I ntracranial masses, especially in the presence of mass effect, edema, or increased intracranial pressure, constitute a relative contraindication for ECT.
1 However, numerous case reports and small series attest to the safe use of electroconvulsive therapy (ECT) in patients with space occupying intracranial lesions.
2 –
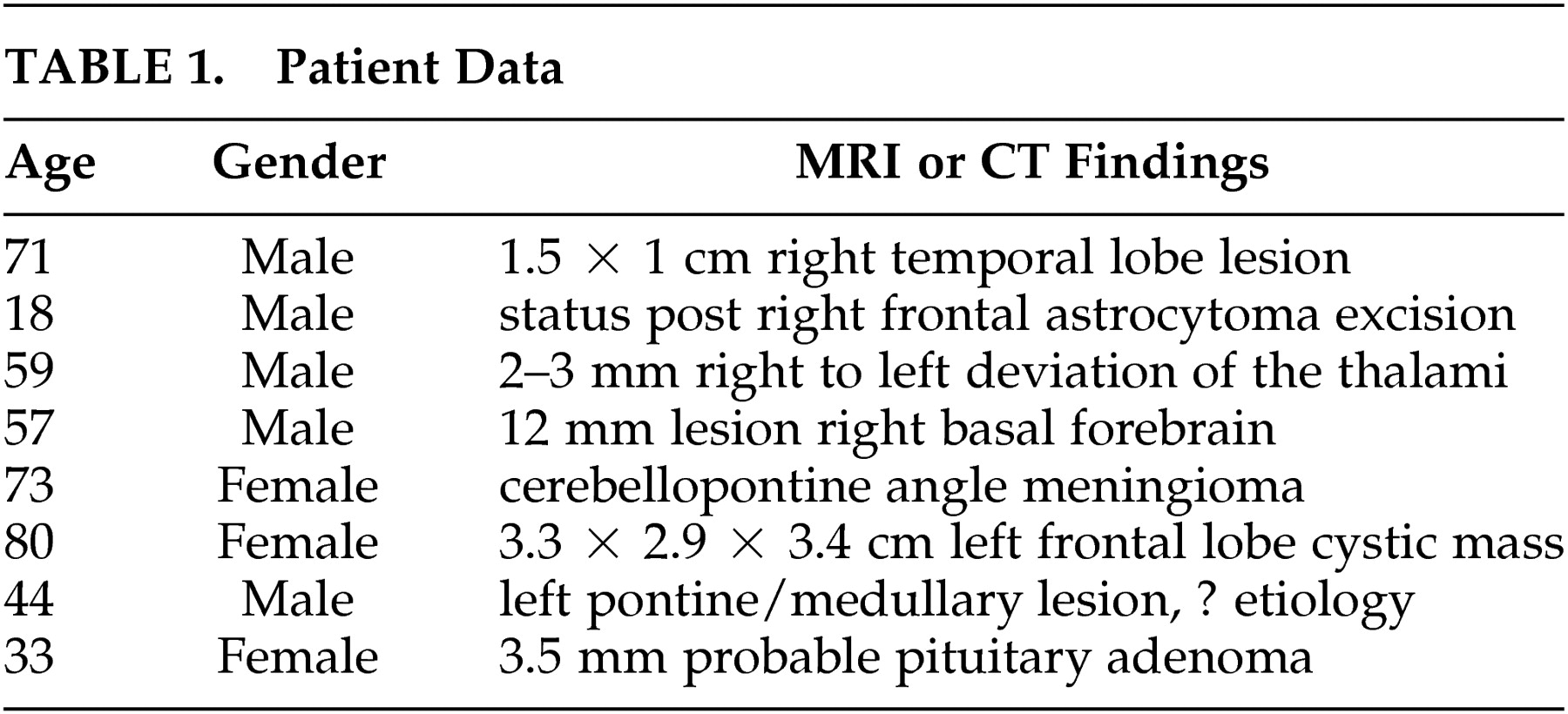
7 However, the total number of published cases is relatively small. In reviewing our ECT database, we discovered that over the past several years, we have treated seven patients with an intracranial mass (or mass effect) and one patient status post mass resection. In order to provide more clinical data on this important issue, we describe our experience herein.
All patients were treated using the Thymatron DGx or System IV ECT apparatus (Somatics, Inc., Lake Bluff, IL) utilizing bilateral electrode placement in most cases with occasional use of unilateral placement. Anesthesia technique included glycopyrrolate as antisialogogue, thiopental for induction, and succinylcholine for neuromuscular blockade. In our series, no measures were undertaken to reduce mass effect, edema, or intracranial pressure. The findings are summarized in
Table 1 .
CASE REPORTS
Patient #1
A 71-year-old psychotic man with a 3-month history of increased agitation and behavioral dyscontrol responded well to a course of ECT treatments. A pretreatment magnetic resonance imaging (MRI) scan demonstrated an approximately 1.5×1 cm lesion within the medial right temporal lobe characterized by a very subtly increased T2 signal peripherally with a central cystic component and no evidence of abnormal gadolinium enhancement. Additionally, ischemic changes in both cerebral hemispheres and mild generalized cerebral atrophy were present. A neurosurgical consultant did not feel that these findings were responsible for the patient’s current symptoms and did not require any surgical intervention; nor did the consultant feel that they should preclude him from receiving ECT. He has been receiving regular maintenance ECT treatments for approximately 1.5 years as of this writing without complications. A repeat MRI 6 months after the original showed no significant changes. No further diagnostic work-up was deemed necessary.
Patient #2
An 18-year-old man status post resection of a pleomorphic xanthoastrocytoma was hospitalized 2 years later for a major depressive episode and treated with ECT. A recent head MRI had shown a healed right frontoparietal craniotomy with postsurgical encephalomalacia involving the lateral right frontal lobe, no evidence of residual/recurrent tumor, and focal T-1/T-2 hyperintensity in the head of the right caudate nucleus that was thought to be an old hemorrhage (as opposed to postsurgical change). He underwent eight ECT treatments without clinical benefit but without neurological complications either.
Patient #3
A 59-year-old depressed man received nine ECT treatments without complications but with excellent antidepressant benefit. Noncontrast computed tomography (CT) scans obtained as part of his evaluation demonstrated a suggestion of an approximately 2 to 3 mm midline right to left shift at the level of the thalami with no discrete underlying lesion seen, which would account for that finding.
Patient #4
A 57-year-old depressed man received six ECT treatments without complications but with benefit for depression. An MRI was obtained approximately 4 weeks after ECT to look into possible neurological causes of the depression and showed a 12 mm nonenhancing lesion within the right basal forebrain parasagittally in the subcallosal region anterior to the anterior commissure with possible subtle mass effect with expansion of the involved gyrus. Single photon emission computed tomography (SPECT) scanning showed no increased isotope uptake in the area of the lesion. The impression was that the lesion was most likely benign but that a low-grade malignancy was possible. The patient is alive and healthy approximately 4 years later.
Patient #5
A 73-year-old woman received index and maintenance ECT over a 1-year interval. She was evaluated for diplopia and sixth nerve palsy, which had predated her initial ECT treatments by several years but had never been investigated. Multiple CT scans were performed in the interim, with one study having been read as showing slightly increased soft tissue on the left side of the pons anterior to the brainstem, which was thought to be a dolichoectactic basilar artery. An MRI scan was performed after approximately 1 year of maintenance ECT and showed a 1.0×1.7 cm extraaxial, durabased, homogeneously enhancing mass in the left cerebello-pontine angle cistern just anterior to the internal auditory canal. The mass abutted and slightly deformed the ventral surface of the pons. Subsequent review of previous CT scans revealed that the mass had been present on pre-ECT studies. It was diagnosed as a meningioma.
She underwent gamma knife surgery, which caused shrinkage of the meningioma without any complications. Follow-up MRI scans over the next 2 years showed no progression of the lesion. During this time, she continued to receive maintenance ECT at intervals ranging from once weekly to once monthly without any complications and with good control of her depression until her death, which was unrelated to ECT, several years later.
Patient #6
An 80-year-old woman received index and maintenance ECT over an approximately 3-year period for recurrent bouts of depression without complications. Due to some falls, a head CT scan was ordered which showed no pathology. She continued receiving treatments every other week when another fall occurred, and a CT scan, approximately 3 months after the previous one, showed a frontal mass with ring enhancement. Her family noted that she may have been sleepier with possible worsening of cognitive impairment and vivid dreams/hallucinations over the previous month.
An MRI scan showed a 3.3×2.9×3.4 cm cystic mass in the left parasagittal frontal lobe with a mild amount of surrounding nonenhancing T2 hyperintensity. It had a generally thin peripheral rim of enhancement, though it was slightly complex at its anteromedial margin on T2-weighted and postcontrast images. The radiologist felt that since there was no restricted diffusion and mild complexity along one margin, a cystic neoplasm (either primary or secondary) was the most likely consideration, although a cerebral abscess was also possible. Also noted on the study was mild enlargement of the lateral and third ventricles, which appeared mildly out of proportion to the depth of the cerebral sulci, suggesting the possible presence of mild hydrocephalus. Also, there was a moderate amount of periventricular nonenhancing T2 hyperintensity, which was possibly related to impaired transependymal flow of fluid or chronic small vessel ischemic disease.
Due to her underlying neurological disease and low probability that surgical intervention would provide significant benefit, ECT treatment was halted and she died 2 months later.
Patient #7
A depressed 44-year-old man had an MRI scan which demonstrated an indeterminate nonenhancing, ill-defined region of an abnormal T2 signal in the left medulla and pons, with some extension to the right medulla. No mass effect was present, and it was felt the lesion could represent demyelinating disease, low-grade tumor, or an artifact. Additionally, we noted nonspecific enlargement of the lateral ventricles bilaterally with particularly prominent atria suggesting mild colpocephaly, as well as mild cerebellar atrophy. He received eight ECT treatments with no complications and with good antidepressant benefit. Follow-up imaging was without significant interval change or clarification of diagnosis.
Patient #8
A 33-year-old woman was given ECT for depression. An MRI scan directed at the sella had been obtained at an outside facility as part of an endocrinology work-up and demonstrated a 3.5 mm area of lesser enhancement in the right inferior sella possibly representing a pituitary microadenoma. No deviation of the pituitary stalk or significant deformity of the diaphragma sellae was noted. She received 10 treatments without complications and with good antidepressant benefit.
DISCUSSION
Electroconvulsive treatment for the patients with known intracranial masses has been considered a high-risk undertaking. There is a general consensus in case report literature, however, that if a lesion is relatively small, solitary, and not associated with significant mass effect, edema, or increased intracranial pressure, then ECT probably does not present greater than usual risk of neurological deterioration.
1 None of the patients in our series was known to have increased intracranial pressure or edema. Mass effect, when present, was invariably quite mild. Thus, our patients probably represented low-risk candidates for ECT. Nonetheless, in the absence of a large-scale series, such patients should still be approached with caution and ongoing consultation and evaluation by a neurologist or neurosurgeon. In particular, the necessity of daily neurological evaluation cannot be overstressed, as deterioration may initially be subtle and slow. The appearance of any new-onset focal neurological finding during a course of ECT in such patients should warrant immediate neuroimaging and expert consultation. Additionally, the informed consent process should include discussion of the possible extra risk of ECT.
A more problematic scenario is the presence of one of the complicating features mentioned above. The presence of a large mass, multiple masses (e.g., metastatic lesions), edema, increased intracranial pressure, or mass effect should probably be considered relative contraindications for ECT. Only in the case of a profoundly ill patient in which the psychopathological features cause the risk of suicide, prolonged psychomotor retardation, inanition, or agitation toward others should ECT be considered, and even then only when all other options have failed. Invariably, such patients have an attending neurologist or neurosurgeon with whom to consult regarding risk-reduction strategies in preparation for ECT. We recommend that it be considered standard of care in ECT practice that if a high-risk patient as defined herein is to be treated, then measures to reduce edema and the increase in intracranial pressure be undertaken. This may include diuretic agents (e.g., mannitol or furosemide), steroid medication such as dexamethasone or methylprednisolone, or hyperventilation,
7 depending on the preference of the patient’s attending neurologist or neurosurgeon, who is likely to be familiar with the dosing of such agents and the methods to document their efficacy. As is the case with the low-risk patient, meticulous daily neurological assessments should be conducted to detect subtle changes that might become fulminant unless the treatment series is terminated. Finally, if the patient is to receive maintenance treatments, then the clinician must take into account the rate of change of the lesion. A low-risk lesion may, over time, progress to a high-risk one, necessitating either discontinuation of ECT or institution of the strategies outlined above.