Neuropsychiatric disturbances are a major feature of a variety of dementing illnesses, including Alzheimer's disease (AD), vascular dementia (VaD), and frontotemporal dementia (FTD). Behavioral abnormalities may contribute significantly to decreased quality of life, increased morbidity, higher levels of caregiver distress, and the decision to institutionalize a patient.
1–3 In the few studies devoted to this topic, anxiety is identified as an important behavioral symptom in AD and other forms of dementia, and it may be a prominent feature early in the course of the disease.
4 In studies commenting on anxiety in AD patients, the cross-sectional relevance varies from 25% to 75%.
5–10 However, anxiety in dementia has not undergone much study, and the literature offers little information about its features and any associations it might have with other patient characteristics and behavioral changes. It also has been difficult to assess anxiety separately from common comorbid behaviors such as depression, agitation, and irritability. Anecdotal evidence suggests associations between anxiety and agitation, irritability, pacing, and depression; it is not known whether such associations are specific to AD or are present in other forms of dementia as well. In one study of patients with AD, the presence of a generalized anxiety disorder (GAD) was associated with greater levels of depression, tearfulness, irritability, overt aggression, and mania.
11RESULTS
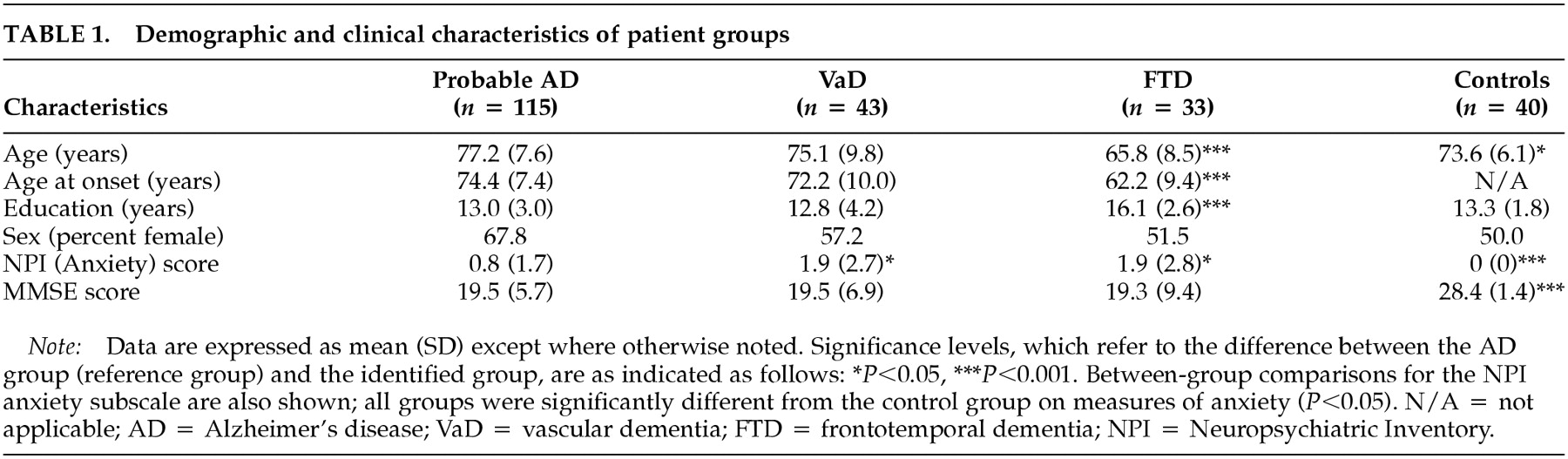
Study population. Table 1 summarizes the characteristics of the study populations. The mean ± SD age of the control subjects (73.6 ± 6.1) was lower than that of patients with AD (77.2 ± 7.6;
P<0.05) and higher than that of patients with FTD (65.8 ± 8.5; (
P<0.001). The mean age of patients with FTD (65.8 ± 8.5) was lower than that of patients with AD (77.2 ± 7.6;
P<0.001) or VaD (75.1 ± 9.8;
P<0.001). These results are consistent with the earlier age at onset of FTD (under age 65).
20 Of the patients with AD, 65.2% were white, non-Hispanic, 17.4% were black, non-Hispanic, 4.3% were Asian or Pacific Islander, and 13.1% were classified as other. In the VaD group, 74.4% were white, non-Hispanic, 18.6% were black, non-Hispanic, 2.3% were Asian or Pacific Islander, and 4.7% were other. In the FTD group, 84.8% were white, non-Hispanic, 9.0% were white, Hispanic, and 6% were other. All control subjects were white, non-Hispanic.
The mean MMSE score of the control group was higher than that of the dementia groups (AD, VaD, FTD; P<0.001); there were no significant differences among patient groups.
The FTD group differed from all others in total years of education; the FTD group was more highly educated (16.1 ± 2.6; P<0.001).
Frequency and Characteristics of Anxiety. Anxiety was reported less frequently in patients with AD than in those with VaD or FTD. Caregivers reported the presence of anxiety in 30 patients with probable AD (26.1%), 22 patients with VaD (51.2%), and 18 patients with FTD (54.5%). A significant difference between groups was noted (Pearson chi-square, χ2=36.4, P<0.001). Comparisons between groups demonstrated a significant difference in the presence of anxiety between the AD and VaD groups (Yates corrected chi-square, χ2 = 7.8, P<0.01) and between the AD and FTD groups (χ2 = 80.01).
The mean anxiety score of the AD group (0.8 ± 1.7) was significantly lower than that of the FTD group (1.9 ± 2.8;
P<0.05) and the VaD group (1.9 ± 2.7;
P<0.05) (see
Table 1). All dementia groups had significantly higher scores than the control group (
P<0.01). No significant differences were observed between the VaD and FTD groups. These comparisons remained statistically significant when analyses were adjusted for the covariates of age, age at onset of the disorder, educational level, and MMSE score.
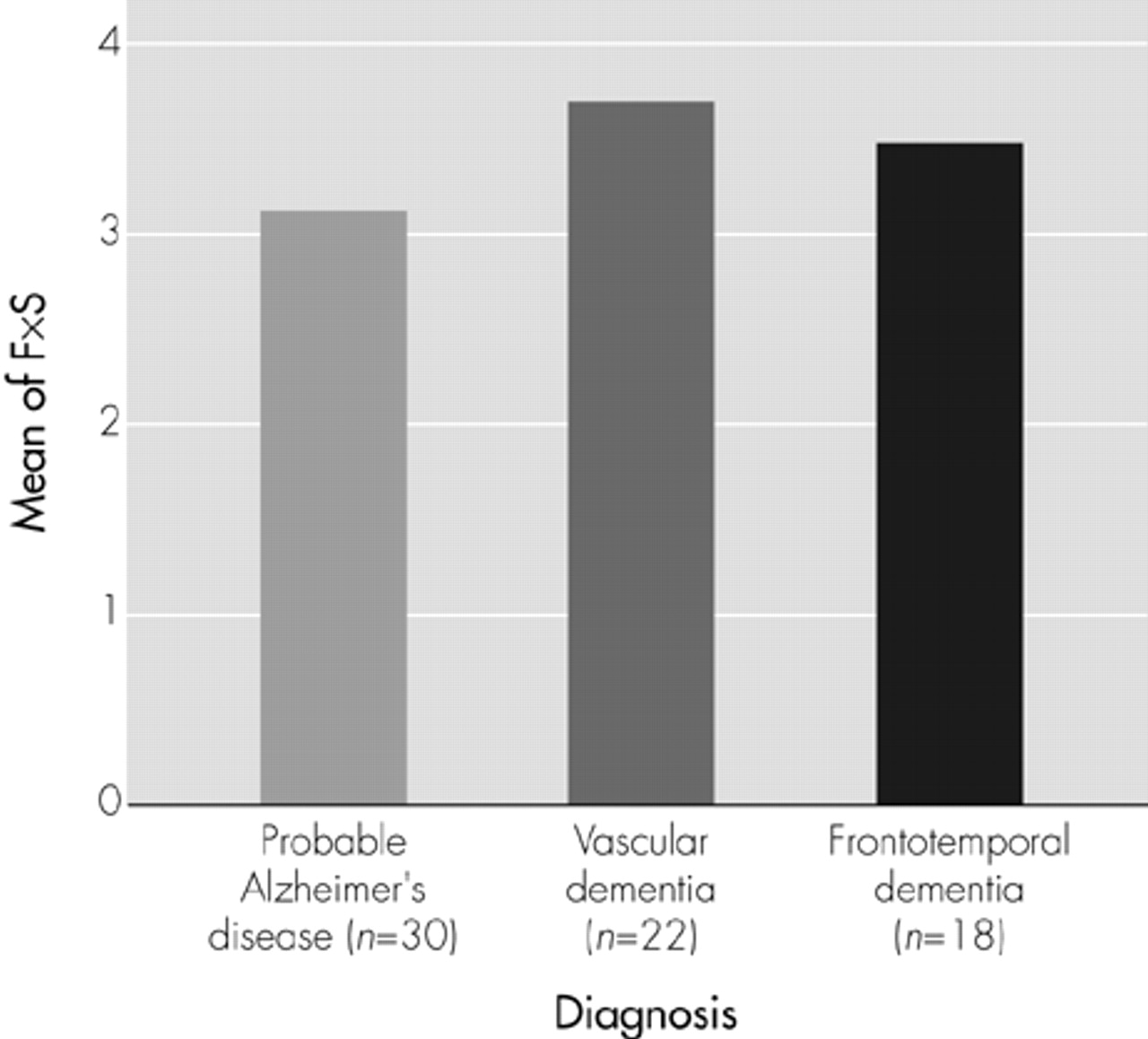
When we performed a subgroup analysis including only patients in whom anxiety was present (
Figure 1), no significant differences in anxiety scores between groups were observed. Thus, the between-group differences delineated in
Table 1 are due to differences in the prevalence of the report of anxiety among the various forms of dementia, not to differences in the level of anxiety reported in symptomatic patients in each group.
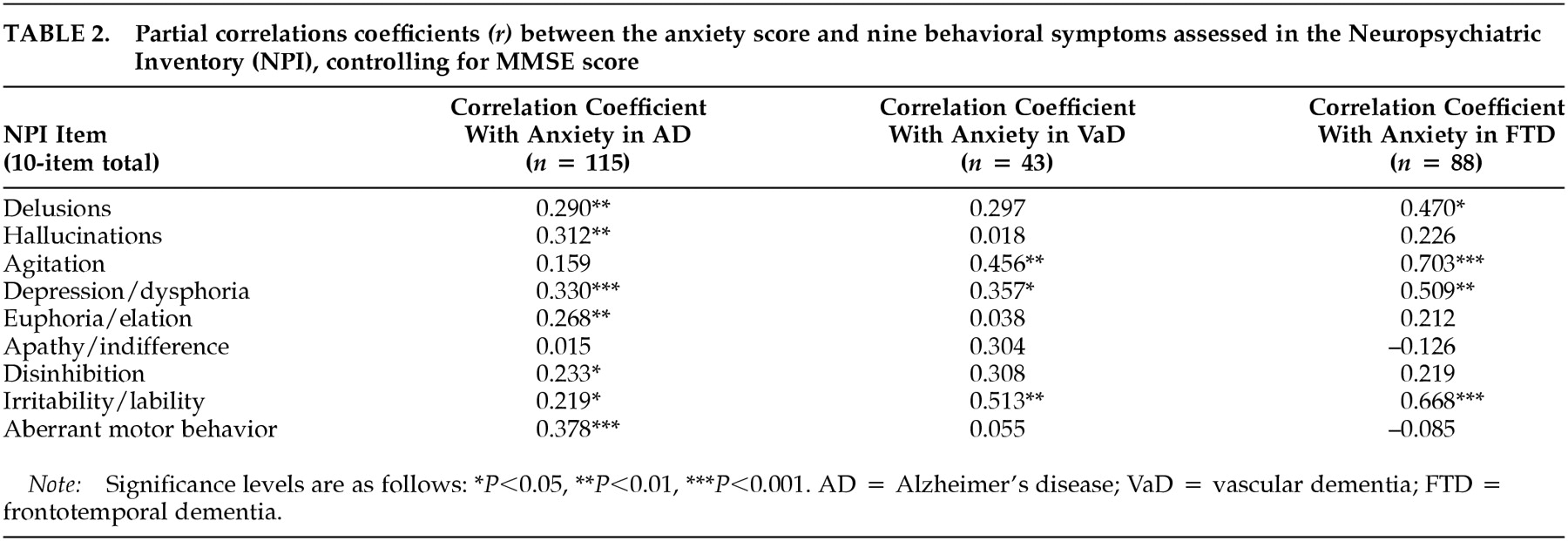
Association Between Other Comorbid Behavioral Traits and Anxiety. We calculated correlation coefficients between anxiety scores and other comorbid behavioral symptoms for the various groups.
Table 2 shows partial correlations, controlling for MMSE score, between the anxiety score and each of the other behavioral traits for the three dementia groups. When associations were examined across all dementia groups, positive correlations were noted between anxiety and depression and between anxiety and irritability. Among patients with AD, anxiety also was associated with delusions, hallucinations, euphoria, disinhibition, and aberrant motor behavior. The association between anxiety and other behavioral features was more apparent among patients with AD than among those with FTD or VaD.
The association between anxiety and depression may be explained in part by the presence of an anxious depression in some patients, given that 19 of 30 (63.3%) AD patients with anxiety also had depression. In patients with FTD, 15 of 18 (83.3%) with anxiety had both anxiety and depression. In patients with VaD, 18 of 22 (81.8%) with anxiety had both anxiety and depression.
The presence of anxiety symptoms is not equivalent to establishing a diagnosis of anxiety disorder. Only one of 115 subjects with AD in this study had anxiety as the predominant major neuropsychiatric symptom and would meet DSM-IV criteria for anxiety disorder due to a general medical condition (namely, AD). However, 30% of the AD patients with anxiety had subscale scores of 4 or greater, which is generally considered to be clinically significant. Among patients with FTD and VaD, 38.9% and 45.5%, respectively, had anxiety scores of 4 or greater.
Disease Severity and Anxiety in AD. When MMSE scores for the AD group were divided into terciles indicating mild (24–29), moderate (15–23), and severe (<15) dementia, a one-way ANOVA revealed a significant linear relationship between severity level and anxiety score (F = 5.49, df = 1,111); patients with more severe dementia had higher anxiety scores (P<0.05). Rank correlation using Spearman's rho showed an inverse correlation between anxiety score and total MMSE score (ρ = –0.308, P<0.05), indicating that the degree of anxiety increases as mental status deteriorates with advancing disease.
Gender and Anxiety in AD. No significant differences in anxiety scores were observed between men and women with AD.
Ethnicity and Anxiety in AD. A one-way ANOVA showed no significant differences in anxiety scores among the different ethnic groups (P = 0.52). Given the small number of ethnic minority patients in the sample, however, the statistical power of this negative conclusion is limited.
Age at Onset and Anxiety in AD. In order to determine whether the age at onset of the disease influenced caregivers' reports of anxiety among patients with AD, subjects were divided into those whose onset occurred before age 65 or at age 65 or older. The mean anxiety score was higher for the group with the earlier onset (2.1 ± 3.1) than for the group with a later onset (0.7 ± 1.6). An ANOVA was performed on the group means, and a corrected model was applied to adjust for the covariates of the patient's current age and the total number of years since the onset of the disease. A statistically significant difference between the earlier and later onset categories was observed after application of the model (P<0.01; R2 = 0.1, adjusted R2 = 0.07). Thus, patients with a younger age at onset of AD had a higher level of anxiety. There was no significant correlation between age at evaluation and anxiety score (Spearman's rho correlation coefficient = 0.065, P = 0.49).
Instrumental Activities and Anxiety in AD. The FAQ scale assesses independence in instrumental activities of daily living.
15 The relationship between FAQ score and anxiety score for patients with AD was examined. Partial correlation coefficients corrected for MMSE score were obtained between the anxiety score and the FAQ score. Significant partial correlation coefficients were obtained for the anxiety score (
r = 0.20,
P = 0.04). Partial correlation coefficients between the FAQ score and the anxiety score, corrected for age, remained significant (
r = 0.30,
P = 0.002). These results suggest that anxiety may contribute to disability in social functioning and to decreased independence. This result is independent of the effects of age and severity of dementia.
Medication and Levels of Anxiety in AD. There were no statistically significant differences between patients with and without anxiety with respect to use of cholinesterase inhibitors (e.g., tacrine or donepezil). No difference was observed in the presence or absence of anxiety among patients with AD when the use of anxiolytic, neuroleptic, antidepressant, or other psychotropic medications was examined. Only one of the 115 patients with AD was receiving anxiolytics at the time of evaluation. Nineteen percent of patients with AD and 13.3% of AD patients with anxiety were receiving antidepressants.
DISCUSSION
In this cross-sectional analysis, we used an established neuropsychiatric instrument, the NPI, to assess caregiver-reported anxiety among patients with dementia and normal control subjects. Anxiety was more common among patients with AD, VaD, and FTD than among normal controls. Anxiety was reported less commonly for patients with AD than for those with VaD or FTD. Among patients for whom anxiety was reported, no significant differences in mean scores were found between the diagnostic groups. Anxiety was more common among AD patients in whom the onset of the disease was before age 65 than among those whose onset was at age 65 or older. Significant partial correlations, adjusted for MMSE score, were observed between anxiety and depression and irritability across all dementia groups. Clinically relevant levels of anxiety (subscale scores of 4 or greater) were noted in 30% of patients with AD, 38.9% of patients with FTD, and 45.5% of patients with VaD.
These data suggest that anxiety constitutes a significant problem for many patients with dementia. The differences in reported anxiety between the patients with AD and those with VaD and FTD were unexpected. One possible explanation relates to the putative neuroanatomic substrate of anxiety. Recent studies suggest involvement of the orbitofrontal cortex in the subjective perception of anxiety.
21 Higher levels of reported anxiety in VaD and FTD may reflect greater involvement of the frontal lobes in these conditions. Similar disease-related differences in anxiety have been reported in the few published studies that examine this question.
22–24Some behavioral changes associated with AD may be related to the cholinergic deficits in the brains of AD patients, and these neuropsychiatric abnormalities may respond to cholinergic therapy.
25 Although less is known about the effect of cholinesterase inhibitors on the neuropsychiatric symptoms of AD than about the cognitive effects, preliminary evidence suggests that these agents may reduce apathy, anxiety, hallucinations, disinhibition, and aberrant motor behavior.
26 Donepezil has been reported to decrease anxiety in patients with moderate to severe AD.
27 In this study we did not observe an association between anxiety and the use of cholinesterase inhibitors; this may have been because our data were derived from the initial patient evaluation, and only 30 of 115 patients with probable AD were using such medications at the time of assessment.
We found no associations between anxiety and the use of neuroleptics, antidepressants, or other psychotropic medications. Only one patient of the 30 patients identified as having anxiety in the AD group was receiving an anxiolytic medication at the time of evaluation. However, many physicians prescribe antidepressants for their anxiolytic properties, desiring to avoid the potential cognitive side effects of benzodiazepines. In our sample, 22 of 115 (19%) patients with AD were receiving antidepressants, although only four of the 30 (13.3%) identified as having anxiety were receiving an antidepressant. These data suggest that there may be a role for more aggressive treatment of anxiety symptoms that are distressing to the patient and caregivers.
Although this cross-sectional analysis suggests that anxiety is a frequent behavioral manifestation across different forms of dementia, several limitations of the study design should be noted. First, relative increases or decreases of anxiety from a baseline level—such as prior to the onset of dementia—may not be accurately measured by assessment of a single time point. Second, the presence of relatively few subjects in the VaD and FTD groups did not allow for subgroup analyses to discern the influence of potential covariates such as gender, ethnicity, and the association between anxiety and FAQ scores. Third, given the homogeneity of the study sample (largely white, well-educated, and upper middle class), any generalization of the findings to other populations must be made with caution. Fourth, patients with VaD have frequently been found to have both cerebrovascular disease and AD-type pathology at autopsy, and the VaD group in this study may include patients with mixed degenerative and vascular disease. Finally, the exclusion criteria for the study were based on caregivers' reports of medical conditions, which may not include all factors that could affect the presence of anxiety. This difficulty is inherent to all studies that use proxy respondents for assessment of disease states, and it is particularly relevant in studies of dementia.
In summary, anxiety is a common behavioral symptom in patients with AD, VaD, and FTD. Among patients with AD, anxiety is associated with distinctive patterns of other behavioral manifestations, and it is more severe among patients in whom the onset of the disorders occurs earlier in life. It is less common in AD than in VaD and FTD, and this may be due to anatomical variations among these disorders. Considering the low proportion of patients in our group receiving anxiolytic therapy at the initial evaluation for dementia, there may be the opportunity for more aggressive management of disabling symptoms and for continued research into the use of potentially multifaceted pharmacological agents such as cholinesterase inhibitors.