Over 59 million people, or 20% of the United States population, live in rural communities.
1,2 Significant health disparities have been linked to rural residence, including higher rates of premature mortality
3 and chronic disease (e.g., hypertension),
4 as well as overall poorer health status, as compared with urban areas.
5 Therefore, more research is needed on a broad range of health-related topics regarding the aging population, especially women, living in rural U.S. regions. This study sought to contribute to the literature on rural women's health by examining the relationship between thyroid functioning and cognition in a sample of rural-dwelling women. The link between thyroid function and cognition is a topic that has intrigued scientists for the past two decades. It is commonly understood that thyroid functioning plays an important role in cognition over one's lifetime,
6 with several prospective studies linking markers of thyroid functioning with cognitive decline. In the Kungsholmen Project, thyroid-stimulating hormone (TSH) levels within the normal range, but not FT4 (free T4), were associated with decline in cognition.
7,8 However, in the Women's Health and Aging Study and the MRC Cognitive Functioning and Aging Study, FT4 levels, but not TSH, were associated with greater risk of cognitive decline.
9,10 When looking at risk for Alzheimer's disease (AD), low TSH has been found to be a risk factor for AD, independent of cerebrovascular factors.
11 In the Framingham Study, low and high levels of TSH were associated with increased incidence of AD in women, but not in men.
12 Combined, these results provide strong evidence for the link between cognitive functioning and thyroid markers; however, they also point to the potential differential impact of different markers of thyroid functioning on neuropsychological domains.
The current study was undertaken to provide the first in-depth examinations of the link between thyroid markers and neuropsychological functioning among rural-dwelling women within the U.S. We hypothesized that both TSH and FT4 would be significantly associated with neurocognitive domain scores among women enrolled in the ongoing rural health study, Project FRONTIER.
METHOD
Sample
The study sample consisted of 82 rural-dwelling women (Hispanic: N=34, non-Hispanic: N=47, no ethnicity reported, N=1) from Project FRONTIER (Facing Rural Obstacles to healthcare Now Through Intervention, Education & Research). Project FRONTIER is an epidemiological study of health issues among rural-dwelling individuals in West Texas. A detailed description of Project FRONTIER has been provided elsewhere.
13 The mean age of the participants was 66.4 years (standard deviation [SD]: 14.8; range: 41–97), and the years of education was 10.5 (SD: 3.96; range: 2–20). Fifty-six percent of the sample reported an annual income below $20,000.
Any participant with TSH or FT4 levels beyond 4 SDs outside of the mean were not included in analyses; only one participant was excluded on the basis of these criteria. Mean TSH level was 2.3 (SD: 2.42), indicating that the majority of the sample fell within normal range (0.5–5.00). The mean FT4 level was 1.04 (SD: 0.28), again, indicating that the majority of the sample fell within the normal range (0.7–1.8). On the basis of consensus review of medical examinations and clinical labs, there was 1 participant with hyperthyroidism and 20 with hypothyroidism. ANOVA findings revealed that there were no significant differences in levels of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) scores between the euthyroid and hypothyroid groups (p>0.05 for all indices).
Measures
TSH and FT4 tests were conducted under fasting conditions in the morning by the community hospital, a Clia-certified lab. Neurocognitive status was assessed with the RBANS. The RBANS was developed to identify and characterize abnormal cognitive functioning in older adults and as a neuropsychological screening battery for younger patients.
14 It is a brief, highly portable test with extensive normative data,
15 which has demonstrated good psychometric properties
16–18 and is capable of distinguishing between different cognitive domains.
19 The RBANS consists of 12 subtests that yield 5 indices of cognitive functioning, including Immediate Memory, Visuospatial/Constructional, Language, Attention, and Delayed Memory.
14 The subtests that make up the five indexes are detailed below:
1.
The Immediate Memory index consists of two subtests: a) List Learning, which consists of immediate recall of a 10-item list of words over four learning trials; b) Story Memory consists of a 12-item story, read aloud for immediate recall over two trials.
2.
The Visuospatial/Constructional index consists of two subtests: a) Figure Copy consists of copying a geometric figure comprising 10 parts; b) Line-Orientation consists of a 10-item line-orientation test. Each item involves a radiating array of 13 lines, spanning 180°. Below this array are two target lines that are identical in orientation to two of the lines from the array. The subject must identify the matching lines.
3.
The Language index consists of two subtests: a) Picture Naming consists of 10 line drawings that the subject must name; b) Semantic Fluency consists of the total number of examples generated by the subject for a given semantic category (e.g., fruits and vegetables) within 60 sec.
4.
The Attention index consists of two subtests: a) Digit Span, which consists of two strings of digits in each item, at lengths increasing from 2 to 9 digits. The second string is only read if the first string is failed; b) Coding, in which the subject must match symbols and write a number that corresponds to the matching symbol in 90 sec.
5.
The Delayed Memory index consists of four subtests: a) List Recall involves the subject's free recall of the words from the List-Learning task; b) List Recognition involves Yes/No recognition testing for memory of the words from the List-Learning task; c) Story Recall involves free recall of the story from the Story-Memory test; d) Figure Recall involves free recall of the figure from the Figure Copy subtest.
Data Analyses
Data were analyzed using a linear-regression model, with TSH and FT4 levels as predictor variables and age-corrected RBANS index scores as outcome variables, and education entered as a covariate. The significance level was set at p<0.05. Post-hoc regression analyses were conducted to examine the influence of the thyroid markers on specific subtests that make up the RBANS index scores.
RESULTS
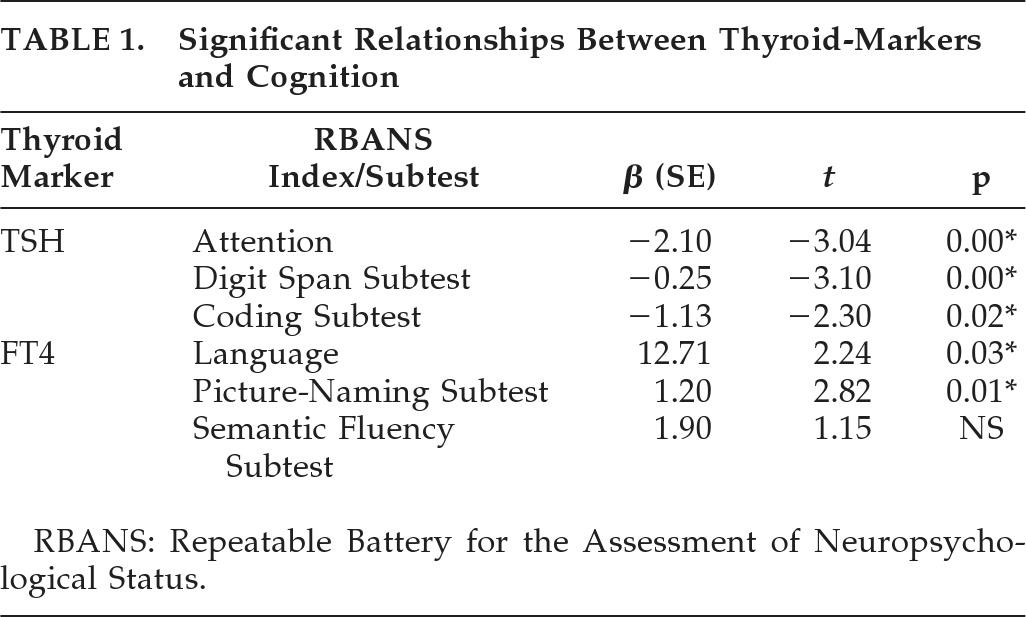
Results indicated that TSH significantly predicted the RBANS Attention index, but not other RBANS indices (Language, Visuospatial Skills, or Immediate and Delayed Memory). Follow-up regression analyses on the subtests that make up the RBANS Attention index revealed that TSH levels were significantly related to both Digit Span and Coding (see
Table 1).
FT4 levels were significantly related only to the RBANS Language index. Post-hoc analyses revealed that FT4 was significantly related to the Picture-Naming subtest of the Language index, but not the Semantic Fluency subtest.
DISCUSSION
Despite the fact that approximately 30 million women live in rural areas, there is a dearth of research investigating the various health needs of this segment of the U.S. population. The current study sought to contribute to the literature by examining issues related to the mental health of rural-dwelling women. The current findings indicated that TSH and FT4 were significantly but differentially related to neurocognitive domains among rural-dwelling women. Specifically, elevated TSH levels were related to poorer scores on measures of attention, whereas lower FT4 levels were specifically associated with poorer scores on tests of language.
The current study, although preliminary, points to the need to consider thyroid-marker levels as possible causes for poorer cognition among rural-dwelling women. The differential relationship between thyroid markers of TSH and FT4 with specific neuropsychological domains is intriguing and may be reflective of the differential site of production. It is possible that the link between TSH and attention is related to the integrated circuitry of the hypothalamic–pituitary–adrenal (HPA) axis, which has been strongly linked to attentional capacity, but not specifically to language. Why FT4 would be specifically related to language is unclear and requires further inquiry. The differential findings related to TSH and FT4 are important when evaluating elderly women with complaints of cognitive loss as deficits in attention and language are characteristic of different dementia syndromes.
Specifically, insidious language disturbances are oftentimes associated with Alzheimer's disease or other “cortical dementias,” whereas attention deficits are more frequently associated with “subcortical” dementia syndromes (see Lezak et al., 2003 for full review), which are also commonly associated with psychiatric disturbances such as depression. Therefore, a more thorough understanding of the complex relation between different markers of thyroid functioning and neuropsychological functioning is imperative for rural practitioners so as to have up-to-date best-practice guidelines for their elderly women patients.
There are limitations of this study. Because Project FRONTIER is in its initial stages, the data available for analysis were limited to 82 women; a larger sample size will allow for more fine-grained analyses. Recent research has demonstrated that subclinical hypothyroidism is an important diagnostic category to examine. Although the current sample size was not sufficient to conduct such analyses, they will be conducted in the future. Despite these limitations, the current study adds significantly to the existing literature regarding the link between thyroid levels and cognitive functioning among women. There is a deficiency of research examining the health of rural-dwelling women, and thus practitioners serving these populations rarely have the relevant research to inform their practice. Project FRONTIER was created to provide current research-based knowledge regarding the factors that influence health of rural-dwelling men and women. The current findings suggest that the relation between thyroid markers and cognitive status is complex and requires further study. As the sample grows, these and other analyses will be conducted to better understand how thyroid functioning affects neurocognitive status of rural-dwelling women.
Acknowledgments
The authors thank the entire research team, with special thanks to the people of Cochran County, as well as our Advisory Board, particularly Nancy Luper; without their help this project would not be possible. We thank Cochran County Memorial Hospital and its staff for all of their assistance and provision of office space. This work would not have been possible without the assistance of our community recruiters, Joel Torango and Bennie O'Brien. We offer special thanks to Dr. Yan Zhang and Erin Braddock for database management.
This study was funded in part by the National Academy of Neuropsychology.