S ystemic lupus erythematosus (SLE) is a chronic multisystem autoimmune disease. The importance of identifying specific syndromes in understanding systemic lupus erythematosus-related CNS pathophysiology, prognosis, and treatment is highlighted in the American College of Rheumatology’s
1 descriptions of 19 neuropsychiatric syndromes of systemic lupus erythematosus, including headache, vascular disorders, encephalopathies, and seizures.
While depression and anxiety have been reported in up to 25% of people with systemic lupus erythematosus,
2 –
4 emotional lability has only once been reported.
5 However, increased “emotionalism” has been linked with several neuropathological etiologies, including amyotrophic lateral sclerosis, multiple sclerosis, stroke, pseudobulbar palsy, and in patients recovering from temporal lobectomy for epilepsy.
6 –
10 In a neuropsychiatric service working with a systemic lupus erythematosus clinic we observed that clinically significant emotional lability was not uncommon and hence investigated the prevalence of emotional lability and symptoms of depression and anxiety in a sample of patients with systemic lupus erythematosus. We also wished to explore whether significant emotional lability, if present, was associated with increased responsiveness to external auditory stimuli, which we postulated would be a measurable electrophysiological correlate of emotional lability.
Pathological and functional consequences of systemic lupus erythematosus in the brain have been widely studied but remain poorly understood. Several studies have undertaken neurophysiological testing in patients with systemic lupus erythematosus, including visual event-related potentials, brain stem auditory event-related potentials, and electroencephalography. While these have demonstrated abnormalities in patients with systemic lupus erythematosus, correlations with clinically identifiable abnormalities of the CNS have been hard to show.
11 –
18Event-related potentials are derived from averaged EEG responses to specific stimuli and can be characterized in terms of latency and amplitude of response. Those occurring within the first 150 msec or so after stimulus onset index automatic, preattentive aspects of initial response to stimuli, while those occurring later may index specific cognitive operations related to the processing of the stimulus. The N1, peaking around 100 msec after stimulus onset in response to discrete auditory stimuli, has several components largely reflecting auditory cortex activity in the transient detection of a stimulus, facilitating later responses as an early part of an attention-switching process.
19 Mismatch negativity (MMN) is elicited when infrequent (“deviant”) sounds occur in a sequence of repetitive (“standard”) sounds. It is generated by an automatic, attention-independent neural process as part of auditory preattentive memory, usually peaking between 100 and 200 msec after deviation onset, and it is part of an automatic alerting mechanism, stimulating the individual to attend to unexpected environmental events.
20,
21 P3a and P3b are later event-related potentials associated with the process of conscious attentional shifts. P3b is generally recorded in an “oddball” paradigm in which two different stimuli are randomly presented with different probabilities while the participant is instructed to identify each occurrence of the less frequent stimulus. It is considered to reflect attentional resource allocation when working memory is engaged. P3a is recorded in response to a series of task-irrelevant, individually novel stimuli inserted into an “oddball” paradigm and is thought to reflect a frontal lobe-based process of involuntary attention orientation to an unexpected novel stimulus.
19,
22In this study we focused on a single psychiatric manifestation of systemic lupus erythematosus—emotional lability—and hypothesized that higher levels of emotional lability would be reflected in measurable changes in attentional processes, reflecting greater responsivity to changing internal or external stimuli. This hypothesis was based on reports of decreased latency and increased amplitude of electrophysiological responses to several paradigms in people with panic and anxiety disorders who showed increased environmental responsiveness
23 –
25 and similar observations in some
26 but not all studies of early perceptual processing in children with attention deficit/hyperactivity disorder who also manifest affective lability and emotional overreactivity.
27 The biological underpinning of the relationship between affective state and attentional processes is not yet clarified. However, there is evidence that experimentally induced reduction in 5HT levels following acute tryptophan depletion is associated with both the generation of transient mood change and reduced mismatch negativity latency reflecting stimulatory effects on involuntary attention switching, possibly mediated by decreases in brain 5-HT
2 receptor binding in various cortical areas, including the temporal and frontal regions.
28 This explanation is supported by reports of successful treatment of neuropsychiatric emotional lability by selective serotonin reuptake inhibitors.
29,
30In the current study we therefore predicted that increased emotional lability would be associated with increased responsiveness and faster attentional orienting to unexpected auditory stimuli.
METHOD
Participants and Clinical Measures
Thirty-two consecutive attendees (29 females, ages 19–63 years, mean age 42) at a rheumatology-led systemic lupus erythematosus clinic were recruited into the study, approved by the local research ethics committee, with informed consent obtained after study procedures had been fully explained. All participants fulfilled the 1982 American College of Rheumatologists’ research criteria for systemic lupus erythematosus. Participants completed the Hospital Anxiety and Depression Scale (HAD)
31 and the Centre for Neurological Study Lability Scale (CNS-LS), a self-report measure of affective lability.
7 Participants also underwent a clinical interview to provide information about onset, severity, and treatment of their systemic lupus erythematosus and any neuropsychiatric symptoms.
Procedures and Stimuli
Three standard auditory tasks were employed to elicit event-related potentials: mismatch negativity, novel sound P3a and oddball P3b. Mismatch negativity standard (1000 Hz) and rare (922 Hz) tones were presented in pseudorandom sequence. All had intensity of 85dB and duration of 40 msec, including 5 msec rise and fall time. Altogether, 1000 tones (880 standard and 120 rare tones) were delivered binaurally through headphones with a constant interstimulus interval (ISI) of 500 msec. Participants were instructed to read a book while the tones were presented.
The P3b paradigm consisted of a pseudorandom sequence of 210 standard (1000 Hz) and 45 target tones (1500 Hz). For the P3a, 45 unique novel sounds were added. Participants were instructed to press a button when detecting a target tone. Before the recordings, participants listened to five target and five standard tones to ensure correct differentiation between them. Tones were delivered binaurally through headphones with interstimulus interval of 1 sec, intensity of 85dB, and duration of 40 msec, including 5 msec rise and fall time.
EEG Recording
Electroencephalograms (EEGs) were recorded from Ag/AgCl electrodes placed along the midline (Fz, Cz, Pz) and fronto-laterally (F3, F4) according to the standard 10–20 electrode placement system, using Neuroscan software v.4.2 (Neuroscan Inc., Charlotte N.C., U.S.). Linked earlobe electrodes were reference electrodes. The ground electrode was halfway between Cz and the left earlobe. Electro-oculograms (EOGs) were recorded from an electrode located above and in between both eyes and an electrode 1 cm lateral to the outer canthus. All recordings were made in a sound-attenuated dimly lit room with sources of extraneous electrical noise minimized. EEGs and EOGs were amplified with a bandpass filter (0.15 Hz–100 Hz) and digitized at a sampling rate of 500 Hz. Latencies to peak and peak amplitude were measured for each event-related potential. Stimulus tones were generated and presented using the Neuroscan Stim package.
Data Editing and Analysis
Continuous EEG data were processed off-line, correcting for ocular artifacts using the ocular artifact reduction algorithm in the Neuroscan v. 4.2 software package.
32 Data were epoched from 100 msec before to 500 msec or 1000 msec after tone-onset for mismatch negativity and P3, respectively. Epochs containing data outside the amplitude range +/−70 μV were rejected, and the remaining epochs were baseline corrected using the 100 msec prestimulus period. Reponses to each stimulus type were averaged separately for each participant.
Statistical Analysis
To quantify mismatch negativity, evoked responses to frequent tones in the mismatch negativity paradigm were subtracted from responses to the rare tones. The resulting difference waveform was filtered using a zero-phase shift low-pass filter (cutoff 30 Hz, 48dB/oct). Mismatch negativity latency was evaluated within the 100 msec–200 msec time window as the time of occurrence of the peak of the difference waveform measured from stimulus onset.
P3a was defined as the largest positive peak occurring between 250 msec and 450 msec after onset of novel auditory stimuli. The largest positive peak between 300 msec and 800 msec in the averaged waveform recorded in response to target stimuli was taken as the P3b response. Amplitude was measured relative to prestimulus baseline. Latency was measured from stimulus onset to time of peak amplitude. These measures were taken after the waveforms had been filtered (zero-phase shift, cutoff 30 Hz, 48dB/oct) at Fz, Pz, Cz, F3 and F4. Amplitude and peak latencies of N1 responses to nontarget and target tones in the P3b paradigm were also measured.
One participant was excluded from analysis of mismatch negativity and P3 because the subject did not understand the instructions. A further recording was excluded from P3 analysis because of electrical interference.
Analyses aimed to investigate possible associations between emotional lability in systemic lupus erythematosus patients and event-related potential markers of attentional processes. Accordingly, participants were divided into two groups according to whether their scores on the Centre for Neurological Study Lability Scale were below the cutoff of 17, previously identified by Smith et al.
9 as a sensitive and specific measure of pathological emotional lability.
RESULTS
Clinical Findings
Thirty-two patients were studied. At the time of the study, nine patients had symptoms of active disease, while the remainder were in remission. Nine participants had a history of mood disorder and five were taking psychotropic medication. Twenty-three participants were taking steroid medication at the time of the study and 16 were taking an immunosuppressant, most commonly azathioprine.
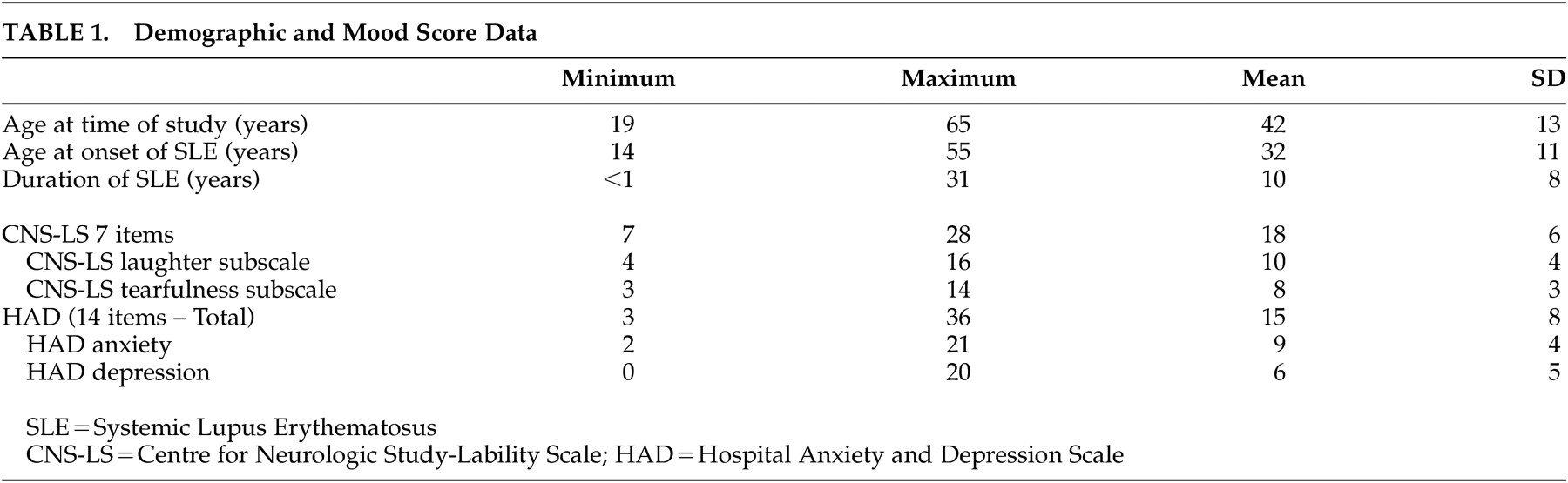
Details of the participants and their clinical rating scales are in
Table 1 . Considering Hospital Anxiety and Depression Scale scores, only six participants gained a score of less than 8, whereas five obtained a total score of between 8 and 10, indicating possible or borderline depression or anxiety, and 21 obtained a score of 11 or more, indicating probably significant depression or anxiety. Symptoms of mood disturbance, therefore, were common in this group of patients.
Using the Centre for Neurological Study Lability Scale cutoff score of 17 identified by Smith et al.,
9 15 participants obtained a score at or above this cutoff (mean 22.7), whereas 17 participants scored below it (mean 12.9). There were no significant differences in age at entry to the study or in age of onset or duration of systemic lupus erythematosus between the high and low lability groups. Of those considered on clinical grounds to have active lupus during the study, four patients were in the low lability group, whereas five were in the high lability group. There was no significant difference in numbers of those taking steroids (chi-square p=0.44) or azathioprine (chi-square p=0.29), nor any difference in mean prednisolone dose between the high and low lability groups (4.4 mg and 6.1 mg respectively) (1-way analysis of variance [ANOVA] p=0.38).
There was no significant difference between the total Hospital Anxiety and Depression Scale scores (13.5 and 16.4, respectively) nor between the Hospital Anxiety and Depression Scale depression subscale scores (6.5 and 6.1, respectively) in the low and high lability groups. However, the high lability group had higher scores than the low lability group on the Hospital Anxiety and Depression Scale anxiety subscale (10.3 and 6.9, respectively), (1-way ANOVA F=5.483, df=1, 30, p=0.026).
Event-Related Potential Findings
Event-related potential parameters were initially compared between high and low lability groups using repeated measures ANOVAs with the Greenhouse Geisser correction applied where appropriate, and significant findings were then further explored using 1-way ANOVA. To address the question of whether any observed differences were related to anxiety (which was significantly higher in the high lability group), analyses were repeated with Hospital Anxiety and Depression Scale anxiety subscale (HAD-A) score included as a covariate in the repeated measures ANOVAs.
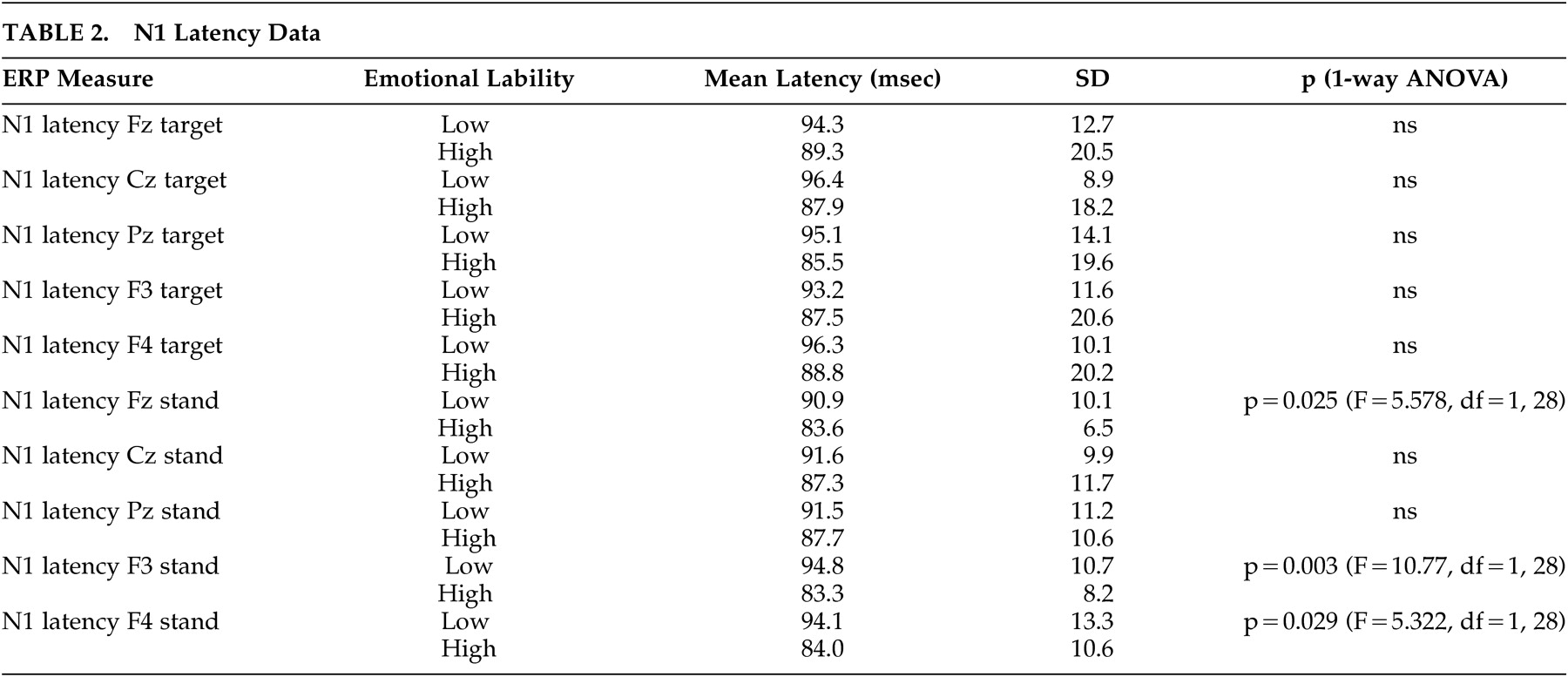
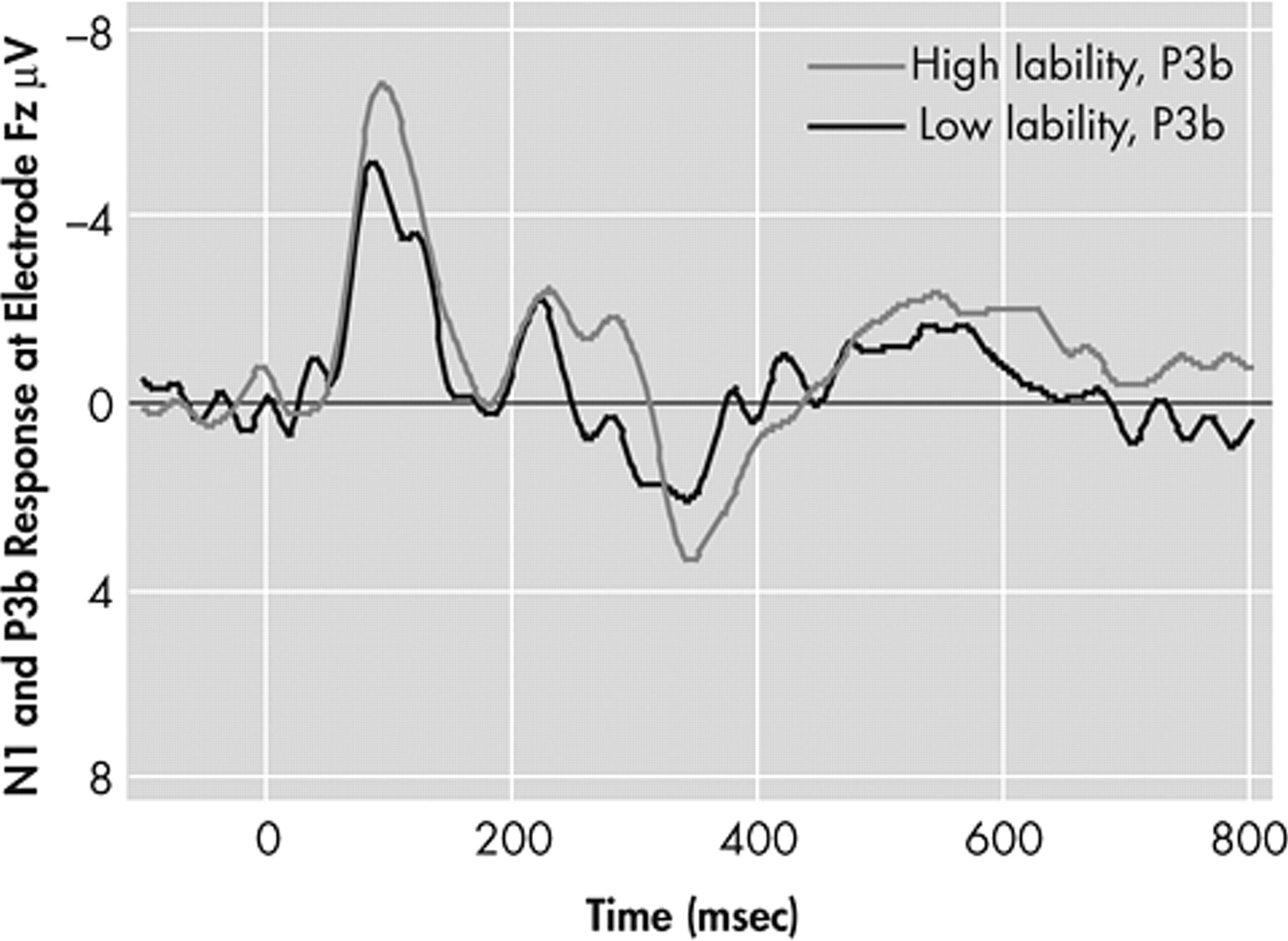
N1 Responses in the P3b Paradigm
Considering N1 latency, repeated measures ANOVA, with electrode (Fz, Cz, Pz, F3, F4) and condition (standard or target tone) as within-subject variables and membership of either high or low lability group as the between-subjects factor, revealed no significant within-subject effects. There was however a borderline-significant between-subjects effect (F=4.083, df=1, 28, p=0.053) for the high versus the low lability groups (see
Table 2 and
Figure 1 ).
Introduction of Hospital Anxiety and Depression Scale anxiety subscale score as a covariate in the repeated measures ANOVA did not change this result. Examination of the N1 latency data presented in
Table 2 demonstrates that at every electrode in response to both standard and target stimuli, N1 latencies were shorter in the high than the low lability group. Subsequent 1-way ANOVA revealed significantly shorter N1 latency to standard tones at frontal electrodes (Fz, F3 and F4) in the high compared to the low lability group. Considering N1 amplitude, repeated measures ANOVA revealed no significant group differences.
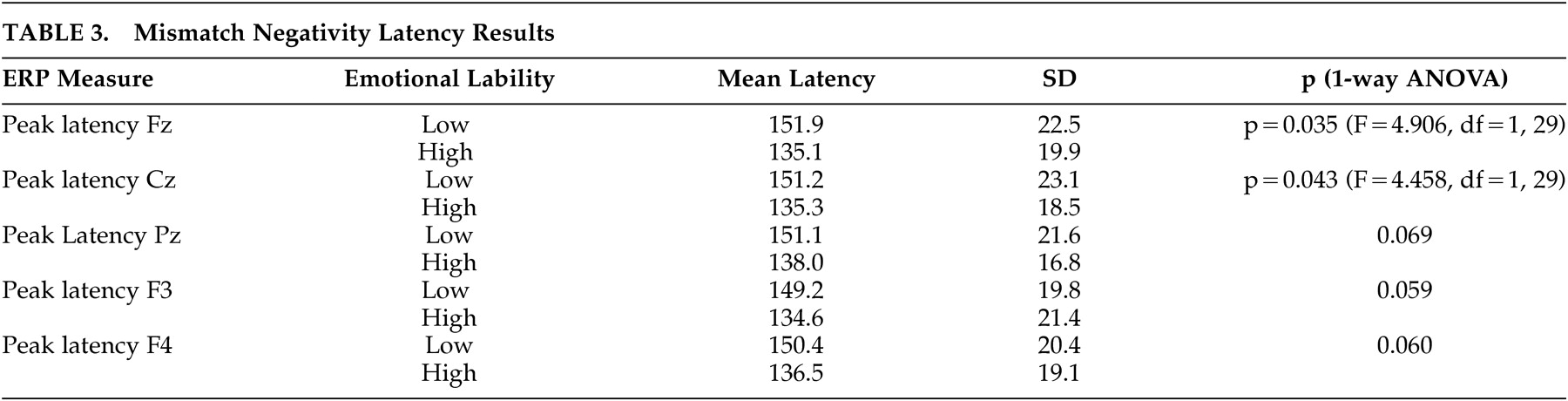
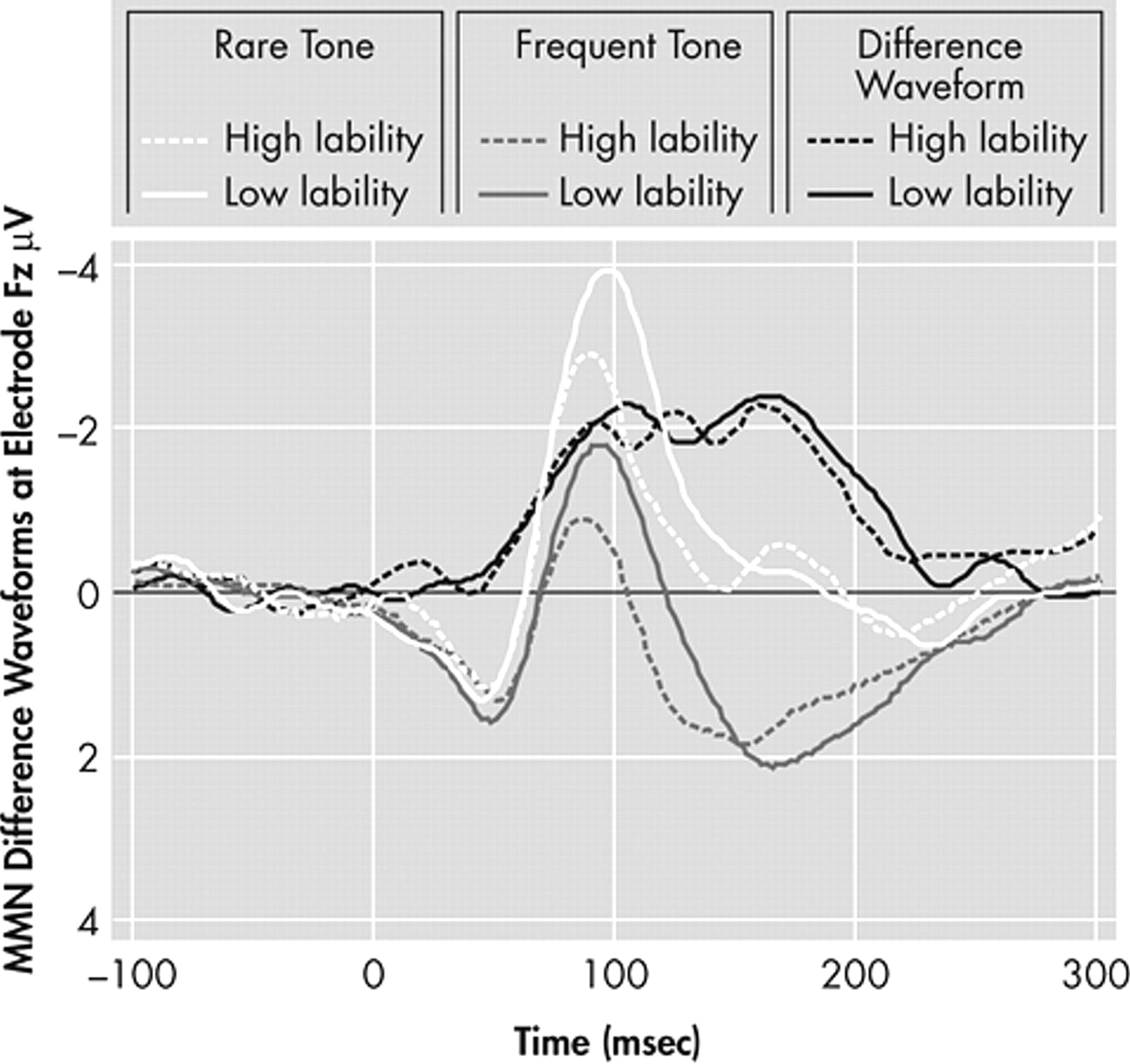
Mismatch Negativity Responses
Mismatch negativity latencies to peak response at electrodes Fz, Cz, Pz, F3 and F4 were analyzed using repeated measures ANOVA with electrode as within-group factor and membership of high or low lability group as between-groups factor. This ANOVA demonstrated no significant main effect of electrode or electrode by group interaction. However, the between groups contrast demonstrated a significant difference (F=5.004, df=1,29, p=0.033), indicating that latency was significantly different between the high and low lability groups. Introduction of Hospital Anxiety and Depression Scale anxiety subscale score as a covariate into the repeated measures ANOVA did not reduce the significance of this difference. Subsequent analysis using 1-way ANOVA demonstrated that latency to peak response was significantly earlier in the high lability group at Fz and Cz, with trends toward decreased latency at the other electrodes (see
Table 3 and
Figure 2 ). There were no differences between high and low lability groups in mismatch negativity amplitude.
P3a Results
Repeated measures ANOVA demonstrated no significant findings in analysis of P3a peak latency measures. Repeated measures ANOVA showed no significant findings in analysis of P3a peak amplitude with respect to lability.
P3b Results
Repeated measures ANOVA did not demonstrate any significant findings in the analysis of P3b peak latency measures. Repeated measures ANOVA showed a significant main effect of electrode (F=23.625, df=4, 1.853, p<0.0001). However, when Hospital Anxiety and Depression Scale anxiety subscale score was included in the repeated measures ANOVA as a covariate, this significant effect of electrode was lost.
Relationship between Event-Related Potential Parameters and Treatment and Disease Variables
While splitting the study population according to high or low lability scores revealed the group differences in event-related potential parameters reported above, no event-related potential group differences were observed when the study sample was subsequently divided according to presence (N=9) versus absence (N=22) of active lupus; treatment with (N=22) versus without (N=9) steroids; or treatment with (N=20) versus without (N=11) azathioprine.
DISCUSSION
This study arose from the clinical observation that emotional lability seemed to be relatively common in people with systemic lupus erythematosus who were referred to a neuropsychiatry clinic. We have aimed to address two questions: first, how common is significant emotional lability in people with systemic lupus erythematosus, and second, is emotional lability in this condition associated with increased sensitivity to unexpected changes in the auditory environment, measured using electrophysiological responses? Considering clinical emotional state, we observed that 47% of unselected consecutive attendees at a rheumatology-led systemic lupus erythematosus clinic obtained scores on an emotional lability rating scale that indicated clinically significant levels of emotional lability. There were no differences between those with high and low lability scores with respect to systemic lupus erythematosus-related variables, including duration of disease, presence of active disease or drug treatment, or to psychiatric variables, including past psychiatric history, psychotropic medication, or depressive symptomatology. In line with previous observations that depression and anxiety are common in people with systemic lupus erythematosus,
2 –
4 the Hospital Anxiety and Depression Scale scores of the majority of our participants indicated borderline or probably significant depression or anxiety. Our results suggest that emotional lability is found in a relatively high proportion of patients with systemic lupus erythematosus and is not associated with general indicators of overall disease severity.
Considering the event-related potential findings, we predicted that increased emotional lability would be associated with event-related potential correlates of increased responsiveness to external stimuli. This hypothesis was proved by the latency results of the earlier event-related potentials studied but not by the amplitude data or the later P3 event-related potentials. Latencies in the event-related potentials associated with preattentive auditory processing (the N1 and the mismatch negativity) distinguished between the high and the low lability groups, with shorter latencies in the high lability group. In neither the P3a paradigm, a measure of involuntary orienting of attention to an unexpected stimulus, nor the P3b paradigm, a measure of voluntary orienting of attention to a target stimulus, and in which the peak latency occurs around 50 msec later than the P3a,
33 were significant latency differences observed. While anxiety levels differed between high and low lability groups, inclusion of Hospital Anxiety and Depression Scale anxiety subscale as a covariate in the repeated measures ANOVAs demonstrated that these anxiety differences did not underlie group differences observed in N1 and mismatch negativity responses. The results suggest that higher levels of emotional lability may be associated with faster preattentive processing of changes in the auditory environment. The absence of a relationship between the observed N1 and mismatch negativity event-related potentials and anxiety scores suggests that while anxiety may be greater in those with higher levels of emotional lability, the mechanisms relating to mood change that may be modulating these preattentive event-related potentials are not the same processes that have resulted in increased anxiety scores in the higher lability group.
While there are few event-related potential studies in systemic lupus erythematosus with which to compare our findings, it is noted that the N1 latencies observed in both our high and low lability groups were a little shorter and the P3b latencies a little longer than the values observed by Khedr et al.
16 For both these event-related potentials, however, the values observed in the current study more resembled the values observed in the systemic lupus erythematosus group than in those authors’ control group. Two further studies looking at event-related potential data in systemic lupus erythematosus
34,
35 found no change in N1 latency compared to controls. However, they did not measure emotional lability or mismatch negativity.
Though previous studies have not reported associations between event-related potentials and neuropsychiatric manifestations of systemic lupus erythematosus, generally the definition of neuropsychiatric involvement has been wide-ranging.
36 In our study the specific neuropsychiatric manifestation of lability and our electrophysiological tests were precisely defined and conceptually linked based on the observation that increased emotional lability is associated with large emotional responses to relatively small triggers, which we hypothesized to be linked to changes in attentional processes.
Pathophysiological links between systemic lupus erythematosus and emotion and attention, and psychophysiological markers of these, have not been determined. While 20 different antibodies have been identified as being associated with the presence of neuropsychiatric symptoms of systemic lupus erythematosus,
37 no specific links have been determined between particular antibodies and individual neuropsychiatric symptoms. It is possible, however, that the production of neuropsychiatric symptoms may not be associated to a specific antibody but, rather, that a range of potentially brain-reactive systemic lupus erythematosus-related antibodies may lead to neuropsychiatric symptoms and that the precise nature of these symptoms will be determined by where the blood-brain barrier has been sufficiently damaged by systemic lupus erythematosus-related pathological processes to lead to it becoming permeable to these antibodies.
38Several aspects of this study mean the results should only be considered a preliminary exploration of this area. Although we looked for, and found within our participants, differences between those with higher and lower levels of lability, we did not study a comparison group without systemic lupus erythematosus so cannot contrast lability or event-related potential findings with the general population. Nevertheless, our results suggest increased emotional lability in people with systemic lupus erythematosus may be a significant clinical problem and should at least be inquired about as part of neuropsychiatric assessment. We cannot explore relationships between specific systemic lupus erythematosus symptoms and event-related potential or affective measures, as while participants met diagnostic criteria for systemic lupus erythematosus, no detailed characterization of lupus severity at the time of the study was available. The Centre for Neurological Study Lability Scale was developed to measure affective lability in amyotrophic lateral sclerosis
7 and subsequently demonstrated to be valid in patients with multiple sclerosis.
9 In their account of its use in multiple sclerosis, Smith et al.
9 noted a cutoff of 17 provided a sensitivity of 0.94 and a specificity of 0.83 with respect to clincial diagnosis of pathological emotional lability. In the current study we chose at the outset to use the cutoff established in that study.
In conclusion, within the limitations outlined above, this study demonstates that emotional lability is relatively common in people with systemic lupus erythematosus, suggesting that this psychiatric symptom should be considered in their neuropsychiatric assessment. Reliable clinical markers of CNS pathophysiology in people with systemic lupus erythematosus have been difficult to identify. Our observation that greater emotional lability was associated with shorter latency of preattentive electrophysiological responses to auditory stimuli indicates that future studies might usefully explore the relationship between this group of event-related potentials and clinical symptoms of neuropsychiatric systemic lupus erythematosus both cross-sectionally and prospectively.
Acknowledgments
The work was carried out at the Royal London Hospital, London E1 1BB, and the Section of Developmental Psychiatry at the University of Cambridge, Cambridge CB2 2AH, UK.