Geriatric Treatment Center: A Contemporary Model for Collaboration Between Psychiatry and Neurology
Abstract
CASE REPORTS
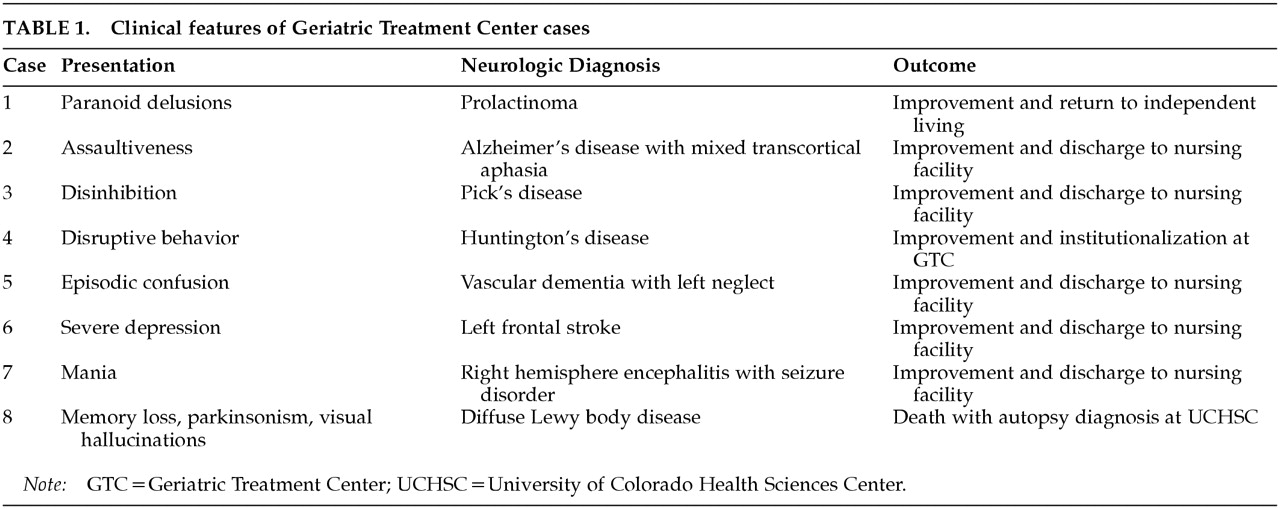
Case 1. A 71-year-old right-handed man was admitted involuntarily because of progressive delusional thinking, agitation, and irritability. He had had numerous confrontations with the police in the months preceding his admission and had violated a restraining order by refusing to desist from harassing a local child care center. He had bizarre and rigid beliefs that were inappropriately patriotic; he was noted to walk 10 to 25 miles daily displaying an American flag and to complain that children at the care center were not required to recite the Pledge of Allegiance often enough. Marital discord had led to his separation from his wife in the previous year. Although most evident in the past 6 to 12 months, problems with interpersonal relationships for the past 15 to 20 years had led to job instability and increasing isolation. His past medical history was unremarkable, and he was taking no medications on admission. There was no history of alcohol or illicit drug use. He was a university graduate who had earned a master's degree in library science, married, and had three children before the onset of interpersonal difficulties.Mental status examination showed him to be disheveled, tangential, and irritable. The most striking feature of his presentation was delusional thinking, and he had significant paranoia centering on the police in his community. His affect ranged from tearful to euphoric. He was fully oriented but would not cooperate with formal mental status testing. The elemental neurologic examination was normal. Some aspects of his clinical picture suggested mania, although the late age of onset for bipolar disorder was considered highly unusual.His hospital course was characterized by extremely uncooperative behavior that eventually required seclusion and restraints and emergency intramuscular haloperidol. He was calmed by the medication to some extent, and he then allowed diagnostic testing. Blood and urine tests were unremarkable, but computed tomography (CT) and magnetic resonance imaging (MRI) scans of the brain showed a cystic suprasellar mass. Behavioral neurology consultation was provided, and after discussions with the Endocrinology Service at UCHSC, further workup disclosed a prolactin level of 755 ng/ml (normal<20 ng/ml), indicating that the lesion was likely a prolactinoma. Additional testing revealed that he had no visual field deficits and that his neuropsychological function was normal with the exception of very subtle memory disturbance.The patient was treated with bromocriptine, and his behavior showed dramatic improvement. He became cooperative, rational, and euthymic. One month later, he was discharged to live in an apartment, and shortly before he left the hospital, his prolactin level was found to be less than 5. The use of bromocriptine clearly contributed to an excellent outcome, and it is plausible that the prolactinoma, a slow-growing benign tumor, was a major or even the sole cause of the neuropsychiatric syndrome. This case also emphasizes the importance of an accurate diagnosis. If the tumor had not been discovered, long-term treatment with dopamine-blocking drugs would have been likely; these agents could exacerbate the problem by increasing serum prolactin levels and promoting tumor growth.6
Case 2. A 60-year-old man with bipolar disorder and non–insulin-dependent diabetes mellitus was admitted for assaultive behavior that could not be managed in the community. He had experienced both mania and depression for the past 20 years, but multiple treatments, including a variety of mood stabilizers and antidepressants, had permitted him several extended periods of relative psychiatric stability. Neuropsychological testing during one of these periods disclosed a Wechsler Adult Intelligence Scale7 full scale IQ of 112 (Verbal 106, Performance 120). However, in the four years prior to his admission, cognitive impairments became increasingly apparent. He had been seen at the UCHSC Neurology Clinic at the onset of this problem, at which time mild memory deficits were observed. Neuropsychological testing then demonstrated a decline in his full scale IQ to 97 (Verbal 88, Performance 113), with mild difficulties in new learning and language. Neurologic examination shortly thereafter documented a Mini-Mental State Examination (MMSE)8 score of 28/30. Over the course of the following two years, cognitive decline continued; his full scale IQ was then 88 (Verbal 77, Performance 108), and his MMSE score 13/30. Primary deficits in new learning and language were apparent in these evaluations. A diagnosis of probable AD was made, and the patient was soon placed in a nursing facility.He came to the attention of the GTC following an episode of neuroleptic malignant syndrome precipitated by therapy with haloperidol and lithium at another hospital. This episode resulted in marked and persistent exacerbation of his dementia as well as the development of aggressive behavior. During the course of his treatment, behavioral neurology consultation was obtained. Review of his history confirmed probable AD complicated by the episode of neuroleptic malignant syndrome. Examination was remarkable for slowed gait, mild upper extremity rigidity, and profound cognitive impairment. He was awake and alert, but had a paucity of spontaneous speech. With difficulty, he could count from 1 to 10. He was oriented only to person, and could not encode new information. Auditory comprehension was limited to one-step commands. He had remarkable sparing of repetition, however, and had occasional fragmentary echolalia. Executive function was severely impaired, and he showed prominent perseveration. There was no evidence of psychosis. CT scan of the brain revealed diffuse volume loss.As a consequence of this consultation, the patient's diagnosis of probable AD was supported, and he was found to have the unusual syndrome of mixed transcortical aphasia. The consequences of this aphasia and his other deficits for daily behavior were considered in formulating his treatment plan and guiding the pharmacotherapy of assaultiveness. Treatment with valproate, clonazepam, and paroxetine, combined with a behavioral management plan sensitive to the functional consequences of his unique cognitive impairment, effectively reduced his assaultiveness without producing excessive sedation or exacerbating cognitive loss. These interventions permitted him to be returned to the nursing facility from which he had been admitted.
Case 3. A 55-year-old woman was admitted with progressive personality change over the preceding year, characterized by hypersexuality, hyperreligiosity, paranoia, impulsivity, emotional instability, and cognitive impairment. In the distant past, she had briefly received treatment with an antidepressant following a divorce, but she had no significant depression in the many years that followed. Her medical history was noncontributory, as was her family history. Four years before admission, co-workers at her civil service job noticed that she was having difficulty managing increases in her workload. In the year before her admission, she developed religious delusions regarding her relationship with God, beliefs that her co-workers were involved in Satanism, and paranoia regarding their intentions toward her. She began displaying more prominent cognitive impairment, particularly in problem solving, judgment, and insight. These deficits affected her ability to perform her work and meet the demands of everyday life. She was briefly hospitalized on the general psychiatric ward at CMHIP and diagnosed with major depression with psychotic features, for which venlafaxine and haloperidol were given. After approximately one month of treatment, her psychotic symptoms and emotional instability had marginally improved, but her cognition and daily functioning remained markedly impaired. She was subsequently transferred to a nursing facility for continued treatment and functional rehabilitation, where she continued to decline cognitively. When her hyperreligiosity and paranoia recurred, and she also developed severe hypersexuality, she was transferred to the GTC for further evaluation.Her readmission prompted reconsideration of the diagnosis, and behavioral neurology consultation was requested. On examination, she was alert but restless and distractible. Disinhibition was the salient feature of her presentation. She was hypersexual and repeatedly attempted to remove her blouse in front of the examiner while saying “I love you.” She made many inappropriate, sexually explicit statements. She was also preoccupied with religious themes and paranoia. Her speech was normal, and there was no aphasia. She was oriented to person and recalled recent events, but so intense was her sexual preoccupation that additional cognitive examination was not possible. Her elemental neurologic examination was normal except for bilateral and strongly positive grasp reflexes.Although late-onset schizophrenia, psychotic mood disorder, and medication effects were considered, her age at onset, prominent cognitive impairments, progressive course, and neuropsychiatric features suggested a dementing disease, most likely a frontotemporal dementia (Pick's disease). Reversible causes of dementia were excluded by use of standard laboratory studies, and an electroencephalogram (EEG) was normal. CT scan of the brain demonstrated marked bifrontal and anterior temporal atrophy. A diagnosis of Pick's disease was made.Treatment with quetiapine, clonazepam, and gabapentin was combined with environmental management for her disinhibition, and this strategy was sufficiently successful to permit her transfer to the dementia unit of a local nursing facility. This case then became a frequent topic for education of GTC and other CMHIP staff on frontotemporal dementia; these efforts resulted in the improved recognition, diagnosis, and treatment of many similar patients over the following years.
Case 4. A 61-year-old left-handed man was admitted with slowly escalating disruptive behavior. The admission was precipitated by excessive outbursts of anger, but he had been experiencing confusion, memory loss, and inappropriate behavior for 6 years. A Mexican citizen who spoke no English and had received no formal education, he was an illegal alien who had worked as a migrant farm worker. His past medical history was unremarkable, and he was taking no medications. He had never been exposed to neuroleptic drugs. Family history was negative, according to his relatives.The examination was conducted in Spanish by an interpreter. The patient was alert but distractible, and was oriented to his name but not the date or locale. His speech was fluent, but he had rambling logorrhea and could follow only one-step commands. He also had a marked tendency to perseverate. He scored 9/30 on the MMSE given by an interpreter in Spanish. His affect was appropriate and he did not show evidence of psychosis. The elemental neurologic examination was notable for chorea of the limbs and trunk that interfered with voluntary movements and gait.A CT scan of the brain, interpreted by the behavioral neurologist, showed bilateral atrophy of the caudate head. Laboratory evaluation was otherwise unremarkable. On the basis of the clinical picture and the CT scan findings, a presumptive diagnosis of Huntington's disease (HD) was made. Genetic testing subsequently found an abnormally expanded allele (42 CAG repeats), and the diagnosis of HD was confirmed.The patient was treated with haloperidol and valproate. His chorea diminished, and after adjustment of the haloperidol dose to minimize the associated parkinsonism, he remained stable with only mild chorea. His behavior improved with valproate, but he did not recover sufficiently to be able to leave the hospital. In addition, his status as an illegal alien complicated his disposition. Eventually he was declared incompetent because of his dementia, and thus he could not be deported under the authority of the Immigration and Naturalization Service. He has therefore remained at the GTC for the past eight years. Risperidone has afforded acceptable control of chorea, although his dementia has advanced to a more severe state. Genetic counseling was provided to his family.
Case 5. A 76-year-old right-handed man was admitted for evaluation of recurrent episodes of confusion in the context of progressive cognitive impairment lasting two years. The patient had long-standing hypertension, treated vitamin B12 deficiency, prostate cancer in remission, chronic back pain, possible narcotic and alcohol abuse, and peptic ulcer disease. The most recent event occurred one month before admission, when the patient had an acute confusional state requiring admission to a local hospital. Although consideration was given to the possibility of a narcotic-induced delirium from drugs prescribed for his back pain, he was ultimately given a provisional diagnosis of AD with behavioral disturbances and transferred to a nursing facility for further care. At the nursing facility he was intermittently agitated and assaultive, and he required admission to the GTC for evaluation and treatment.On initial examination, affective lability, agitation, and significant cognitive impairment were evident. The confusional episodes over the preceding two years were regarded as not adequately explained by the patient's medical conditions or treatments, and a behavioral neurology consultation was requested. No other medical problems were revealed, although family history was positive for cerebrovascular disease and coronary artery disease. It was noted that his cognitive abilities did not fully recover between confusional episodes, resulting in a “stepwise” cognitive decline. His depression, affective lability, agitation, and assaultiveness also appeared to have developed in the setting of these episodes. The patient's elemental neurologic examination revealed a left homonymous hemianopia and a slow and shuffling gait with diminished arm swing. His mental status examination revealed an MMSE score of 17/29, with deficits in orientation, new learning, and visuospatial function. Further testing disclosed dramatic left neglect on clock drawing. Although his mood was neutral, the patient was affectively labile and had frequent tearful spells.Laboratory investigation for reversible causes of dementia was unrevealing. MRI demonstrated multiple areas of encephalomalacia in both frontal lobes, the right parieto-occipital region, and the left occipital lobe, all of which likely indicated previous infarction. Of these, only the right frontal lobe lesion was interpreted as relatively recent. Also noted were mild periventricular white matter disease and mild diffuse atrophy. An EEG showed no epileptiform activity.The clinical and neuroimaging findings were thought to support a diagnosis of vascular dementia with prominent left neglect, and AD was considered less likely. Recommendations were then made regarding stroke risk factor reduction, and because of possible aspirin allergy, ticlopidine was given. Behavioral disturbances were addressed with risperidone, and affective lability was treated with sertraline; both treatments were effective. The patient had no additional episodes of confusion. Daily care was adjusted to minimize the effects of left neglect, and this syndrome slowly improved. He could then be discharged to a nursing facility one month after his behavioral neurology consultation.
Case 6. A 57-year-old right-handed woman was admitted for treatment of an exacerbation of chronic major depression. She had a history of an extensive left frontal infarct approximately nine years prior to admission, resulting in right hemiplegia, nonfluent aphasia, simple partial motor seizures, and depression. Subsequent to her stroke, neurologic evaluation revealed multiple cerebral aneurysms for which she underwent four separate aneurysm-clipping surgeries and ventriculoperitoneal shunting for treatment of obstructive hydrocephalus. As a consequence of these problems, she resided in a nursing care facility for several years prior to admission. In the several months preceding admission, her seizure frequency ranged from three to six per week, she became noncompliant with her antidepressant regimen, and she ultimately became unmanageable because of increasingly severe major depression.On her admission to the GTC, a comprehensive neuropsychiatric and neurobehavioral evaluation was undertaken. Although the patient had experienced an episode of major depression three years before her stroke, that episode had fully resolved. Her medical and family histories were otherwise noncontributory. On examination, right lower facial droop, right spastic hemiplegia, hemiplegic gait, and right-sided hyperreflexia were noted. Mental status examination showed her to be alert and attentive, but with dense nonfluent aphasia. She understood two-step commands, but severe apraxia limited her ability to participate fully in additional cognitive testing. Her mood was depressed, and she endorsed hopelessness, helplessness, and suicidality.The persistence and refractory nature of her poststroke depression suggested that the stroke had at least exacerbated her subsequent mood disturbance. Her simple partial motor seizures also appeared to be consequent to the stroke. Following unsuccessful initial treatment of depression with nortriptyline and nefazodone, paroxetine was effective. Concurrently, seizure control was achieved with a combination of phenytoin and gabapentin. Because the patient had not been engaged in physical therapy or speech therapy subsequent to her stroke or multiple surgeries, both were undertaken during her hospitalization. The patient's mobility improved so much that she was no longer wheelchair-bound, and she learned to use a special communicator to compensate for her nonfluency. After five months in the hospital, she was sufficiently improved to permit discharge to a skilled nursing facility for further care.
Case 7. A 48-year-old right-handed woman was admitted from a nursing home for evaluation and treatment of one week of irritable mood, affective lability, aggression, assaultiveness, impulsivity, suicidal ideation, decreased sleep, and paranoia. The patient had experienced idiopathic encephalitis approximately 15 years before admission that produced massive injury to the right hemisphere and left frontal lobe and led to left hemiplegia, complex partial seizures with secondary generalization, and a variety of ill-defined psychiatric disturbances. She had thus required skilled nursing care and had been residing in a nursing facility immediately prior to her admission. The neuropsychiatric disturbances prompting her admission appeared after a secondarily generalized seizure approximately one week earlier. This seizure was apparently the result of a reduction in carbamazepine dose prompted by observation of a marginally elevated serum carbamazepine level. Her past medical and family history were otherwise noncontributory.On admission, her behavior was so dangerous that seclusion and restraints were required for nine days despite vigorous treatment with haloperidol and lorazepam. With repeated administration of these medications, and the addition of valproate, her aggressive and dangerous behaviors diminished. When she could be tested, laboratory workup was unremarkable. However, MRI of the brain revealed marked encephalomalacia of nearly the entire right hemisphere with several porencephalic cysts; although diffusely distributed, the cysts were most numerous in the right temporal lobe. Moderate atrophy of the left hemisphere was noted, as was subtle left frontal encephalomalacia. Her Mattis Dementia Rating Scale9 score was 83/144, with the most profound deficits in attention, construction, and perseveration.Behavioral neurology consultation was obtained during the first month of her hospitalization. Her elemental neurologic examination was remarkable for a left homonymous hemianopia, dysarthric speech, dense spastic left hemiplegia with flexion contracture of the left upper extremity, left hemihypesthesia, and left hyperreflexia. Mental status examination was remarkable for impaired attention, visuospatial dysfunction, left hemineglect, expressive aprosodia, affective lability, witzelsucht, impulsivity, and perseveration.This evaluation suggested a relationship between poor control of the patient's seizure disorder and worsening of her neuropsychiatric syndrome, and a provisional diagnosis of postictal mania was made. Optimizing her anticonvulsant regimen with carbamazepine and valproate substantially reduced the incidence of seizures and secondary mania. Continued treatment with haloperidol was also required to reduce impulsivity and aggression that persisted despite improvement in her secondary mood disorder. By understanding the relationship between her right hemispheric lesions and the various cognitive and behavioral effects of this damage, the GTC staff were able to construct a behavioral management plan that promoted a balanced approach between tolerance of and interventions for her “frontal” behaviors. This plan was communicated successfully to her usual nursing facility, to which she was discharged after a five-month hospitalization.
Case 8. A 75-year-old right-handed retired Air Force officer was hospitalized on the GTC after five years of progressive neuropsychiatric deterioration that had not been securely diagnosed. Initial symptoms included impaired memory, poor concentration, and irritability. Soon thereafter, he began experiencing visual hallucinations, paranoia, episodic disorientation, facial masking, cogwheel rigidity, a shuffling gait, and myoclonic seizures. His past medical history and family history were noncontributory.On examination, the patient was an ill-appearing, anxious man who was only intermittently cooperative. He was alert but inattentive, distractible, and oriented only to person. Although he was able to register three items, he was unable to recall any of them after a five-minute delay. Remote memory was somewhat better preserved. Speech was hypophonic and palilalic, and although his writing was micrographic and his reading was poor, other language functions were relatively intact. Visuospatial impairment was evident on drawing. His calculations were poor, and responses to proverbs were nonsensical. Impulsivity and perseveration pervaded all aspects of the examination. He had a coarse resting tremor of the hands, diffuse rigidity, and occasional asynchronous myoclonic jerks of the extremities.Laboratory evaluation for reversible causes of dementia was unrevealing, and lumbar puncture and a CT scan of the brain with contrast were normal. MRI revealed two small periventricular white matter lesions on T2-weighted sequences. EEG demonstrated frontal intermittent rhythmic slow activity, and when myoclonus occurred, a burst suppression pattern was observed. Treatment with phenytoin, carbamazepine, desipramine, haloperidol, chlorpromazine, and thiothixene was ineffective. A diagnosis of Creutzfeldt-Jakob disease (CJD) was then considered. Biopsy of the right frontal lobe was performed to clarify the diagnosis; the result was indeterminate, but spongiform changes were not seen.The patient died after seven years of the illness, and as a result of the collaboration between the GTC and UCHSC, postmortem examination was obtained. The autopsy demonstrated classic Lewy bodies in the substantia nigra and other subcortical regions, and Lewy-like bodies in the neocortex; neuritic plaques and neurofibrillary tangles were rare and spongiform changes were absent. A diagnosis of diffuse Lewy body disease was made.10This case, an example of what is now called dementia with Lewy bodies (DLB),11 was one of the first such to be recognized in this country.10 Since that time, DLB has become an important entry on the list of degenerative dementias. At the GTC, the case provided an opportunity for many continuing education efforts concerning CJD, DLB, and related dementias of late life.
DISCUSSION
ACKNOWLEDGMENTS
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).