General paresis (GP) is a clinical type of late-stage syphilis and neurosyphilis. Diagnosis of GP depends on clinical evaluation, serologic testing, and cerebrospinal fluid (CSF) examination. Clinical presentation of GP varies considerably among patients, and diagnosis may fall to the general physician, geriatrician, neurologist, psychiatrist, or venereologist. Clinical recognition of GP may be easy or difficult. There is no gold standard for its diagnosis at present, which often results in undue delayed diagnosis and causes serious consequences.
It is therefore necessary to investigate the clinical characteristics of GP in hope to improve its early diagnosis. For this purpose, we collected data on demographic characteristics, clinical neuropsychological, EEG, neuroradiological, serum, and CSF examination profiles of GP patients in several neurological units in the south of China.
DISCUSSION
GP is caused by syphilis infection; it is also known as paralytic dementia, Bayle's disease, parenchymal syphilis, and symptomatic neurosyphilis. It is a neuropsychiatric disorder affecting the brain and CNS, and typically presents as progressive dementia, beginning 15–20 years after original infection (range: 3–30 years).
Evidence shows that syphilis has become a major public health problem again in recent decades. From 1988 to 1995, a persistently growing number of new cases of syphilis in the world was observed.
2 In the United States, rates of primary and secondary syphilis again began to rise in 2001 after a decade of decline.
3 In San Francisco, the increased incidence of early syphilis has been accompanied by increasing rates of neurosyphilis,
4 and HIV infection also increases the risk of neurosyphilis.
5 Similar trends have also been observed in Canada and Europe.
6 In China, since the reform and opening-up policies of the early 1980s, STDs have been gradually recognized as public health problems, and the incidence of syphilis has increased steadily.
1 In 1993, the reported total rate of cases of sysphilis in China was 2 cases per million people, whereas primary and secondary syphilis were 57 cases per million people in 2005. The rate of congenital syphilis increased drastically, with an average yearly rise of 71.9%, from 0.1 per million live births in 1991 to 196.9 per million live births in 2005.
7 GP increased correspondingly after several years of incubation period; this is considered to be a “treatable” dementia because it can be treated with antibiotics, mainly penicillin.
8 However, early diagnosis and treatment are very important.
The diagnosis of GP could be differentiated from other known psychoses by characteristic abnormality in eye pupil reflexes, development of muscular reflex abnormalities, seizures, memory impairment (dementia), and other signs of relatively pervasive neurocerebral deterioration. Eventually, the patients became completely incapacitated, bedridden, and die, the process taking about 3-to-5 years, on average.
9–11 Clinicians need to recognize all the features of the clinical picture in order to correctly identify the GP patients at the early stage of the disease and design appropriate clinical treatments.
In our study, we found that neurosyphilis occurred more often in male than female patients, with a sex ratio of 8.67 to 1, which was higher than in previous reports.
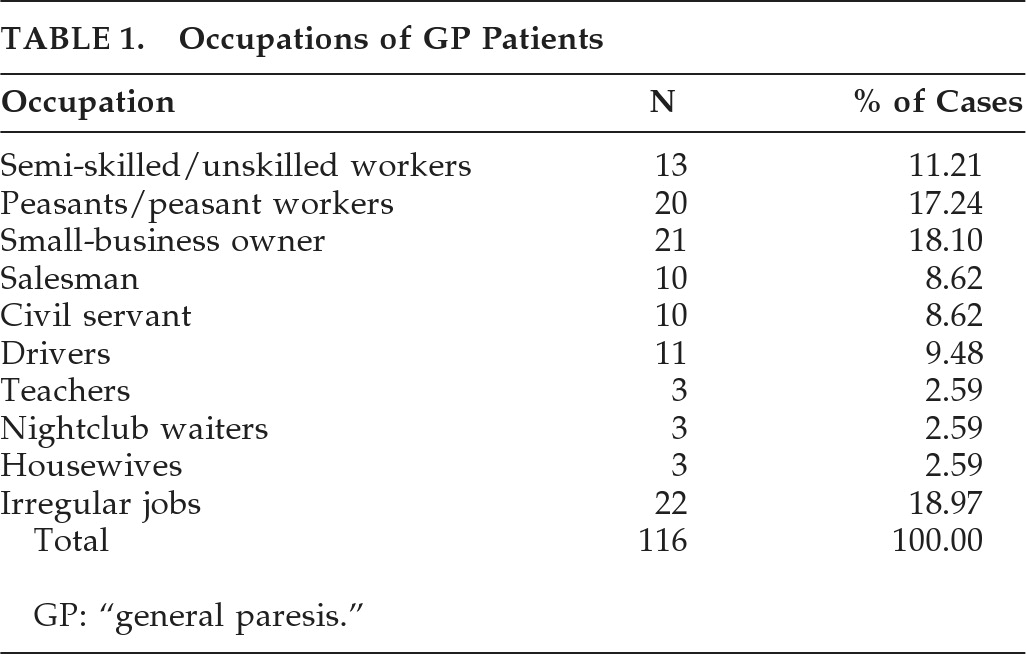
12 Furthermore, GP affected mainly young adult men, raising the question of whether it is due to an increasing incidence of homosexual behavior among men. About half of the patients had identified promiscuous sexual activity and/or history of frequenting prostitutes. The group suffering with GP were persons engaged in a variety of occupations. Among them, a large portion was mainly from lower social classes, including those with irregular work, nightclub waiters, low-skilled workers, poorly educated (junior middle school education or less), peasant or peasant workers, small-business owners, and laborers. It is worth noting that the analysis of social status revealed that some well-educated persons, such as teachers and civil servants, were also involved. This indicates that the prevalence of GP has extended to various social strata or classes, which is consistent with the report by Lin et al.
13 The prevalence of GP is a very serious issue now in China.
It has been reported that HIV infection has a strong epidemiological association with neurosyphilis. Analysis of cases with dual infection with Treponema pallidum and HIV indicated that HIV infection may accelerate the course of syphilis and that the presence of syphilis may also have an influence on progression of chronic HIV infection to AIDS.
5,14 Yet, in our study, no GP patients were simultaneously infected by HIV, maybe because of lower incidence of HIV infection in certain populations in China. Nevertheless, we strongly suggest that all of the patients with syphilis should be examined for the presence of HIV infection.
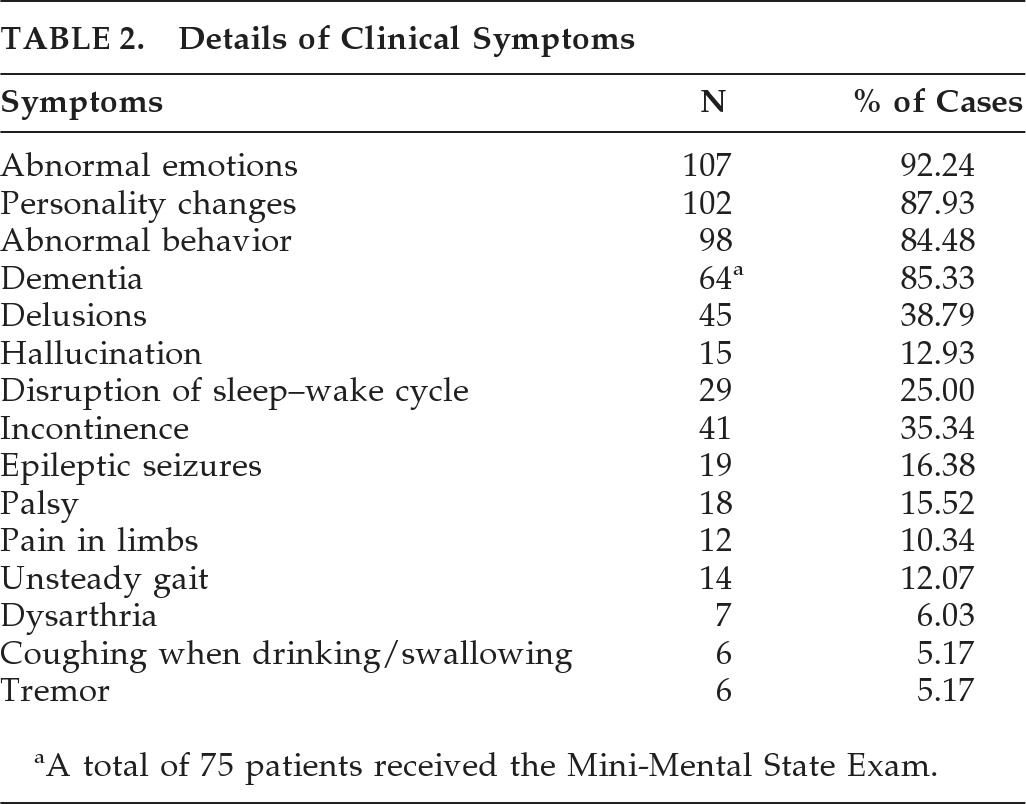
The most common symptom in our findings was emotional problems, followed by personality changes, different degrees of cognitive deterioration, abnormal behaviors, psychiatric symptoms, including delusions and hallucination, incontinence of feces and urine, dysrhythmia of the sleep–wake routine, and epileptic seizures. Other, lower incidence, symptoms, such as palsy, unsteady gait, coughing when drinking, dysarthria, and tremors, could also be observed in our study. Dawson-Butterworth and Heathcote
15 reported that the incidence of dementia in GP patients is about 60%–80%. It was 85.33% in our study. The incidence of personality changes and abnormal behavior were similar to those of dementia, reaching 87.93% and 84.48%, respectively, which were higher than their report. As for the incidence of emotional problems, in our report, it was 92.24%, which was much higher than the 17% reported by them. The reason may be that emotional problems are now being taken more seriously by neuropsychologists, and there are more precise neuropsychological scales now than there were then. Epileptic seizures and limb pain, which were seldom reported before, were 16.38% and 10.34%, respectively, in our study, indicating that clinical manifestation of the GP developed in a diversified forms and complicated ways.
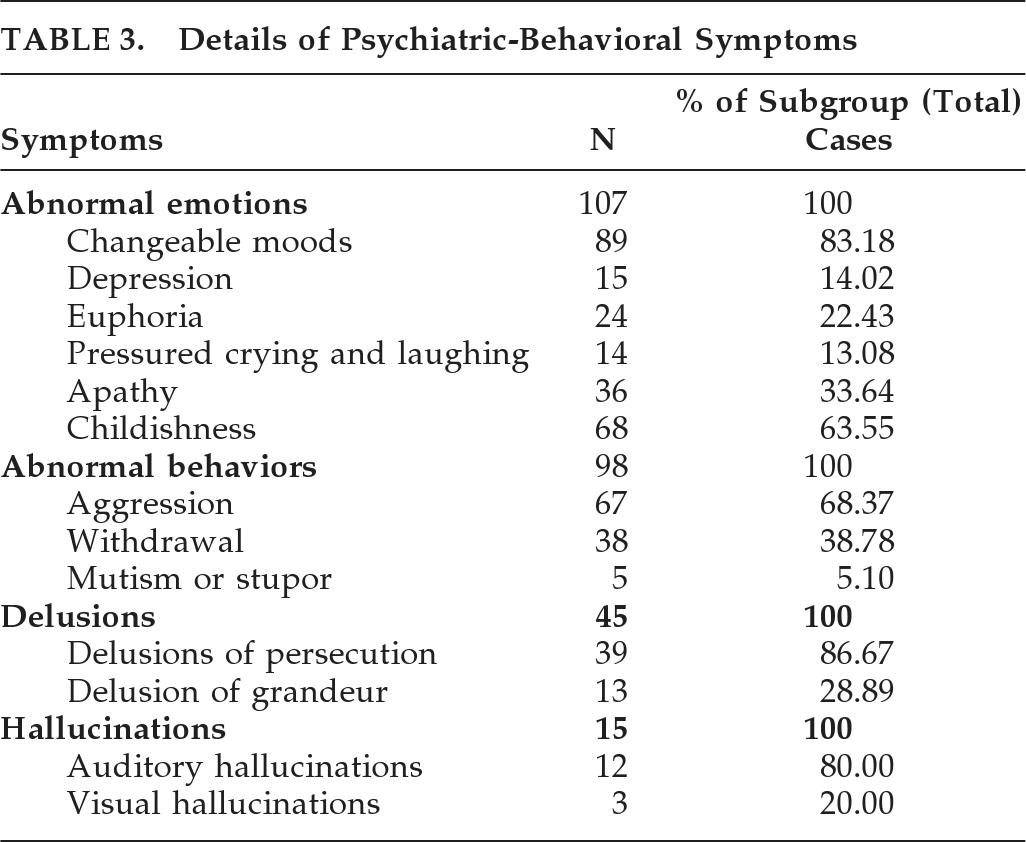
We further investigated the details of the common symptoms in those with psychosis. Changeable mood was the most common symptom and occurred in 83.18% of patients with emotional problems. The incidence of depression and euphoria tended to remain constant over the years, at 10% and 20.69%, respectively. Auditory hallucination was the most outstanding symptom in patients with hallucinations. Dewhurst
16 stated that grandiose delusion was not one of the most commonly presenting features of cerebral syphilis. He reported 10.9% for his patients; data from Chia and Tsoi
17 indicated it was 10%; Dawson-Butterworth and Heathcote
15 gave a figure of 9.3%; and our investigation was also in agreement and yielded 11.21%. It has been reported that men tended to be more aggressive than women on admission. Dawson-Butterworth and Heathcote reported that the total incidence is around 30%, and this uncontrolled behavior subsided with treatment, but tended to recur after a few years in the same proportions as before.
15 Chia and Tsoi
17 reported 44% of patients with aggressive behavior. In our study, there was a higher incidence of aggression; it reached 57.76%, which implies that GP patients might be potentially harmful to society.
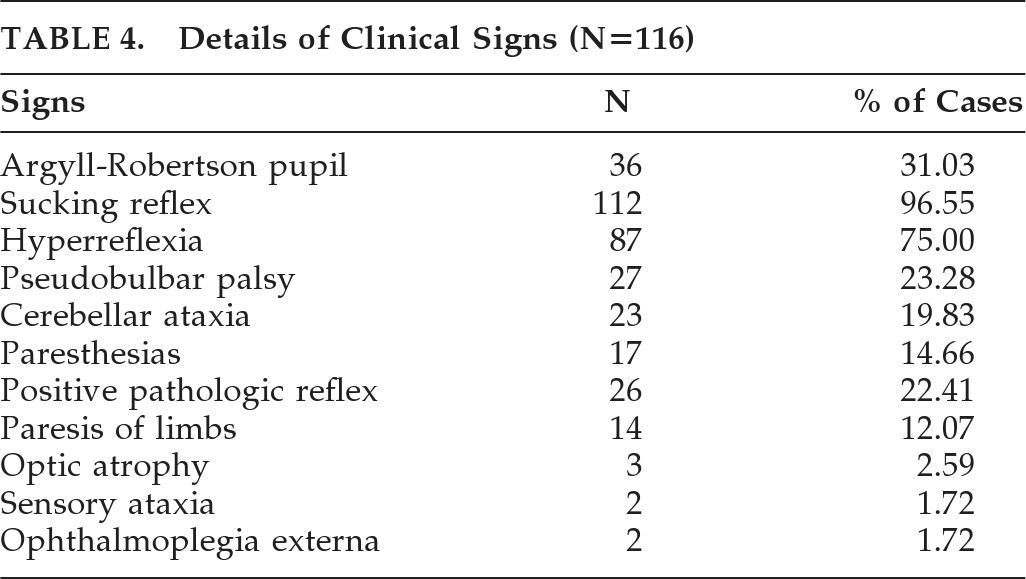
The most common sign, although seldom noticed by doctors, was positive sucking reflex. There were 112 cases in a total of 116 patients, which indicated severe damage to the frontal lobe, and is in accordance with patients' abnormal emotions and psychosis. Argyll-Robinson pupils are bilaterally small pupils that constrict when the patient focuses on a near object (they “accommodate”), but do not constrict when exposed to bright light (they do not “react” to light). Although the underlying pathophysiologic mechanism is unclear, research has implicated that the rostral midbrain in the vicinity of the sylvian aqueduct of the third ventricle might be the most likely region of damage. Argyll-Robinson pupil is an important and typical sign of neurosyphilis. The incidence here was 31.03%, slightly lower than the 35% reported by Dawson-Butterworth and Heathcote. The other clinical signs, such as tendon hyperreflexia, positive Babinski's sign, cerebellar ataxia, paresthesia, and optic atropy, were similar to those reported in recent literature.
15,16,18Results of EEG in most patients showed generic arrhythmic slow activity. Moderate or worse abnormal EEG activity and severe asymmetrical brain electrical activity were also detected. They are not specific, however, and can also be seen in other diseases. Anghinah et al.
19 reported two GP cases characterized by progressive cognitive impairment followed by partial complex seizures, for which the EEG showed generalized periodic activity like those appearing in Creutzfeldt-Jakob disease. Our data revealed single epileptiform discharge in five patients, yet no generalized periodic activity.
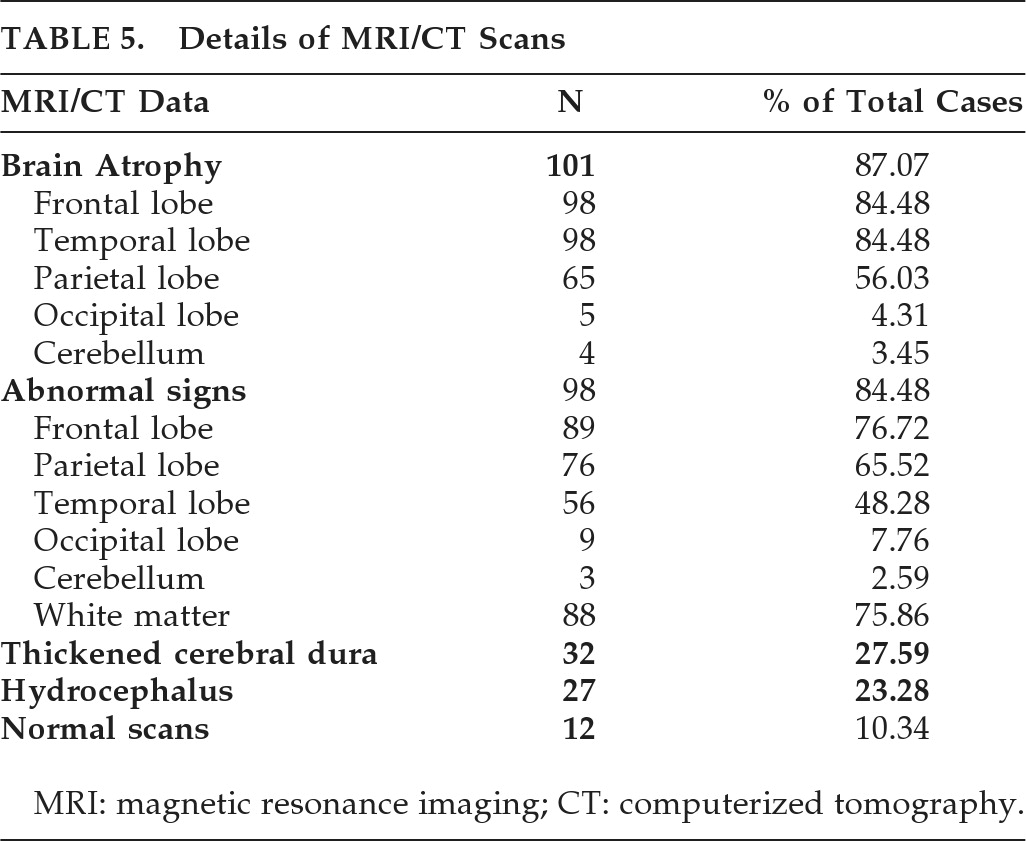
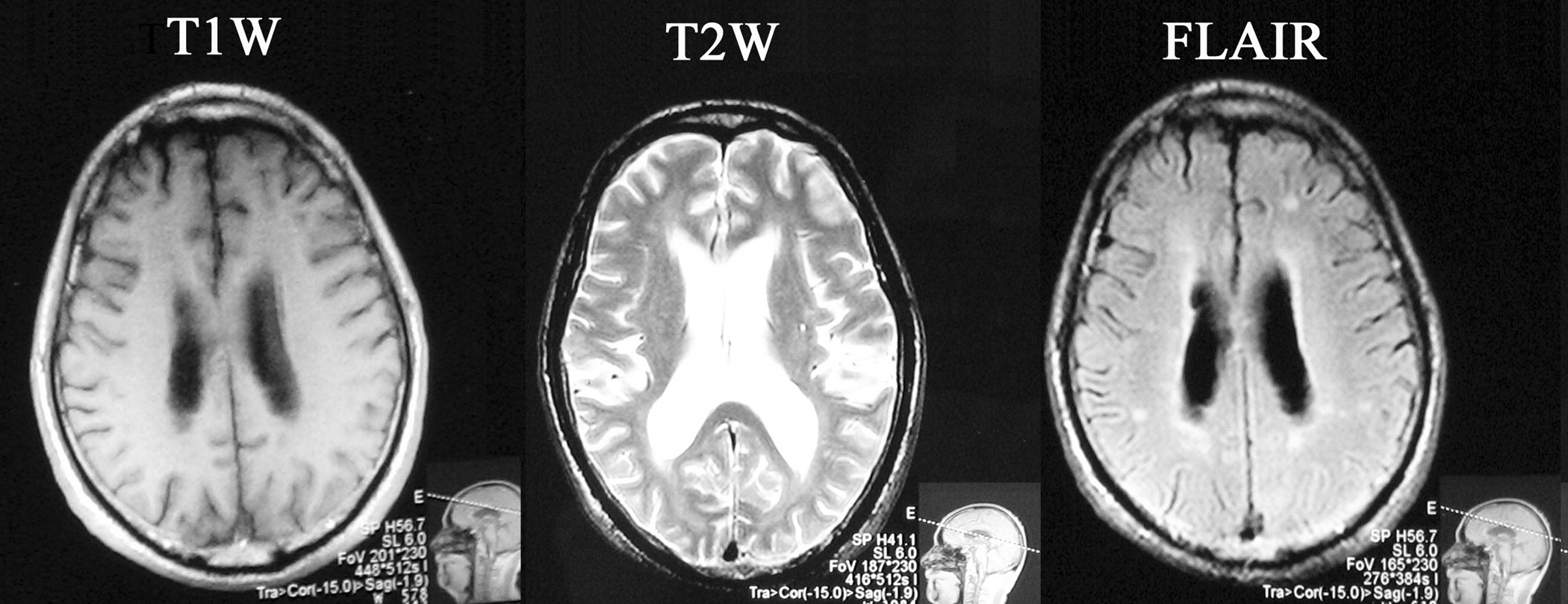
Neuroimaging of neurosyphilis generally is not very specific and thus is of limited value in making a diagnosis. Our MRI/CT finding in patients (
Figure 1) was mainly focal atrophy in one or multiple cerebral regions, especially in the frontal and temporal lobes, seldom in the occipital lobe and cerebellum, which was consistent with others' reports.
20 Kodama et al.
21 has suggested that MRI could be of prognostic value in patients with general paresis. They described severe atrophy, especially in the medial temporal lobe, which may be a poor prognostic sign in GP. For the purpose of verification, we may follow up these cases in a further study to observe their prognostic values. Single or multiple spotty or patchy lesions, mainly located in the cerebral cortex, subcortical white matter, and basal ganglia, with long T-1 and T-2 signal, were observed in 84.48% (98 patients). They were considered the result of insufficient blood to the brain caused by syphilitic cerebral vasculitis. Good and Jäger
22 reported diffusely enhancing meninges around the brain and spinal cord, and pointed out there might exist obstruction of the CSF. Our study found that more than 20% of patients suffered thickened cerebral dura mater and hydrocephalus. Cognitive deterioration, ataxia, and incontinence of feces and urine were the most common clinical manifestation in these cases.
As for syphilis pathogenic examination, positive blood TPHA and TRUST tests were seen in 100% of patients. For CSF samples, the positive rate of TPHA was 100%, whereas TRUST was 86.21%; statistical analysis indicated that TRUST was less sensitive than TPHA for CSF samples (p<0.05). There were also reports of negative TRUST values in the CSF of GP patients,
23,24 coinciding with our interpretation of the question.
GP has diverse clinical manifestations and can easily be misdiagnosed as schizophrenia, depression, and viral encephalitis. In elderly patients, it is especially likely to be misdiagnosed as vascular dementia. Our data showed that the rate of misdiagnosis was 36.21%, and the mean duration for the misdiagnosis lasted from 1 month to 24 months (mean: 8.2 [SD: 4.6] months). A similar finding has also been reported by others.
25,26