These findings may suggest that rheumatic fever activity
1 is not a necessary condition for the expression of neuropsychiatric symptoms. In acute phase rheumatic fever patients, these manifestations could be the result of an abnormal immune process related to the activity of the disease. In the nonacute phase rheumatic fever patients,
1 it cannot be excluded that acute changes might have persisted or might have triggered other psychopathological changes that increase the susceptibility to neuropsychiatric disorders. It is well established that carditis continues to evolve even in the absence of rheumatic activity and also that may worsen with reinfections.
10 It is also known that pregnant women with past Sydenham's chorea are prone to develop
chorea gravidarum, even without the recurrence of strep infections.
11 Furthermore, basal ganglia have been implicated in OCD genesis
2,
3,
4 and persistent changes in the caudate of Sydenham's chorea patients have been detected by MRI.
12 Thus, it is possible that strep infections and/or rheumatic fever may trigger obsessive-compulsive symptoms, which may persist through adulthood independently of new rheumatic fever episodes. Another possibility is that obsessive-compulsive symptoms and OCD share a common genetic vulnerability with rheumatic fever. Patients bearing susceptibility for obsessive-compulsive symptoms and OCD could have symptoms triggered by a rheumatic fever episode. Interestingly, the association between tic disorder and ADHD symptoms which was previously reported by our group in children
2 was found in our adult sample.
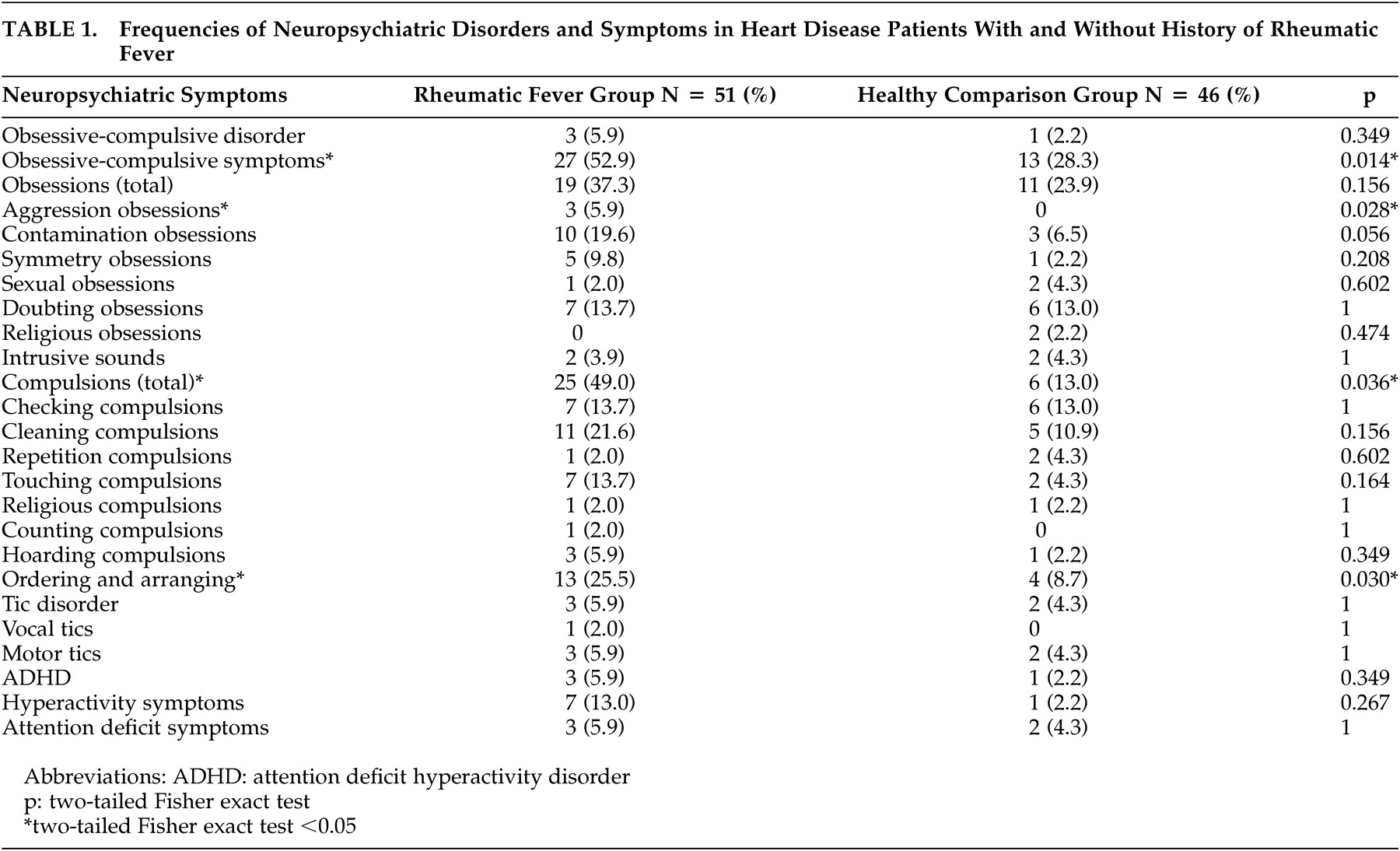
The most striking finding in the present study was the occurrence of obsessive-compulsive symptoms, mainly aggressive obsessions and ordering-arranging compulsions in a significant rate of the rheumatic fever group. These phenomenological characteristics have been reported as being part of the early onset OCD subtype and the tic-related OCD phenotype.
13 It is worth noting that according to our findings in previous studies that assessed children with streptococcal infections, men outnumbered women regarding neuropsychiatric disorders.
3 It is possible that significant obsessive-compulsive symptom rates in women with rheumatic fever would be expected in larger samples. OCD, tic disorder, and ADHD symptoms were more frequent (though not significant) in the rheumatic fever group (
Table 1 ). This may be explained by the small sample sizes.
There are some limitations to this investigation, such as the small sample sizes and the difficulty in rigorously matching groups for gender. Unfortunately, it was not possible to obtain reliable information regarding the onset of the obsessive-compulsive symptoms. Patients often did not remember the time of onset of psychiatric symptoms. The interval between the first episode of rheumatic fever and the beginning of the neuropsychiatric symptoms would bring relevant data. Although our study was not designed to assess severity of symptoms, doing so could have brought additional data. Moreover, structural brain imaging studies have not been performed. Finally, the high level of psychopathology found in the rheumatic fever group could also be secondary to the chronic heart valve disease. We hope to have controlled for these variables by using the comparison group and blind interviewers.