T he term
schizotype was introduced to identify a disorder genetically and clinically related to schizophrenia.
1 With the DSM-III, this concept was revitalized, applying a number of criteria based on the clinical profiles of probands and relatives in the adoptive studies of Kety, Rosenthal, and Wender.
2 DSM-IV diagnostic criteria for schizotypal personality disorder consist of attenuated psychotic-like symptoms such as ideas of reference and cognitive/perceptual distortions, as well as deficit-like symptoms of constricted affect, social isolation, and related criteria reflecting eccentric appearance and speech. A series of studies pertaining to the phenomenology, genetics, biology, outcome and treatment response suggested that schizotypal personality disorder is indeed closely related to chronic schizophrenia in all these domains. In particular, people with schizotypal personality disorder share similar temporal lobe volume reductions as those with chronic schizophrenia.
3 Psychiatric disorders are common in epilepsy and range from those that are a direct consequence of the epileptogenic activity to others that are simply comorbid.
4 Although evidence about a higher prevalence of psychiatric disorders in epilepsy than in the general population is still a matter of debate, an overrepresentation of psychoses seems more compelling.
5 A Danish record-linkage study found that the incidence of nonaffective psychoses was significantly increased for both men and women with epilepsy even after excluding all people diagnosed as suffering from learning disabilities or substance abuse.
6Schizophrenia-like psychoses of epilepsy seem to have distinct clinical features,
7 and a delay between the onset of seizure disorder and the psychosis has been reported.
8 However, we found no studies that specifically investigated different dimensions of schizotypy, despite the fact that it may provide further insights into the relationship between schizophrenia and epilepsy. Thus, in this study, we sought to investigate clinical correlates of schizotypal features in patients with epilepsy, with special attention to the age of onset of the seizures and a diagnosis of temporal lobe epilepsy.
METHODS
We performed a cross-sectional study of consecutive adult outpatients with epilepsy recruited from a university-based epilepsy center, the Epilepsy Clinics of the Department of Neurology at Amedeo Avogadro University in Novara.
To be enrolled, patients had to fulfill the following criteria: diagnosis of epilepsy accorded to the International League Against Epilepsy (ILAE) criteria
9 ; older than 18 years of age; absence of learning disabilities; a reading level more than 6th grade and/or a Mini-Mental State Examination (MMSE) score more than 24; willingness to provide a written informed consent to undergo the experimental procedures; and absence of severe medical diseases or a high risk of suicide. After explanation of the procedures, patients gave informed consent.
All subjects underwent a clinical interview and were assessed using the Beck Depression Inventory (BDI),
10 the State-Trait Anxiety Inventory (STAI) Y1 and Y2,
11 and the Schizotypal Personality Questionnaire (SPQ).
12 The SPQ is a 74-item self-report questionnaire modeled on DSM criteria for schizotypal personality disorder, containing subscales for the nine schizotypal traits: ideas of reference, excessive social anxiety, odd beliefs/magical thinking, unusual perceptual experiences, odd or eccentric behavior, no close friends, odd speech, constricted affect, and suspiciousness/paranoia.
12 SPQ showed good psychometric properties with a 2-month test-retest reliability of 0.82 and an internal consistency ranging between 0.90 and 0.91 for the total score and between 0.71 and 0.78 for the individual subscales.
12 Converging evidence suggests that schizotypy scores, when subjected to principal component analysis, show a three-factor structure that mirrors the three clinical syndromes found in schizophrenia: a
cognitive-perceptual factor, which includes the traits of odd beliefs/magical thinking, ideas of reference, unusual perceptual experiences, and suspiciousness/paranoia and is analogous to the clinical reality distortion syndrome; a
disorganized factor, which includes the traits of odd or eccentric behavior and odd speech and is analogous to the clinical disorganized syndrome; and an
interpersonal factor, which includes the traits of excessive social anxiety, no close friends, constricted affect, and suspiciousness/paranoia and mirrors aspects of the clinical negative syndrome.
13Correlations between patient age, age at onset of the epilepsy, SPQ total and subscales scores, BDI scores, and STAI-Y1 and Y2 scores were analyzed using the bivariate two-tailed nonparametric correlation procedures. Subsequently, a linear regression model was applied to identify relevant SPQ subscales associated with age of onset of the epilepsy.
The SPQ total and subscales scores were compared in patients with and without a diagnosis of temporal lobe epilepsy (TLE) using the Mann-Whitney test. A backward stepwise logistic regression model was applied to identify relevant SPQ dimensions correlated to diagnosis of temporal lobe epilepsy.
The Kruskal-Wallis Test was used to analyze the relationship between the SPQ total and subscales scores and EEG laterality or seizure frequency. All statistical analyses were two-sided, with a probability level set at p=0.05, and were conducted using the Statistical Package for Social Sciences (Version 12 for Windows, SPSS Inc., Chicago).
RESULTS
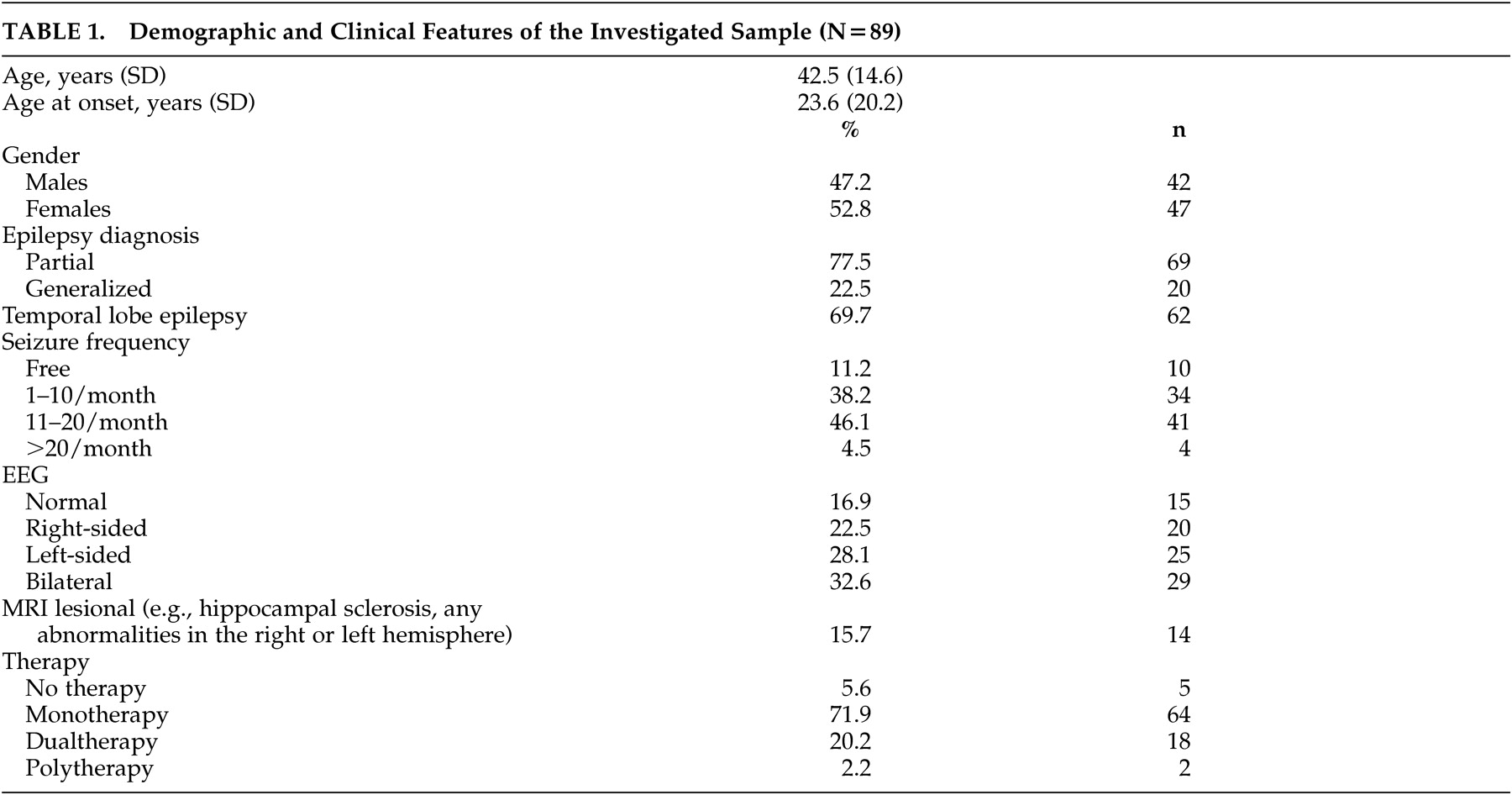
We analyzed data from 89 patients with epilepsy (42 men). Their mean age was 42.5 years (SD=14.6), age at onset of the epilepsy was 23.6 years (SD=20.2), 77.5% had a diagnosis of partial epilepsy (n=69), and 69.7% had temporal lobe epilepsy (n=62) (
Table 1 ). Almost half of the patients (49.4%) were taking carbamazepine (n=44), 19.1% valproate (n=17), 14.6% barbiturates (n=13), 11.2% lamotrigine (n=10), 10.1% oxcarbazepine (n=9), 9% topiramate (n=8), 3.4% levetiracetam (n=3), and 2.2% phenytoin (n=2). In previous psychiatric history, 21.3% had a diagnosis of mood disorders (n=19), 18% of anxiety disorders (n=16), and 3.4% of psychoses (n=3).
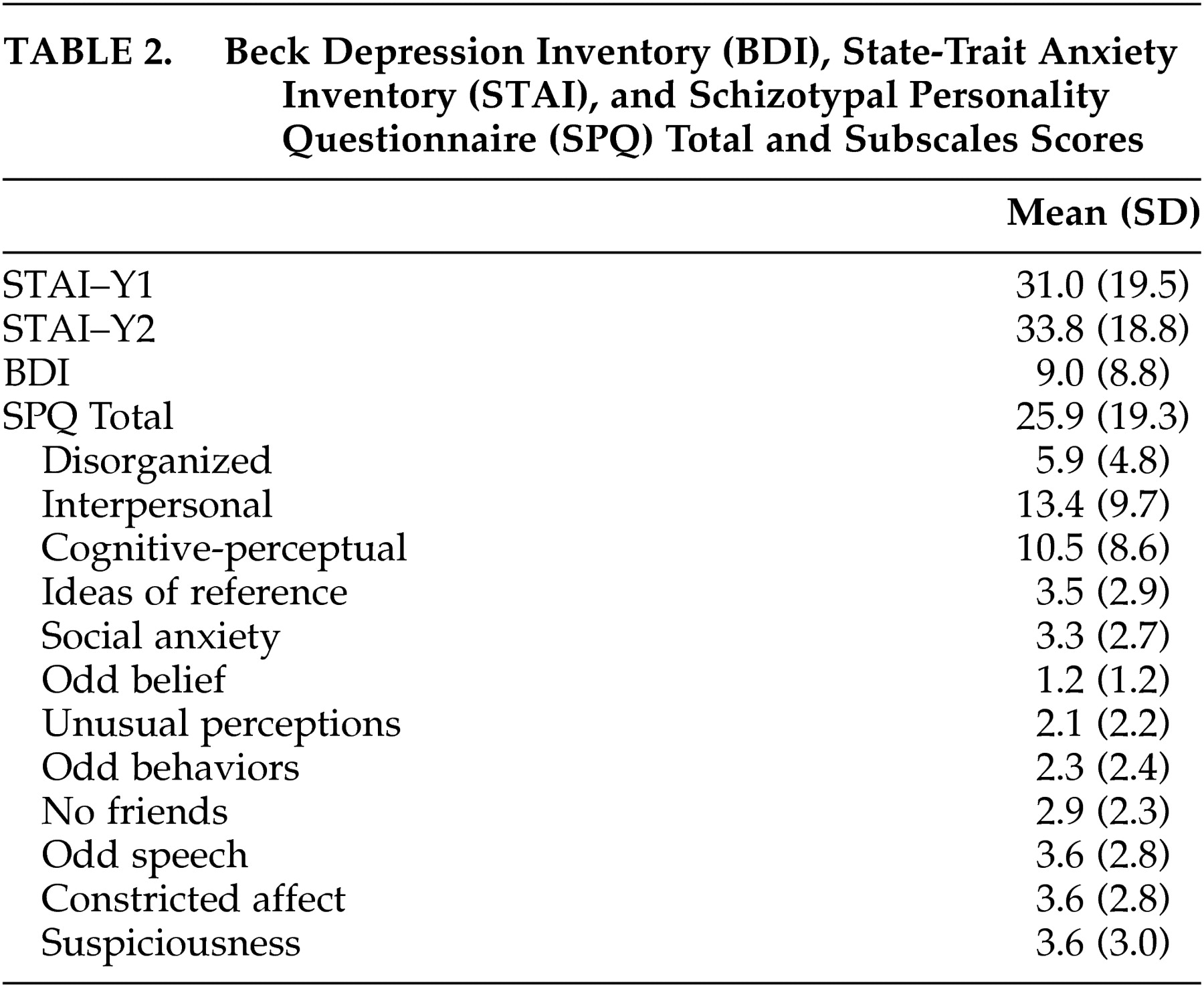
The Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI) Y1 and Y2, Schizotypal Personality Questionnaire (SPQ) totals and SPQ subscales scores are shown in
Table 2 . There was no relation between SPQ total and subscales scores and EEG laterality or seizure frequency. Age at onset of epilepsy did not correlate with BDI or STAI-Y1 and Y2, while significant correlations were found for SPQ total score (ρ=−0.247, p=0.019), disorganized (ρ=−0.214, p=0.044), interpersonal (ρ=−0.248, p=0.019), cognitive-perceptual (ρ=−0.233, p=0.028), odd belief (ρ=−0.249, p=0.019), unusual perceptions (ρ=−0.214, p=044), odd speech (ρ=−0.239, p=0.24), constricted affect (ρ=−0.421, p<0.001), and suspiciousness (ρ=−0.215, p=0.043). However, linear regression models including total SPQ score, the three factors (disorganized, interpersonal, cognitive-perceptual), and the subscales odd belief, unusual perceptions, odd speech, constricted affect, and suspiciousness showed that only constricted affect scores significantly correlated with age at onset of the epilepsy (OR=−3.04; 95% confidence interval [CI]=−5.32 to −1.48, p=0.001). Constricted affect scores showed also a significant correlation with STAI-Y1 (ρ=0.458, p<0.001), STAI-Y2 (ρ=0.364, p<0.001), and BDI scores (ρ=0.299, p=0.004). In the subgroup of patients with temporal lobe epilepsy, the correlation between age at onset of the seizures and constricted affect scores was less evident (ρ=−0.291, p=0.022).
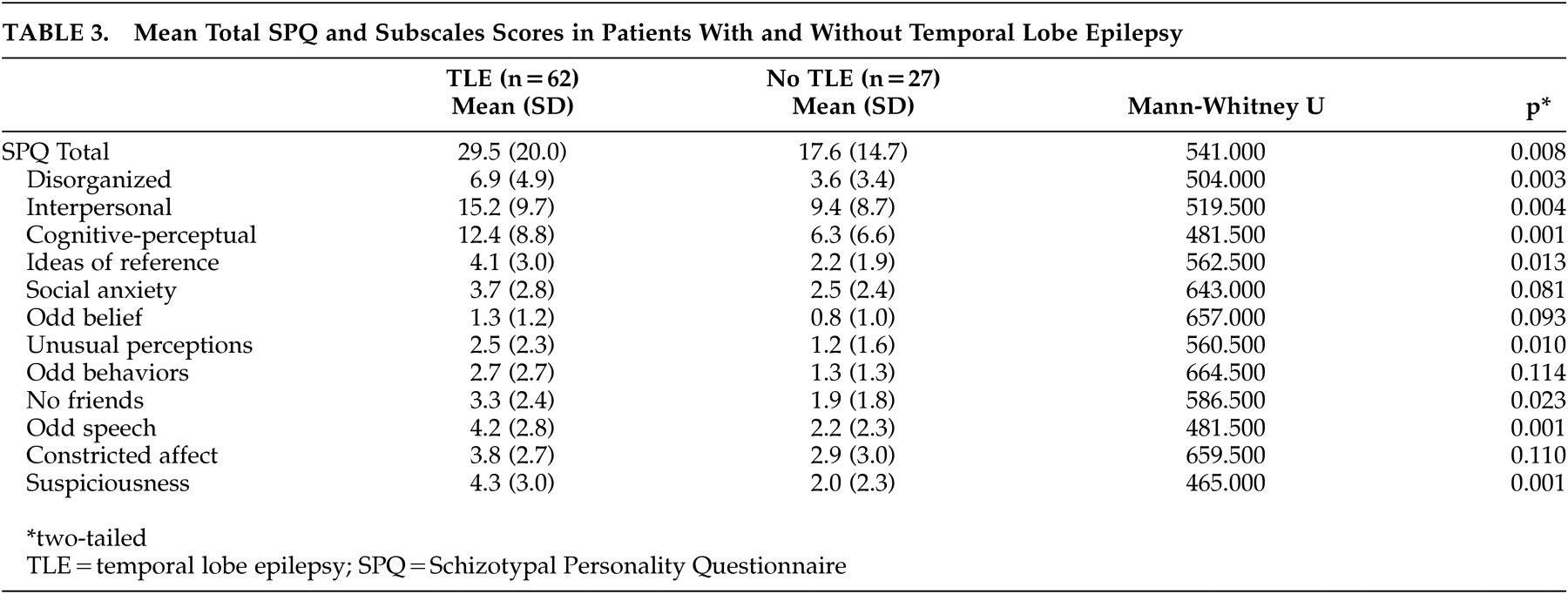
Patients with temporal lobe epilepsy had higher scores than patients without temporal lobe epilepsy for SPQ total scores, and subscales disorganized, interpersonal, cognitive-perceptual, ideas of references, unusual perceptions, no friends, odd speech, and suspiciousness (
Table 3 ). Logistic regression models including SPQ total scores, the three factors (disorganized, interpersonal, cognitive-perceptual), and the subscales ideas of references, unusual perceptions, no friends, odd speech, and suspiciousness showed that temporal lobe epilepsy diagnosis correlated specifically with SPQ total (OR=1.03; 95% CI=1.01–1.06, p=0.009), cognitive-perceptual (OR=1.10; 95% CI=1.03–1.17, p=0.004), and suspiciousness scores (OR=1.34; 95% CI=1.12–1.61, p=0.001).
DISCUSSION
To the best of our knowledge, this study is the first one to investigate associations between epilepsy and different dimensions of schizotypy using a validated psychometric instrument such as the Schizotypal Personality Questionnaire (SPQ). Our results suggest that SPQ-derived schizotypal symptoms are common in adult patients with epilepsy, particularly when compared with the normative sample of healthy subjects.
12,
14 Specifically, epilepsy seems to be associated with higher scores on the interpersonal factor, which includes symptoms of excessive social anxiety, no close friendships, and constricted affect. Particularly, those with constricted affect showed a significant negative correlation with age of onset of the epilepsy (OR=−3.04; 95% CI=−5.32 to −1.48, p=0.001). In the group of patients with temporal lobe epilepsy, this correlation was still present but weaker than that reported in the whole population. This is likely to be related to the small number of subjects investigated and might be more noticeable in larger samples. However, this association needs to be discussed in the light of previous literature.
7,
8There seems to be general agreement that patients with epilepsy and psychosis have an age of onset of seizures within early adolescence,
7,
8,
15,
16 but no studies clearly pointed out a relationship with a specific dimension of schizophrenia. Affective flattening is one of the diagnostic criteria for schizophrenia according to DSM-IV, being, together with alogia and avolition, one of the major negative symptoms. Literature about negative symptoms in seizure patients is scanty and our findings are consistent with a previous study supporting the hypothesis that negative symptoms are stable features of the interictal behavior in epilepsy.
17 Thus, someone would infer that our results further support the hypothesis that psychosis in epilepsy may have a strong biological basis as a consequence of early brain damage. However, the observed correlation of constricted affect scores with measures of anxiety and depression (STAI and BDI scores) raises a number of issues. The most important one is whether this SPQ subscale, namely constricted affect, truly reflects the affective blunting usually seen in psychotic and schizotypal patients and not merely the effects of depressed mood or avoidant personality features. Although depression is in general overrepresented among epilepsy patients, there was no correlation between age at onset of the epilepsy and BDI or STAI scores, making it unlikely that our findings represent just a bias due to the pervasive effect of mood disturbances. This further suggests that negative symptoms of schizophrenia are connected with the age at onset of the seizures in patients with epilepsy.
We need to consider the overlap between schizotypal and avoidant personality features. Conceptually, avoidant patients yearn for social relationships but require an unusually strong degree of acceptance before engaging in them because of their anxiety, while schizotypal individuals do not actively want or seek these relationships. In clinical practice, these distinctions can be difficult to make, especially when avoidant patients appear aloof and distant and there is a significant degree of cognitive impairment.
2 In our opinion, it is impossible to rule out that our data may reflect severe avoidant personality features due to poor self-esteem and a certain degree of cognitive impairment as a consequence of an early-onset seizure disorder. It is therefore evident that the significance of schizotypal features in epilepsy at a phenomenological level deserves further investigation.
The correlations between a diagnosis of temporal lobe epilepsy and total SPQ, cognitive-perceptual, and suspiciousness scores are much more in line with the hypothesis that psychoses in epilepsy have a strong biological component. Few controlled studies have demonstrated an increased incidence of psychoses in patients with TLE,
18 and it has been argued that TLE preponderance on interictal psychoses may be a bias and that patients with partial epilepsy, regardless of the localization of the focus, share similar processes in the development of psychiatric symptoms.
7,
8,
19 We agree that psychoses are multimodal phenomena and that other factors, not necessarily epileptogenic zones, are of relevance.
8 However, our findings support the assumption that temporal lobe dysfunction represents a fertile neurobiological ground for the development of schizophrenia-related personality features such as schizotypy and may be, therefore, of relevance for the development of a thought disorder. The temporal cortex, the frontal cortex, the striatum, and the thalamus have been particularly implicated, as regions of interests, in both schizophrenia and schizotypal personality disorder.
3 In particular, reduced size of the temporal cortex has been reported in schizotypal patients involving the superior temporal gyrus,
20 Heschl’s gyrus,
21 as well as the inferior and middle temporal gyri.
22 Although we fail to show that SPQ scores correlated with any major structural abnormalities in the temporal lobes, as detected with our routine MRI protocols, it has been suggested that these structures may be affected by developmental aberrations that can be detected with more sophisticated investigations.
23 However, our findings further support that temporal lobe alterations are associated with the core symptom profile of schizophrenia disorders, and this is further corroborated by correlations with the cognitive-perceptual factor (OR=1.10; 95% CI=1.03–1.17, p=0.004) that most closely parallels Jaspers’ concept of psychosis.
24Limitations of our study need to be acknowledged. First, the small sample size reduces the statistical power of our study. Second, our findings may not be representative of epilepsy patients in general because our population represents a selected sample coming mainly from a university-based referral center. It is possible that an individual with both epilepsy and schizotypal features is more likely to be referred to our clinic, and correspondingly patients in our clinic may represent individuals with more severe epilepsy and behavioral problems. Furthermore, psychosocial problems that arise from living with, and adapting to, a still stigmatized disorder such as epilepsy need to be taken into account, because these problems may contribute to the severity of associated psychopathology.
In conclusion, our study showed that schizotypal symptoms are common in adult patients with epilepsy and correlate with an early onset of the seizures and a diagnosis of temporal lobe epilepsy. At a theoretical level it is plausible that epilepsy and schizotypy may share a common pathoetiology, and our results are in line with a number of publications showing a complex relation between epilepsy and psychosis.
7 However, further studies are needed to replicate our findings and to shed light on the neurobiology of schizotypy, schizophrenia spectrum disorders, and epilepsy.