W ilson described the behavioral aspects of the disease almost a century ago and called these aspects “psychical.” Scheinberg and Sternlieb
1 reported that every patient with Wilson’s disease suffers from one or more behavioral symptoms at some point during the course of the illness. One-third of patients with Wilson’s disease may initially present with behavioral abnormalities, and failure to recognize this may lead to missed diagnoses, ineffective symptomatic therapy, unwarranted treatment such as ECT, increased morbidity, delay in starting specific treatment, and, on occasion, disastrous outcome of primary illness.
2 There are a few publications addressing psychiatric manifestations of Wilson’s disease as the predominant feature.
3 –
5 Predominant psychiatric presentation of Wilson’s disease occurs in 20% of patients, with mood abnormalities, personality disturbances, and cognitive dysfunction being the most common psychiatric symptoms.
6 Clozapine,
7 quetiapine,
8 and olanzapine
9 have been used effectively to treat symptoms in patients with Wilson’s disease with psychiatric manifestations. But severe extrapyramidal syndrome had been reported with the use of neuroleptics.
9 To the best of our knowledge, there are no reports of beneficial effects of mood stabilizers like lithium alone in patients with Wilson’s disease and mania.
Case Report
A 21-year-old man from an urban background in South India had been diagnosed with Wilson’s disease five years prior to his visit to our psychiatric service. He was on a regimen of zinc sulfate, 220 mg t.i.d., and penicillamine, 250 mg tablets b.i.d., for the past 2 years, and was asymptomatic except for slight slurred speech. A family history of Wilson’s disease was noted in his younger sister, who was 14 years old. She did not suffer from any comorbid psychiatric illness. There was no contributory past or family history of any psychiatric illness in our patient. He was referred to our psychiatric service after 3 months of illness, which had been worsening for 2 weeks. His family observed that he was more cheerful than his usual self, singing film songs and occasionally dancing to music. Gradually he began to voice special abilities of being able to clean the entire city in a day and claiming to have lakhs of rupees in his bank account.
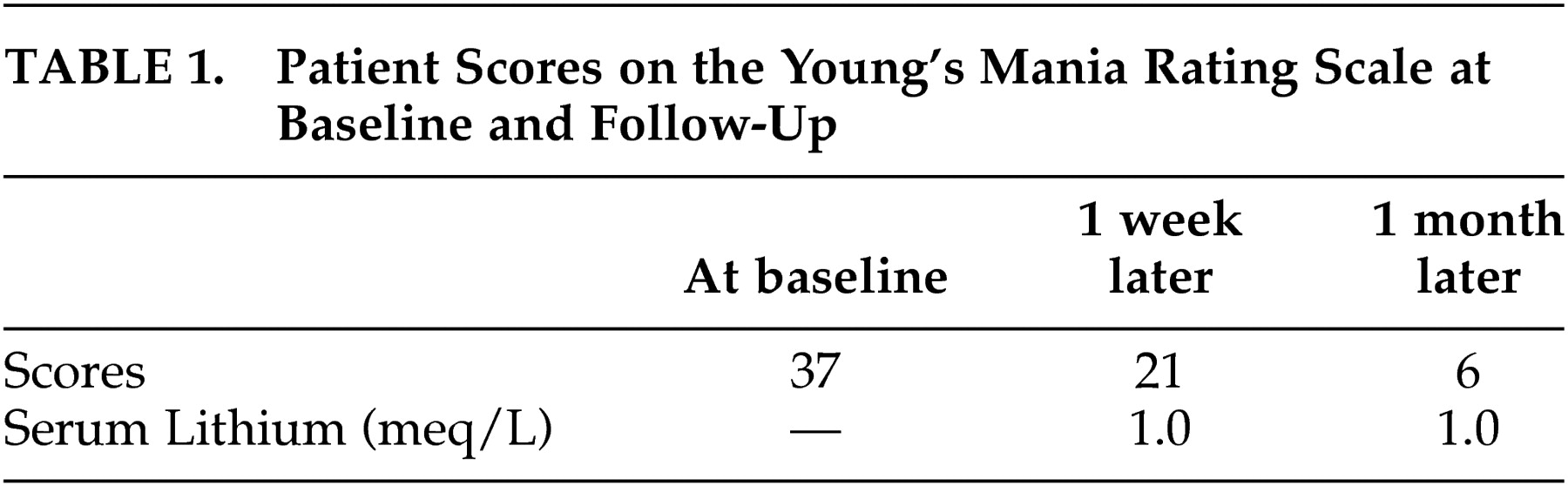
The patient claimed to be influential and to know the chief minister of the state personally. He spoke with strangers in a familiar manner, and on occasion he got irritable with some of them, leading to quarrels in his neighborhood. He was more active than his usual self and was seen to be restless; he also had decreased need for sleep. He asked for different varieties of delicious food to be provided to him. The patient’s doctors advised inpatient care. Mental status examination revealed over-familiarity, increased psychomotor activity, pressure of speech, elated mood, grandiose delusions, impaired insight, and poor social judgment. He was assessed with the Mini-International Neuropsychiatric Inventory and Young’s Mania Rating Scale on which he scored 37 at baseline (
Table 1 ).
On physical examination, the patient displayed slurred speech and a Kayser-Fleischer ring, which was confirmed through slit lamp examination. Investigations revealed urinary copper, 200 μg/24 hours (normal up to 70); serum ceruloplasmin, 9 mg/dl (normal 20–35); serum copper, 38 μg/dl (normal 80–130). Urine homocystine was negative. Ultrasound examination of his abdomen showed coarsened hepatic echo texture. He was diagnosed to have bipolar affective disorder.
The treating team decided to prescribe 5 mg tablets of olanzapine, taken once daily at bedtime, for controlling his manic symptoms, along with 2 mg tablets of trihexyphenidyl, three times a day. De-coppering treatment (zinc sulfate, 220 mg t.i.d., and penicillamine, 250 mg b.i.d.) was continued without any change in the dosage. The following day he was observed to have rigidity, bilateral hand tremors, and decreased arm swing, suggesting drug-induced extrapyramidal symptoms. The treating team decided to stop olanzapine and began a regimen of lithium, 300 mg t.i.d., which gradually decreased his manic symptoms; his extrapyramidal symptoms decreased significantly. By the end of the first week he was less talkative and stopped singing, with almost 50% reduction in his Young’s Mania Rating Scale score. The remaining symptoms and grandiose delusions also disappeared by the third week, and he was almost symptom-free at the end of 1 month. The patient was advised to continue taking lithium tablets, 900 mg/day (serum levels=1 meq/L), along with the other medication for Wilson’s disease.
DISCUSSION
The psychiatric manifestations of Wilson’s disease can be categorized into five groups of symptoms: personality changes, affective disorders, psychosis, cognitive impairment, and others.
10 A study from our center on 50 patients with Wilson’s disease revealed that 12 patients (24%) fulfilled the diagnostic criteria for a psychiatric diagnosis: 18% bipolar affective disorder (n=9), 4% major depression (n=2), and 2% dysthymia (n=1).
Our patient is a young man with a 5-year history of Wilson’s disease, who presented with manic symptoms that started 3 months prior to his visit. The treating team considered the diagnosis to be bipolar affective disorder. We do not know if this patient’s bipolar affective disorder is independent of his Wilson’s disease. The law of parsimony would suggest that the two are connected. On the other hand, it is unusual that his bipolar affective disorder occurred 5 years after his Wilson’s disease was diagnosed and treated. In our patient there were severe extrapyramidal symptoms with olanzapine, and hence it was stopped. This sensitivity to olanzapine could have been because he is a young male, generally known to have a higher propensity for extrapyramidal symptoms with the use of neuroleptics. Since lenticular (source of dopamine) degeneration is the hallmark of this disorder, dopamine is already depleted in the affected regions. With the addition of olanzapine (which blocks nigrostriatal dopamine), an already depleted basal ganglia is further deprived of dopamine. This could also explain his sensitivity to olanzapine. One should be careful while using neuroleptics in the treatment of psychosis or acute control of mania and avoid using typical antipsychotics as they can cause severe extrapyramidal symptoms. Various reports have stated the use of antipsychotics like clozapine,
7 quetiapine,
8 and olanzapine.
9 Patients with Wilson’s disease are more vulnerable to agranulocytosis due to hypersplenism and/or penicillamine. Clozapine, sometimes used in Wilson’s disease patients,
7 might not be a suitable option in such patients as it can enhance the risk of agranulocytosis. Lithium, which is not metabolized by the liver (which could be affected in Wilson’s disease), however, stimulates granulocyte production and might be a much safer option over clozapine in certain patients. In a patient whose mania was inadequately controlled with quetiapine alone, lithium was added to achieve control for a year.
8 The problem with using olanzapine is its propensity to cause weight gain along with other metabolic side effects such as glucose and lipid abnormalities.
Sometimes extrapyramidal symptoms can baffle clinicians and resemble symptoms of Wilson’s disease itself. Before starting antipsychotics in such patients, the available mood stabilizers should be explored. We would recommend clinicians use caution with typical and atypical antipsychotics in Wilson’s disease mania and consider mood stabilizers, such as lithium, as an option. Other mood stabilizers can be considered as well, depending on the patient profile, symptom profile, and side effects. Valproate has been recommended for mania associated with neurological or organic features,
12 as would have been appropriate in this patient. Lithium was chosen for our patient, however, due to the euphoric mania and affordability of medication by the patient.
Whether or not the bipolar affective disorder is independent of his Wilson’s disease, we believe that this case report should be of interest to all physicians who treat patients with Wilson’s disease. As we have reviewed above, psychiatric symptoms are common in Wilson’s disease, and physicians may consider mood stabilizers (such as lithium) in the management of selected patients with Wilson’s disease. We have also shown in this case report that Wilson’s disease may be associated with a peculiar hypersensitivity to olanzapine.