N umerous studies have firmly established the prevalence of dissociative disorders in samples of Vietnam combat veterans with posttraumatic stress disorder (PTSD).
1 –
3 Several investigators have sought to explore neurocognitive functioning in dissociative disorder subjects by examining memory, attention, and executive functioning. For example, Guralnik et al.
4 examined whether the presence of a diagnosis of depersonalization disorder was associated with deficits in attention, memory, and executive function. In comparing a group of healthy subjects to a group of dissociative subjects, Guralnik et al. found that the dissociative group performed significantly worse on measures of memory and attention but did not differ in regards to executive function, whereas both groups performed comparably on the Wisconsin Cord Sorting Test (WCST). In their investigations of other cognitive functions, some researchers have revealed relationships between autobiographical memory and dissociation. Jones et al.
5 showed that subjects diagnosed with borderline personality disorder—a diagnosis frequently associated with dissociative experiences and dissociative disorder diagnoses—recalled fewer autobiographical memories than comparison subjects, and their recall of autobiographical information correlated with their dissociative experiences but not with measures of mood.
Based on the evidence that dissociative disorders are common among veterans with chronic PTSD and that nonveteran populations with dissociative disorders differ from comparison subjects without dissociative disorders in terms of neurocognitive functions, we hypothesized that those veterans with both PTSD and comorbid dissociative disorders would exhibit a different neurocognitive profile from the neurocognitive profile of veterans without comorbid dissociative disorders. To examine this hypothesis, we began a pilot study to examine whether a veteran subject group of PTSD subjects with a comorbid dissociative disorder produced a neurocognitive profile that was significantly different from that of another group of veterans who met diagnostic criteria for PTSD but did not meet diagnostic criteria for a dissociative disorder. Based on existing literature, we hypothesized that the PTSD group with comorbid dissociative diagnoses would show more impairment in attention, verbal memory, and autobiographical memory than PTSD subjects without dissociative illness. Because of our earlier work showing strong relationships between dissociative symptoms and psychosensory symptoms,
6 we also predicted that PTSD subjects with comorbid dissociative diagnoses would have elevated psychosensory symptom scores, compared with PTSD subjects without comorbid dissociative diagnoses.
METHOD
Ten male veteran subjects who met Structured Clinical Interview for DSM-IV Dissociative Disorders-Revised (SCID-DR)
7,
8 criteria for a DSM-IV Dissociative Disorder (PTSD/D group) and 17 male veteran comparison subjects who did not meet SCID-DR criteria for a dissociative disorder (PTSD/ND group) were recruited from consecutive admissions to a referral-based Veterans Administration hospital residential psychosocial treatment program for PTSD. All subjects carried a diagnosis of PTSD prior to program entry, and the diagnoses of PTSD and comorbid psychiatric illnesses were reviewed and validated by psychiatric interview using the Clinician Administered PTSD Scale (CAPS)
9 and Structured Clinical Interview for DSM-IV (SCID).
10 Proof of military service (form DD-214) was required for study entry. Potential subjects were screened for inclusion in the study using their Dissociative Experiences Scale (DES)
11 score. In previous studies, both the DES and the SCID-DR have been shown to have good reliability and validity.
7,
11 Based on average DES scores from 328 veterans previously admitted to the same program, all veterans with scores ranging outside one standard deviation of our local average DES score (29.0 [SD=17.2]) were approached regarding the study. Each of these subjects was then interviewed using the SCID-DR. All subjects approached for the study agreed to participate, and only one was excluded based on a discrepancy between his DES score and SCID-DR diagnosis. (Although the excluded subject’s score on the DES was elevated, he did not meet SCID-DR criteria for any dissociative disorder.) All subjects in the PTSD/D group met criteria for at least one dissociative disorder; however, the majority of PTSD/D subjects met criteria for at least two dissociative disorders. Subjects in the PTSD/ND group did not meet diagnostic criteria for any dissociative disorder. Written informed consent was obtained from all subjects. Subjects with a diagnosis of bipolar disorder, schizophrenia, alcohol abuse or dependence, or substance abuse or dependence within the month prior to testing were excluded. Subjects with a history of significant neurological illness or insult, including any history of head injury with more than a 5-minute loss of consciousness, were also excluded.
A 2.5-hour test battery examined subjects’ general intelligence, attention, memory, and executive function. In order to avoid any possibility of fatigue effects, the testing battery was split and administered on two occasions, with the two testing periods not separated by more than 72 hours. An estimate of current intellectual functioning was gathered via the Wechsler Abbreviated Scale of Intelligence (WASI).
12 The WASI assesses both verbal (Vocabulary and Similarities subtests) and nonverbal (Block Design and Matrix Reasoning subtests) functioning. Executive functioning was assessed using the Wisconsin Card Sorting Test (WCST),
13 the Iowa Gambling Task,
14 and Trail Making Test (Parts A and B).
15 Measures of attention and memory included the Digit Span Distractibility Test,
16 which is comprised of distraction and nondistraction trials. In the nondistraction trials, a female voice reads a string of digits aloud. In the distraction trials, a male voice reads a series of digits during each of the intervals between digits spoken by the female voice. Following each trial, nondistraction as well as distraction, subjects are required to record the digits spoken by the female voice. Verbal learning and memory were assessed with the Hopkins Verbal Learning Test.
17 The Rey Complex Test and Recognition Trial (RCFT) was used to measure visuospatial memory.
In order to assess autobiographical memory, the Autobiographical Memory Interview (AMI)
18 —a clinician administered interview—reviewing subject memories from three significant life eras (childhood, early adulthood, recent) was administered to all subjects. The AMI produces scores based on semantic memories for specific data (such as addresses, names of friends) and memory for details of autobiographical events for each life era. In addition, all subjects completed the Iowa Interview for Partial Seizure-like Symptoms (IIPSS). The IIPSS measures psychosensory symptoms and has been shown previously to correlate with DES scores and PTSD symptoms in this population.
6RESULTS
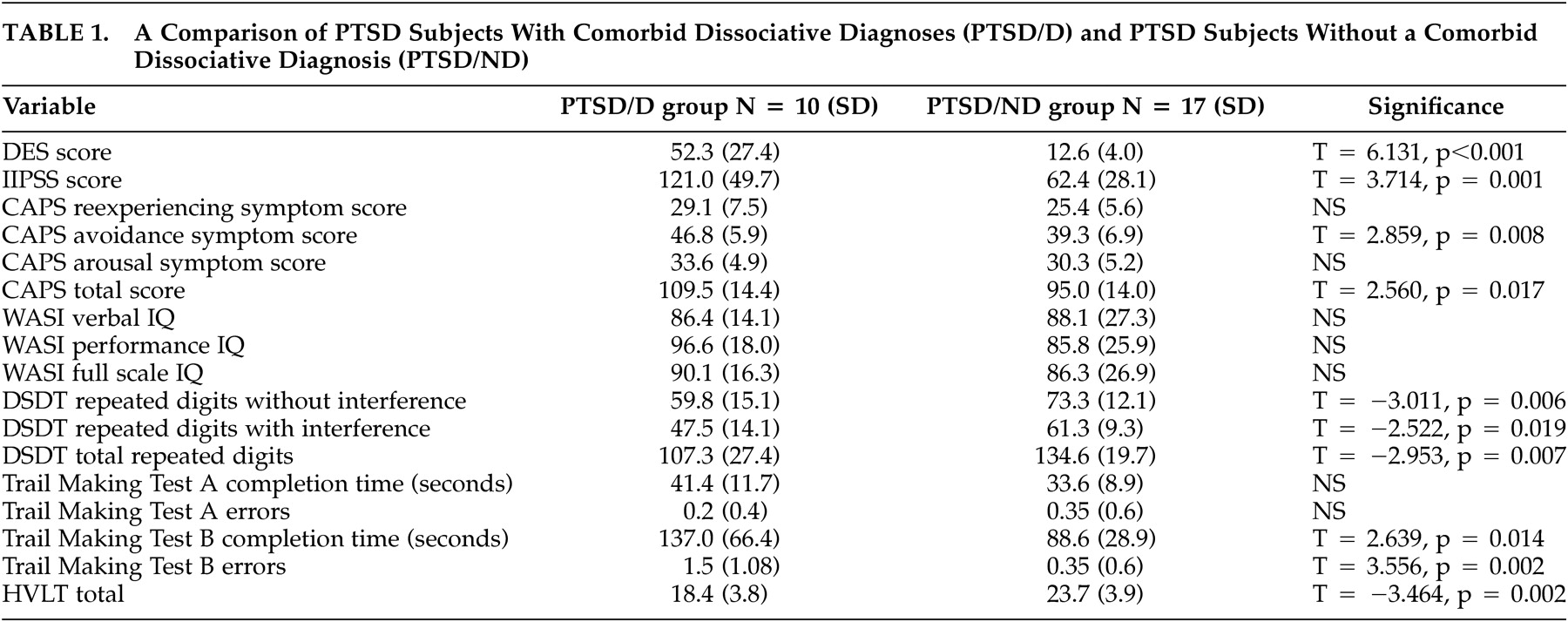
In our study, descriptive statistics and cognitive functioning for both the PTSD/ND group and the PTSD/D group are reported in
Table 1 . No significant differences were found between groups regarding age (PTSD/D=48.0 [SD=3.2] years, PTSD/ND=52.2 [SD=3.7] years; t=−1.929), educational attainment (PTSD/D=12.8 [SD=4.4] years, PTSD/ND=13.6 [SD=2.8] years; t=−0.417), or prevalence of major depression, alcohol or substance use disorders, or panic disorder. No statistically significant differences (by Chi-square) were found between the PTSD/D and PTSD/ND groups in terms of neuroleptic use (PTSD/D=2/10 with neuroleptic use, PTSD/ND=2/17 with neuroleptic use), antidepressant use (PTSD/D=9/10 with antidepressant use, PTSD/ND=15/17 with antidepressant use), benzodiazepine use (PTSD/D=1/10 with benzodiazepine use, PTSD/ND=2/17 with benzodiazepine use), or anticonvulsant medications (PTSD/D=2/10 with anticonvulsant use, PTSD/ND=3/17 with anticonvulsant use). Only one (10%) subject in the PTSD/D group met criteria for only one dissociative disorder diagnosis; five (50%) subjects in the same group met criteria for two dissociative disorder diagnoses, and four (40%) met criteria for three or more dissociative disorder diagnoses. The most common dissociative diagnoses found in the PTSD/D group were depersonalization disorder and dissociative amnesia.
The average DES scores for the PTSD/D and PTSD/ND groups were 52.3 [SD=27.4] and 12.6 [SD=4.0], respectively. PTSD symptomatology, as measured by the CAPS total score, was significantly higher in the PTSD/D group. Of the three PTSD symptom clusters, only avoidance symptoms reached significance (
Table 1 ). DES scores were highly correlated with IIPSS scores (r=0.828, p<0.001) and total CAPS scores (r=0.745, p<0.001). Average psychosensory symptom scores on the IIPSS were significantly higher for the PTSD/D group than for the PTSD/ND group.
Scores for the WASI, Trail Making Test (A and B), Hopkins Verbal Learning Test (HVLT), and the Digit Span Distractibility Test (DSDT) are summarized in
Table 1 . The PTSD/ND group IQ scores were solidly within the low average range. The PTSD/D group’s verbal and performance IQ scores fell within the low average and average ranges, respectively. The two groups did not differ on any of the IQ subscales and did not significantly differ on either the WCST or the Iowa Gambling Task. While no differences were found in errors or completion time on the Trail Making Test Part A, the PTSD/D group produced a significantly slower score on the Trail Making Test Part B and made four times the number of errors on Trails B than the PTSD/ND group. The two groups differed significantly in performance of the DSDT, with the PTSD/D group recalling significantly fewer numbers in the distraction and nondistraction trials.
On a measure of verbal learning and memory, the HVLT, the dissociative group recalled significantly fewer total words, primarily due to poorer performances on the second and third trials. DES scores (r= −0.436, p=0.023) and IIPSS scores (r= −0.459, p=0.024) correlated negatively with HVLT recall for total words. On the HVLT recognition task, the two groups did not differ on the number of words correctly identified. However, the dissociative group produced more errors in identifying words not included in the three learning trials—that is, there was a significant difference on errors of commission. Closer inspection of data found most of this difference was attributed to the incorrect inclusion of unrelated words. In addition, the two groups did not differ on any of the RCFT scores.
PTSD/D subjects performed more poorly on AMI measures than did PTSD/ND subjects, with significantly lower scores on recent semantic memory (t=−2.47, p=0.022), overall personal semantic memory (t=−2.57, p=0.018), and autobiographical memory for young adulthood (t=-2.09, p=0.049). DES scores correlated negatively with overall personal semantic memory (r= −0.558, p=0.011) but not with overall recalled autobiographical incidents. Total CAPS scores showed no correlation with WASI, HVLT, AMI, DSDT, or Trails A or B scores.
DISCUSSION
Results of this pilot study showed that PTSD subjects with a comorbid dissociative diagnosis present with a different neurocognitive profile than veterans with chronic PTSD and without a comorbid diagnosis of a dissociative disorder. The deficits noted in those PTSD patients with dissociative disorders were in the domains of memory (new learning of verbal material, autobiographical memory), psychosensory symptoms, attention, and some frontal lobe functions (Trails B but not Trails A, WCST, or the Iowa Gambling Task). No differences were noted in either IQ or visuospatial memory.
Deficits in memory and frontal lobe type functions have been detected in some studies of patients with PTSD but not in others.
19 It is relevant that across multiple studies of the cognitive deficits of PTSD, the three domains that are typically impaired are IQ, memory, and frontal lobe functions.
20 The fact that these three domains are variably impaired in different combinations across studies suggests there may be subgroups within the PTSD population that explain the consistency of the types of cognitive deficits but the variable severity of the deficits. Since PTSD patients often meet criteria for dissociative diagnoses and the presence of a dissociative diagnosis may be associated with various neurocognitive impairments, this study lends credence to the notion that some of the cognitive deficits previously attributed to PTSD alone could be at least in part associated with other neuropsychiatric conditions, such as dissociation, in these patients. Our pilot project as well as other studies
21 suggests that careful examination of PTSD subject subpopulations can result in improved assessments of objective findings in this heterogeneous group.
Perhaps the chief limitation of this pilot study was the small number of subjects involved; given the prevalence of other disorders, such as borderline personality disorder in subjects with dissociative disorders, future studies should also include assessments for axis two disorders. More studies of larger samples of PTSD subjects are necessary.
Notwithstanding the limitations of this study, it supports the hypothesis that a subgroup of combat veterans with PTSD experiencing significant dissociative phenomena and meeting criteria for comorbid dissociative diagnoses has considerably greater deficits in attention, autobiographical memory, and verbal memory than veteran PTSD subjects without dissociative diagnoses. Elevated psychosensory symptom scores in the PTSD/D group support our earlier findings of associations between the DES and the IIPSS and suggest that further investigation of limbic dysfunction in veterans with PTSD and comorbid dissociative disorders may be warranted.