To the Editor: Arachnoid cysts account for 1% of all intracranial space-occupying lesions. They have an unknown course, and the presenting signs and symptoms are unpredictable and usually related to the size and location of the cyst.
1 The most common presenting symptoms of these cysts are neurological disturbances, such as headache, intracranial hypertension, visual loss, seizures, or focal neurological signs, but mental impairment is rare.
2 There have been few reports of an arachnoid cyst accompanying psychiatric disturbance. We report on a patient with a posterior fossa arachnoid cyst who presented with drop attacks and was diagnosed with conversion disorder.
Case Report
A 45-year-old man presented to the physician with complaint of sudden, unexpected falls from sitting as well as standing positions, lasting for about half an hour and occurring about four to five times a day for the preceding 25 days. He had never hurt himself nor had any spells of dizziness, light-headedness, blurred vision, loss of balance, or loss of consciousness before or during the fall. Between episodes, he could recall what instructions were given to him when he had fallen down, but reported that he was unable to speak. There was no history of headache, palpitations, sweating, nausea or vomiting, vertigo, seizures, or head injury. Perinatal and childhood history was uneventful. Medical history and substance history was negative. He was admitted to the hospital with a provisional diagnosis of drop attacks under investigation. Detailed physical examination revealed neither clinically attentive findings nor focal neurological symptoms and signs. Blood pressure was 170/110 mm Hg in supine position without any postural fall. Laboratory studies were negative for any physical illness. Fundus examination, ECG, and x-ray of the cervical spine did not reveal any abnormality. A brain CT scan revealed an extra axial cystic lesion of approximately 4 cm by 8 cm in the posterior fossa. Antihypertensive medications were started, and his blood pressure stabilized to 140/90 mm Hg. He was kept under observation for 10 days with stable blood pressure, but he continued to suffer from drop attacks with the same frequency.
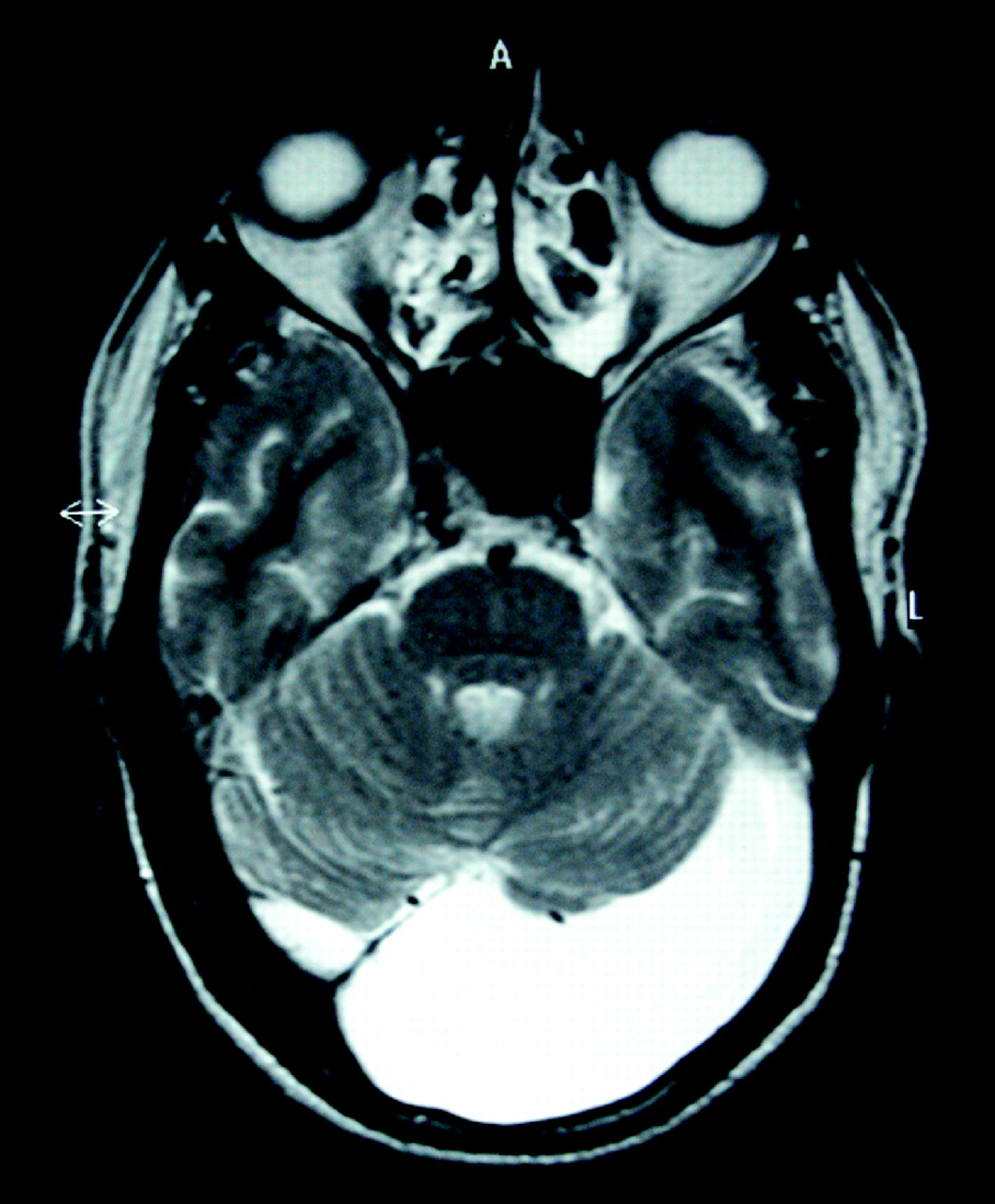
The consulted neurologist (SP) advised an MRI, magnetic resonance angiography (MRA), carotid Doppler studies, and EEG. All investigations turned out to be normal; however, the MRI image showed a well defined nonenhancing intracranial homogenous lesion in the left side of posterior fossa, posterior to the cerebellum (
Figure 1 ). The lesion being homogeneous, with CSF signal intensity on T1-weighted, T2-weighted, and FLAIR sequences, and with no perceptible wall or internal complexity, was identified as an arachnoid cyst. It demonstrated mass effect with an en bloc displacement of the cerebellum and vermis anteriorly. Although space-occupying lesions in the posterior fossa are known to cause drop attacks, sudden onset of the same, and absence of any other identifiable abnormality, demanded probing into further differential diagnosis.
On psychiatric evaluation (SD), it was revealed that 20 days before the onset of symptoms, he witnessed his mother’s death followed by a crisis within the family related to inheritance issues. During the episodes of drop attacks, it was found that there were crying spells. There was no history suggestive of a mood disorder or a psychotic disorder. Past history or family history for psychiatric disorders was negative. On mental status examination, he looked older than his stated age, was shabbily dressed with a partially overgrown beard, and reported anxious mood with appropriate affect. His thought disturbance revealed ideas of helplessness and rumination related to his mother’s death. A diagnosis of conversion disorder was made, and a 45- to 50-minute therapeutic interview, aimed at catharsis of the repressed feelings, was conducted. The patient cried during the interview and expressed his stresses as well as ongoing conflicts. He was prescribed tablet lorazepam, 2 mg/day at night time. On follow-up after 7 days, it was found that his drop attacks had stopped completely. He was advised to continue with the same treatment, and on follow-up visits at 15 days, 30 days, 45 days, and 60 days, the patient did not report any drop attacks.
Discussion
The conglomerate of signs and symptoms in neurology and psychiatry has historically proven difficult to differentiate. This case report discusses the possibility of a causal relationship between the MRI-identified lesion, the somatic symptom, and the psychiatric disorder.
Although space-occupying lesions in the posterior fossa are known to cause drop attacks, sudden onset and persistence of the attacks in the absence of any complication, and the immediate response to catharsis interview and lorazepam treatment, point toward its psychogenic origin. Arachnoid cysts are usually asymptomatic (even when the cyst is quite large) and are often an incidental finding on imaging.
3 Continuation of drop attacks even after control of hypertension ruled out its role.
It is possible that the patient’s neurological lesion coexisted with the psychiatric disorder and that it was an incidental finding without functional importance or correlation.
It may be possible that the conversion disorder itself may have its origin in the organic pathology. In patients diagnosed with conversion disorder, evidence of current or previous comorbid neurological disorders is reported to be 18% to 64%. What is typically seen in these comorbid neurological and psychiatric conditions is an elaboration of symptoms stemming from the original organic lesion.
4 Cerebellar lesions have been correlated to various psychiatric disorders, including schizophrenia, in the literature.
5 There have also been reports of patients hospitalized for psychiatric symptoms who were later found to be having cerebellar pathology.
6The interesting aspect of this case report is that although studies mention various types of conversion syndromes in neurology patients, drop attacks have been reported less frequently.
7 Also, to the best of our knowledge, in the very few case reports available in the literature, arachnoid cyst has been mainly correlated with psychosis, but never with conversion disorder.
8Thus, treatment programs in neurology are likely to be more successful if there is close collaboration between neurologists, consultation-liaison psychiatrists, psychologists, and general practitioners.