their illness.
3Divalproex sodium, an anticonvulsant with mood-stabilizing properties, has demonstrated effectiveness in treating a wide variety of primary psychiatric disorders, in addition to those induced by ABI and degenerative dementias,
4 and is emerging as a safe and effective treatment for ABI-induced agitation in acute and sub-acute rehabilitation settings.
5,6 The present study sought to examine the efficacy of divalproex sodium in managing neuropsychiatric disturbances in community-dwelling psychiatric patients with a remote history of ABI.
RESULTS
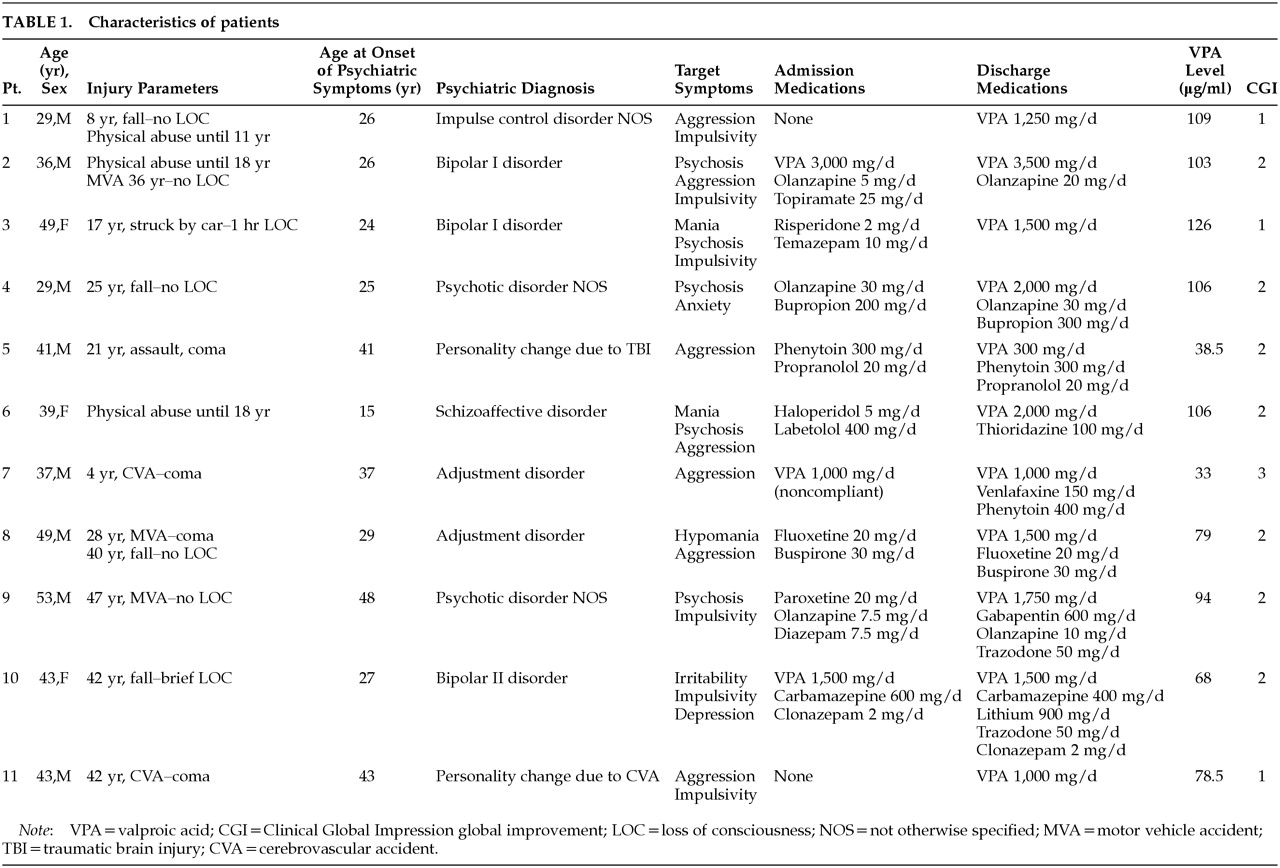
Patient demographics, injury parameters, and concomitant medications are presented in
Table 1. The sample consisted of 8 males and 3 females with a mean age of 40.7±7.8 years. The mean age at onset of psychiatric disturbance was 30.9±10 years. All patients were functionally independent and living in the community. Psychiatric diagnoses included bipolar disorder (
n=3), psychotic disorder not otherwise specified (
n=2), personality change due to acquired brain injury (
n=2), adjustment disorder (
n=2), schizoaffective disorder (
n=1), and impulse control disorder not otherwise specified (
n=1). Four patients (36.4%) had concomitant substance abuse disorders. Symptoms upon initial evaluation included physical and verbal aggression (
n=7), psychosis (
n=6), impulsivity (
n=5), elevated mood (
n=4), and depression (
n=1). Seven patients were injured in accidents; 3 were victims of physical abuse with or without additional accidents; 2 suffered cerebrovascular accidents; and 1 was injured in an assault. The age at time of injury ranged from 4 to 47 years. SPECT scans obtained as part of each patient's clinical evaluation demonstrated reduced orbitofrontal perfusion in all patients and reduced temporal perfusion in 72.3% of patients.
The mean daily dose of divalproex was 1,818±791 mg/day, with a mean serum valproic acid level of 85.6±29.6 μg/ml. Mean CGI improvement score was 1.9±0.5. Three patients were rated as extremely improved, 7 patients were much improved, and 1 patient was minimally improved. There was a negative correlation between serum valproate level and CGI improvement score (r=–0.73, P<0.01). This finding suggests a possible association between higher serum levels and better response, but the small sample size limits the power of the study. Patients all tolerated their medication regimens without adverse effects.
DISCUSSION
This study is limited by its uncontrolled retrospective design, small sample size, and patient heterogeneity. Injury mechanisms ranged from repetitive physical abuse to spontaneous subarachnoid hemorrhage. The presenting psychiatric symptoms varied considerably, and patients were receiving a wide range of concomitant psychoactive medications. Despite the diagnostic heterogeneity of our sample, aggression, psychosis, and impulsivity, either alone or in combination, were observed in all patients. Moreover, all of our patients had evidence of orbitofrontal damage and nearly three-quarters demonstrated temporal lobe hypoperfusion.
ABI frequently causes persistent changes in personality, emotion, and impulse control that may contribute to family distress and poor longitudinal outcomes.
7 The mechanism mediating these neuropsychiatric complications of ABI is not well understood. Orbitofrontal and temporal basal polar lesions are associated with behavioral disturbances in both traumatic brain injury (TBI) and stroke.
8,9 The orbitofrontal cortex is the only cortical structure with direct efferent connections to the hypothalamus, amygdala, and brainstem biogenic amine nuclei. Thus, this region may play a vital role in mediating arousal and instinctive behaviors, in particular aggression and impulsivity.
10Jorge et al.
11 have suggested that orbitofrontal damage may induce subictal kindling due to denervation hypersensitivity in limbic structures. This kindling could enhance dopaminergic mesocorticolimbic transmission, which may in turn contribute to manic, disinhibited, and psychotic states. A common presentation in such cases is a dysphoric mixed bipolar syndrome characterized by dysphoria, irritability, and aggression.
12,13 Our patients suffered from a wide variety of dopamine-dependent symptoms, including mania, aggression, and psychosis, and all demonstrated evidence of orbitofrontal damage on cerebral SPECT scans. These findings are consistent with the hypothesis of hyperdopaminergic states resulting from ABI-induced kindling. Moreover, the wide range of symptoms that appeared to improve in our sample suggests an antikindling rather than a primary antimanic therapeutic effect of divalproex.
Carbamazepine and valproic acid are effective mood stabilizers that inhibit limbic kindling in animal models.
14 Both medications have been used effectively in managing brain-injured patients in the acute neurorehabilitation setting.
6,15 Divalproex sodium, however, may be superior to carbamazepine with respect to cognitive side effects in brain-injured patients.
16,17 Single and multiple case reports cite its effectiveness in reducing agitation, aggression, and affective lability in patients with TBI,
18,19 epilepsy,
20 anoxia, and dementia.
21 Total daily dosages of 750–1,500 mg with serum levels of 50–110 μg/ml were described in these reports. In a retrospective study of 29 acutely brain-injured patients, Chatham Showalter and Netsky Kimmel
6 found that a mean dosage of 1,250 mg/day led to rapid response within 1 week, a time frame consistent with our experience.
Agitation in acutely brain-injured patients has been conceptualized as a subtype of delirium in coma-emerging patients.
22 Our postacute, community-dwelling patients represent a clinically distinct population from those in the Chatham Showalter series. Rather than demonstrating symptoms of coma-emerging delirium, our patients were experiencing symptoms consistent with a limbic kindling model of psychopathology. This is the largest case series reporting the use of divalproex sodium in managing postacute neurobehavioral complications of ABI and complements Chatham Showalter and colleague's acute care study. None of our patients experienced adverse side effects or significant drug–drug interactions. The mean dosages of divalproex and serum levels in our patients were substantially higher than those described in previous reports.
Divalproex sodium, either alone or in combination with other psychotropic medications, appears to be well-tolerated and effective in reducing a broad range of neurobehavioral symptoms in community-dwelling patients with a remote history of ABI. We suggest that the antikindling effects rather than a specific antimanic effect of divalproex is responsible for its broad range of benefits, and that limbic kindling may be responsible for a wide spectrum of ABI-induced psychopathology. The therapeutic effect may be dose-dependent, suggesting that the use of higher doses may be warranted in patients who fail to respond at lower serum levels. These preliminary findings await replication in larger, prospective trials.