Depressive disorders (DDs) are the most common type of psychiatric comorbidity in patients with epilepsy.
1 DDs are more likely to occur in patients with partial seizures of frontal and temporal lobe origin, versus generalized seizure disorder.
2 Depression and epilepsy share common pathogenic mechanisms that facilitate the occurrence of one in the presence of the other.
3The interrelationship between hormonal changes and epileptic seizures is complex because hormones may alter brain excitability, and seizures alter hormone secretion and metabolism. The essential feature of depression is sustained hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis,
4 which in turn leads to changes in certain hormonal levels, that is, in cortisol, prolactin, and thyroid hormones.
5 Epileptic seizures, mainly tonic–clonic, but also complex partial and sometimes simple partial seizures, result in hormonal storms. Immediately after seizures, there are changes in serum concentrations of prolactin, cortisol, T3, thyroxin (T4), and thyrotropin. Free testosterone levels are decreased in men with epilepsy.
4 Whereas prolactin changes tend to persist for about 24 hours after the convulsions, the other hormonal changes last only 2 hours.
5It is important to emphasize the presence of subsyndromal symptoms and features of DDs, which can increase disability and contribute to the hormonal changes noted. Unfortunately, in two-thirds of epilepsy patients with DDs, the diagnosis is missed.
6There are several possible etiologies for the comorbidity of depression and epilepsy that may contribute to the hormonal changes noted in individuals with these disorders. First, both disorders have genetic predisposition, with over 50% of epileptic patients with depression having a positive family history of psychiatric illness, especially affective disorders.
2 Second, patients with these disorders may feel stigmatized,
7 which may lead to social problems.
8 The stigma may result in a state of learned helplessness.
9 Third, the pathophysiology of depression and epilepsy includes changes in common neurotransmitters, particularly serotonin, dopamine, noradrenaline, and gamma amino butyric acid (GABA).
10There are several epilepsy-related factors that may contribute to the presence of depression as well as the hormonal changes noted. For example, depression is more common in patients with complex partial seizure (CPS), particularly of temporal lobe origin.
2 Depression is also more common in epileptic patients with left-sided epileptic foci,
2 which was associated with hypometabolism of the left hemisphere during ictal periods.
This study was therefore conducted to compare serum concentrations of cortisol, testosterone, prolactin and thyroid hormones in drug-naive epileptic (CPS) and generalized tonic–clonic (GTC) patients with and without clinical depression.
11 Because we compared levels of testosterone, the sample was limited to men.
METHOD
Subjects
Sixty men were recruited and examined: 20 patients with epilepsy without a history of depression, 20 epilepsy patients who were clinically depressed, and 20 healthy control (HC) subjects comprised the three study groups. Epileptic patients were classified according to the international classification of epileptic seizures.
12 All patients were recruited from the neuropsychiatric outpatient clinic and inpatient service in Tanta University Hospital (Egypt) between April 2003 and April 2004. All patients were newly diagnosed and medication-naive. The entire study was completed before any medications were started. The patients were seen by the lead author in the epilepsy clinic. Subjects who met inclusion criteria for the study were administered the Hamilton Rating Scale for Depression (Ham-D) and reported on a detailed history of their seizures; including seizure semiology and frequency. Patients were then scheduled for an EEG and fasting blood sample both to be performed the following morning at around 9 A.M. The study was considered completed at that point. Patients were then started on medical treatment. Treatment was never delayed beyond 48 hours. Patients who had had seizures within the last 48 hours were excluded. History of seizure frequency and semiology of seizures were verified by accompanying relatives. Most of the included patients were seeking medical advice for the first time despite history of seizures in the previous 3 to 6 months. The nondepressed epileptic patients included 10 subjects with GTC, and 10 patients with CPS without history of secondary generalization. Depressed epileptic patients included 10 subjects with GTC seizures and 10 subjects with CPS without a history of secondary generalization. All patients had primary epilepsy; patients with secondary epilepsy were excluded. Patients were excluded if they were receiving any hormonal therapy or diagnosed with an endocrine disorder or any other neurological disorder. Twenty healthy men matched for age with the two epilepsy groups were included. Consistent with the matching criterion, the mean age of the study groups revealed no significant differences (
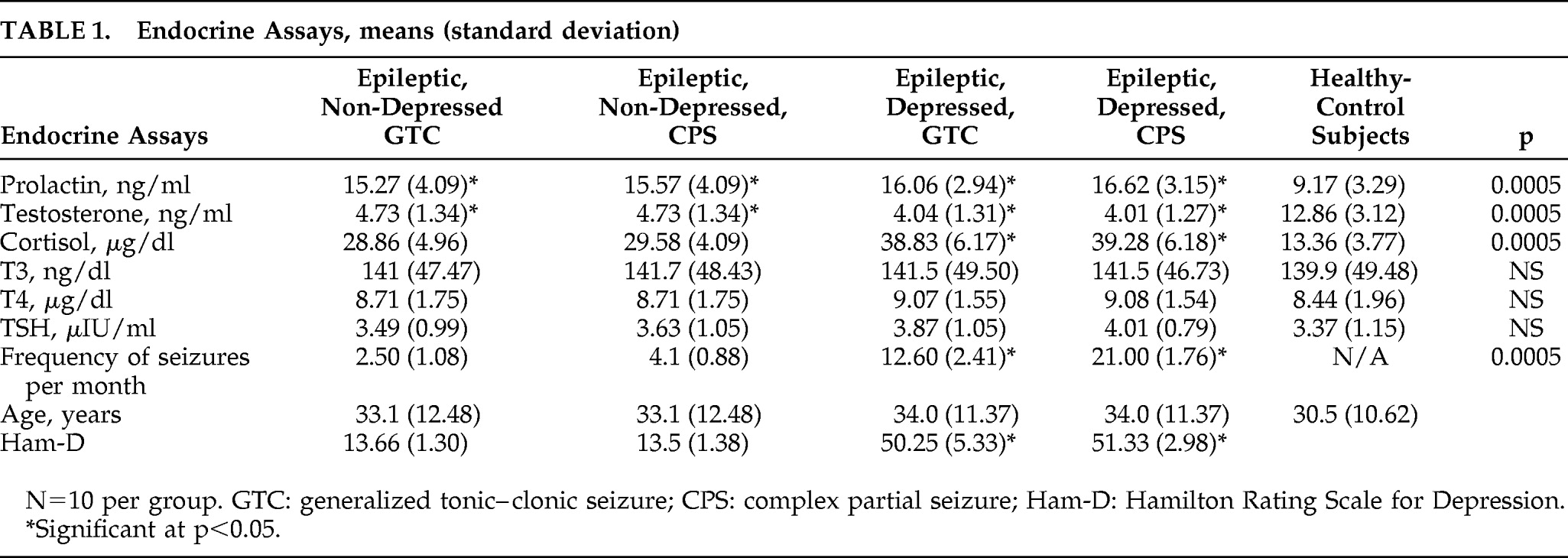
Table 1).
Informed consent was obtained from all subjects, and the study was approved by the Ethics Committee of Tanta University. All subjects underwent a complete history and physical examination, neurological examination, and psychiatric assessment with a clinical interview conducted by a psychiatrist faculty member. All patients received an MRI scan as a part of the routine evaluation so that any abnormality indicating secondary epilepsy led to prompt exclusion. The 24-Item Ham-D was administered to all patients. The Ham-D was not formally administered to the healthy-control subjects. Exclusion criteria for healthy-control subjects included history of any neurological or chronic medical problems that could influence endocrinological assessments. Control subjects were also excluded if they endorsed any depressive symptoms. This was necessary to assure the exclusion of any subsyndromal depression (
Table 1).
Electroencephalogram (EEG)
All patients were subjected to EEG examination using scalp electrodes applied according to the 10–20 system. The device used was DaiHic-Medtronic PI,-EEG 28-channel in the EEG unit of neuropsychiatry department in Tanta University Hospital. The EEGs were interpreted by a neurology faculty member who was blind to the patients' group.
We assayed serum levels of prolactin, testosterone, thyroid hormones, and cortisol. Blood samples were obtained at the same time (mid-morning) in all subjects.
Statistical Analysis
The collected data were analyzed using SPSS Version 10. For comparison between means, the F value of analysis of variance (ANOVA) was calculated with the post-hoc test for differences using Scheffé's test. Pearson's correlation coefficient was calculated to assess the magnitude of the association between two variables. For categorical variables, the chi-square test was used to test for significance and, if inappropriate because of small expected cell sizes, Fisher's exact test was used. Significance level was set at p<0.05.
RESULTS
Serum cortisol levels were significantly higher in both patient groups (F=41.976, p<0.0005) than in the healthy-control subjects. Cortisol levels were also significantly higher (p=0.05) in the depressed (38.83 (SD: 6.2) for GTC; 39.28 [6.2] for CPS) than those in the nondepressed epileptic patients (28.9 [5.00] for GTC; 29.6 [4.00] for CPS).
Serum testosterone levels were significantly decreased in both patient groups as compared with the healthy-control subjects (F=63.737, p<0.0005). Although the differences between the two patient groups did not reach significance, testosterone levels were consistently lower in depressed patients (4.04 [1.3] for GTC; 4.01 [1.3] for CPS) than nondepressed patients (4.73 [1.4] for GTC; 4.73 [1.34] for CPS). Post-hoc power calculations suggested that sample sizes of 50 to 60 per group would be needed to detect a significant difference with 80% power. No differences were noted in the testosterone levels between patients with GTC and CPS.
Serum prolactin was significantly higher in both patient groups than in the healthy-control group (F=7.886, p<0.0005). There were no significant differences between the two patient groups or between patients with GTC and CPS.
The thyroid hormones (T3, T4, TSH) did not differ between patients and control subjects or by patient group. There was a significant (p=0.0005) positive correlation between the frequency of seizures and serum concentrations of cortisol (r=0.73), prolactin (r=0.42), and testosterone (r=–0.53). There were also significant (p<0.0005). correlations between the Ham-D scores and the hormonal levels of cortisol (r=0.83), testosterone (r=–0.67), and prolactin (r=0.49). There was no significant correlation between the frequency of seizures and Ham-D scores.
DISCUSSION
In this study, cortisol levels were significantly elevated in all epileptic patients versus the healthy controls. Cortisol levels were also significantly elevated in the depressed as compared with the nondepressed epileptic patients. This observation suggests that the effects of the two disorders on cortisol levels may be additive; thus possibly increasing the deleterious effects of cortisol in depressed epileptic patients. Comparison with depressed nonepileptic patients would further address this issue. We hypothesize that the chronically stimulated HPA axis prevents the return to baseline of elevated cortisol level after seizures. In agreement with our study, Parker et al. reported that, in acute depression, ACTH levels are increased, whereas, in chronic depression, the high levels of cortisol are due to increased adrenal responsiveness to circulating ACTH.
14 In individuals with unipolar depression with psychotic features, the chronic elevation of cortisol may lead to dopaminergic, noradrenergic, and thyroid dysfunction.
15The marked decrease in testosterone levels in patients with epilepsy suggests that epilepsy per se suppresses the gonadal axis. Our data are consistent with the findings that all forms of epilepsy (focal, temporal, GTC, treated, and untreated) decrease serum free-testosterone and increase serum estradiol levels.
16Pope and colleagues
17 reported that men with refractory depression and low free-testosterone levels who were randomized to testosterone-replacement therapy or placebo in addition to their ongoing antidepressant therapy regimen, had significantly greater improvement on the Ham-D if they received testosterone. The significant correlation between seizure frequency and testosterone level suggests that in some patients replacement therapy may be of value. In agreement with this study, Hamed and colleagues
18 found that the risk of hyposexuality and reproductive disturbances is high in epileptic patients with GTC convulsions despite the antiepileptic drugs (AEDs). The risk is further increased by poor seizure control, which was frequently accompanied by depressive manifestations. It is also possible that the elevated estradiol (E2) increases the risks of seizure by reducing active testosterone through negative feedback, which could in turn increase the seizure intractability to AEDs.
In the present study, there were significantly higher serum prolactin levels in both depressed and nondepressed epileptic patients in both subtypes as compared with a healthy-control group. This is usually explained by the hormonal storm or the direct effect of the electrical activity on the brain, which may impair the hypothalamus control of prolactin secretion by increasing the release of prolactin-releasing peptides and/or suppressing the dopaminergic output to the anterior pituitary gland. Dopamine suppresses the prolactin-secreting cells of the anterior pituitary gland and, at the same time, stimulates the hypothalamic–gonadal axis. Suppression of dopaminergic neuron activity thus is predicted to result in hyperprolactinemia and suppression of the gonadal axis. Elevated prolactin has been associated with psychiatric symptoms such as anxiety, depression, hostility, and aggression.
19 Psychiatric disorders in general are associated with hyperprolactinemia, which, in turn, is a risk factor for depression and anxiety, which also may require a specific therapeutic approach.
19 Also of interest, Koppelman and colleagues
20 reported that in depressed patients bromocriptine can be used as an antidepressant even in patients with normal prolactin levels. In agreement with the current study, it was found that a high prolactin level within 100 minutes of a seizure suggests that a generalized or complex partial seizure has occurred.
21There was a significant correlation between the frequency of seizures and cortisol, prolactin, and testosterone levels. These correlations may have implications for prevention and/or treatment of epilepsy. Further ascertainment of these relationships requires a larger sample. The above data suggest that the interrelationship between epilepsy, depression, and endocrinal changes is complex and deserves further study.
Finally, we found that there were no differences in the thyroid hormones T3, T4, or TSH in the three groups studied. In contrast with our findings, it has been reported that depressed patients may have alterations in TSH in response to TRH from the hypothalamus, and this hypothalamic-pituitary alteration may be partially a trait or partially a state response.
22 These findings suggest that thyroid changes may be subtle and require activation procedures in order to detect deviations in epileptic, depressed, or dually afflicted individuals.
The main limitation of the current study is the small sample size and the absence of the nonepileptic depressed group. The small sample utilized in the current study did not allow the full examination of differences. For example, the comparison of testosterone levels between depressed GTC epileptic patients (4.04 [1.35] ng/dl versus 4.73 [1.35] ng/dl for the nondepressed GTC patients, we would need 62 patients per group in order to have 80% power to detect a two-sided difference at α ≤0.05. The comparison of testosterone levels between depressed CPS epileptic patients (4.01 [1.27] ng/dl versus 4.73 [1.34] ng/dl for the nondepressed CPS patients) requires 54 patients per group in order to have 80% power to detect a two-sided difference at α=0.05. Furthermore, a depressed nonepileptic group was not included for comparison; it should be included in future studies.