To the Editor: Studies and case reports of complex auditory epileptic hallucinations are scarce in the literature.
1 –
5 To date, the cortical origin of auditory hallucinations is still debated.
6 We report a patient presenting with complex partial seizures and complex ictal auditory experiential phenomenology associated with a lesion occupying the left superior temporal gyrus. The lesion was diagnosed on histopathology as angiocentric glioma, a rare epilepsy-related and newly recognized clinicopathological entity.
7 Case Report
A 28-year-old single, right-handed unemployed man presented with a 7-year history of disabling, refractory epilepsy, originally presenting as a generalized seizure around the time of his mother’s death. In retrospect, it appeared that he probably had minor unrecognized attacks throughout his childhood. His habitual seizures began with unilateral muffled sounds in his right ear followed by altered awareness and a staring spell, sometimes accompanied by falling down. Indistinct sounds, music, or even a complex external auditory stimulus such as conversation could also trigger them. Ictal aphasia, déjà vu, epigastric discomfort, and some right arm movements were also described. With time, his ictal experiential phenomena became more elaborated, if still brief, and commonly consisted of derogatory second- or third-person voices arguing (e.g., “We got you” or “He’s got no guts”). Later he claimed he could hear his late mother’s voice asking him brief reassuring questions such as “Are you OK?” The attacks lasted for about 10–20 seconds, appeared up to seven times a week, and were associated with postictal dysphasia lasting for several minutes. He was usually amnesic for the attack; however, sporadically he could recall his hallucinations. Over the years, he developed his own methods of trying to ignore these voices and learned to live with his attacks.
He had delayed speech, an operation for grommets as a child, and a documented seizure at the age of four. His premorbid personality was described as dependent and sensitive. However, his psychiatric history was otherwise insignificant, and he never experienced a psychotic state independent of his seizures. His family history was somewhat unusual in that his father had acoustic neuroma, his paternal grandfather was deaf in one ear, and his paternal aunt apparently turned deaf at the age of 11. His paternal uncle died of a brain tumor, while several cousins had epilepsy. General mental, cognitive, and physical examinations were otherwise normal.
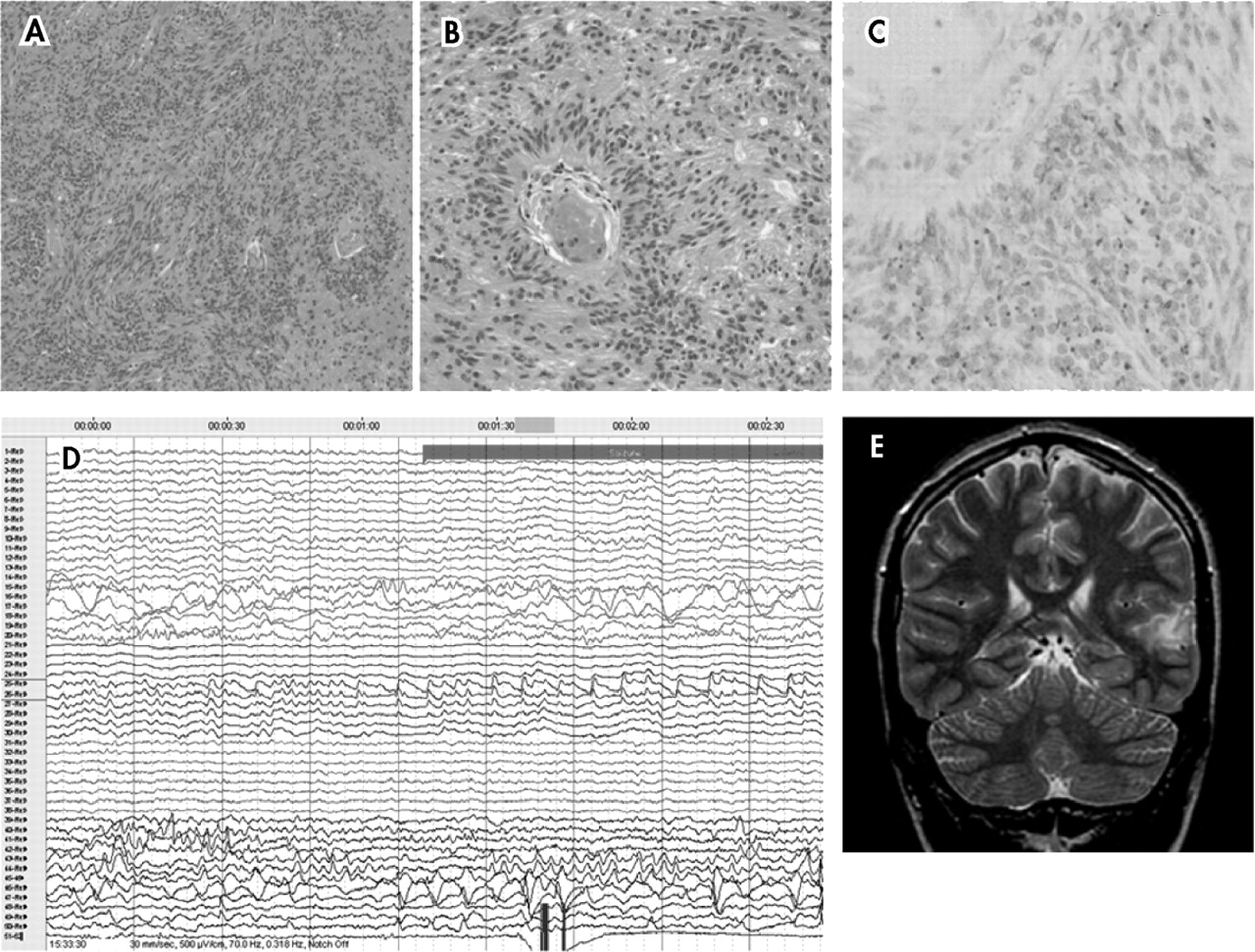
An MRI scan of his head was obtained, and it revealed a lesion involving both gray and white matter of the left superior temporal gyrus, extending into posterior association areas (
Figure 1, panel E). As a part of the multidisciplinary presurgical investigation, we made an intracranial EEG recording using an array of surface electrodes placed over the cortex of the left temporal lobe and Sylvian fissure. The fissure was opened, and an intracerebral depth electrode was also placed. This all allowed for careful speech mapping which demonstrated that speech areas were involved with, or at least very close to, the lesion. During the telemetry several paroxysmal ictal phonemes were reported and electro-clinically confirmed (
Figure 1, panel D). For example, while he reported hearing people singing a song, the epileptiform activity was recorded in the middle of the Sylvian depth electrode. During another recorded episode, a male voice kept saying “Tonight is your night.”
Functional MRI and intracarotid amytal (Wada) test showed that he was left hemisphere dominant, following which a near complete neurosurgical removal of the lesion was done. Resection of the lesion was carried out under local anesthesia, to reduce the risk of severe speech dysfunction. Neuropathology revealed a superficial, diffusely infiltrative tumor composed of uniform bipolar astrocytes with a compact fascicular arrangement around blood vessels, which was diagnosed as an angiocentric glioma, grade I (
Figure 1, panels A–C). The surgical removal of the tumor rendered him seizure-free on antiepileptic medication. No further paroxysmal auditory hallucinations have been reported, and a follow-up MRI scan showed no recurrence 2 years after neurosurgery.
Discussion
Previous neuroimaging studies report a volumetric and functional reduction of the left superior temporal gyrus in schizophrenia patients with severe auditory hallucinations.
8 Although auditory hallucinations are classically found in schizophrenia, they can also be a result of brain damage, most commonly an injury to the superior temporal auditory association areas.
9 Penfield and Perot
3 discovered that stimulation of this area induces an auditory sensation, which appeared real to patients. Auditory hallucinations can also occur as a result of temporal lobe epilepsy (TLE).
2 Familial, sporadic, and reflex-type TLE with auditory auras have also been described.
10 –
12 Their semiology points to an extrahippocampal area although no MRI abnormalities have been found so far.
10 –
15 The mutations in leucine-rich, glioma inactivated gene 1 (LGI1) gene on human chromosome 10q24 were implicated in cases of both reflex-type
12 and familial TLE with auditory auras.
13 –
15The pathophysiological mechanism of complex hallucinations in our patient, who also had striking familial preponderance for epilepsy, deafness, and brain tumors, is unclear. There is an obvious overlap of anatomical site of abnormality in this case with those previously shown in schizophrenia patients with auditory hallucinations. Also remarkably, a number of the recorded ictal phonemes here were of Schneiderian first-rank type
16 and included voices discussing the patient in the third person. Furthermore, reminiscent of those reflex-type telephone-induced seizures described by Michelucci et al.,
12 some of the reported attacks in our patient also appeared to be triggered by the external complex auditory stimuli.
To our knowledge, this is the first report to show the association of probable TLE and auditory auras with an angiocentric glioma, the resection of which abolished both. Finally, as future studies start unraveling molecular genetic properties of angiocentric glioma, it will be interesting to see whether any common mutations with those present in familial TLE with auditory auras will emerge.