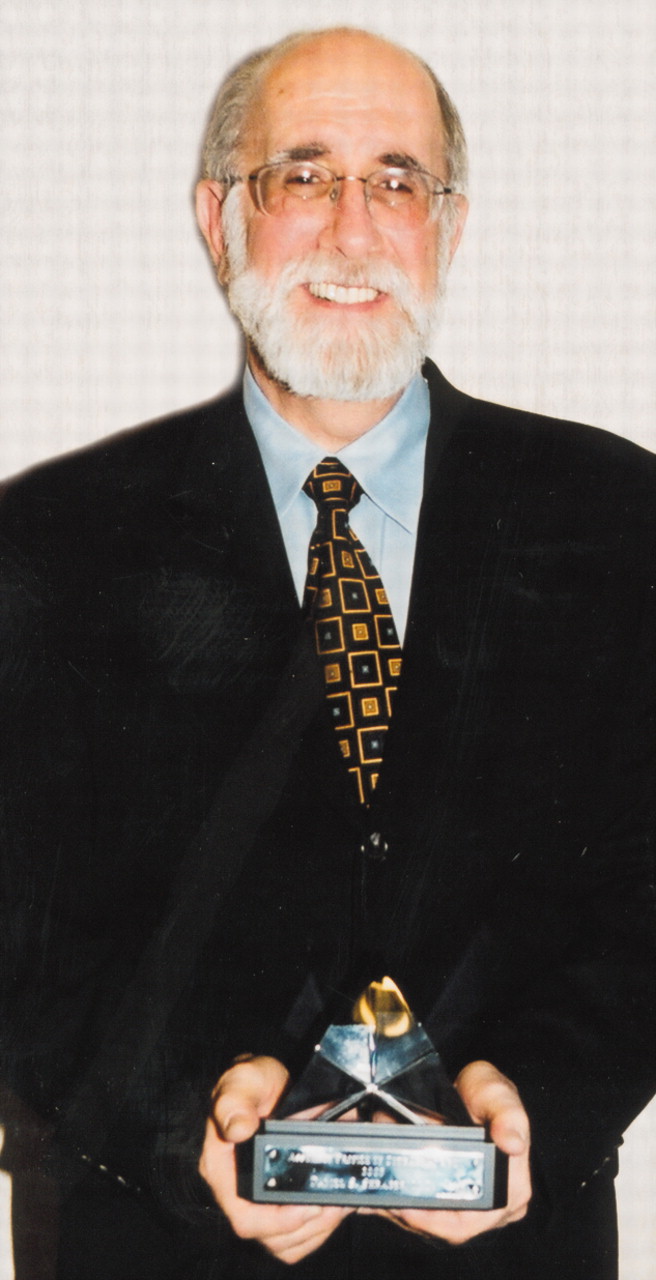
The APA Assembly honored two psychiatrists with its 2003 Profile of Courage Award, which recognizes psychiatrists who have taken financial or professional risks on behalf of patients with mental illness. This year’s awards went to former APA president Harold Eist, M.D., and Pittsburgh psychiatrist Daniel Shrager, M.D.
Eist was awarded for his battle with Maryland’s medical licensing board over its right to see a patient’s records when the patient refused to consent to such a record review. The board attempted, unsuccessfully, to revoke Eist’s license but did fine him and report him to the National Practitioner Data Bank. Eist took the board to court over its its demand for the patient records and its sanctions against him, where an administrative law judge ruled in his favor. The board then appealed this decision to a county court, which also ruled in Eist’s favor on almost all of the matters at issue. Eist’s financial penalty was canceled, and the board was told to revoke its report to the national data bank.
Shrager undertook an expensive battle against a mental health carveout firm that demanded the complete records of five patients whose care it managed for an insurer. It wanted the records as part of its recredentialing process. The company dropped him from its provider panel after Shrager refused to turn over the records without his patients’ authorization. Facing a substantial loss of income if he was dropped, he decided to sue the company. The court ruled in his favor, stating that he could edit the charts before turning them over, and said the company could not remove him from its provider roster. Shrager is appealing the ruling that he must turn over redacted versions of the records regardless of whether the patients agree.
APA contributed funds to help both psychiatrists defray the costs of their legal battles.
On one of the more controversial issues to confront the Assembly in quite a while, two district branches’ plans to open membership to or create a new affiliation for psychiatrists who would not have to join APA as well received a unanimous negative review from the Assembly Procedures Committee. The committee stated that the proposals would violate APA’s Bylaws. (The Assembly was not asked to vote on any issues related to the proposals at last month’s meeting.)
The plans revealed a sizable opinion rift among Assembly members after they heard the proposals described at last month’s meeting in Washington, D.C.
Texas Assembly representative Priscilla Ray, M.D., and Washington state representative George Vlahakis, M.D., described their respective district branch’s plan to implement an “affiliate” membership category in which psychiatrists could join the district branch without becoming APA members. The Bylaws of APA and all of its district branches require dual membership.
Ray indicated that Texas decided to proceed with the plan in the hope that it will increase the district branch’s declining membership. She added that the plan signals neither an intent to “de-link” or secede from APA nor “hostility” toward the national Association. Vlahakis explained that the Washington State Psychiatric Association (WSPA) does not see its plan as a “membership issue” because psychiatrists in the affiliate category will not be able to vote in district branch elections or hold office. WSPA leaders hope that affiliate members will eventually become full members, he added.
In the discussion that followed, some members spoke with empathy about trying strategies to stem the membership and revenue declines plaguing many district branches and did not express alarm about the plans’ potential for weakening or dividing APA. Early in the meeting, however, APA Medical Director James H. Scully Jr., M.D., pointed out that membership numbers appear to be stabilizing.
Opponents of the plans spoke more passionately than supporters did, emphasizing the need to avoid any actions that could dilute organized psychiatry’s voice or influence. One member, distressed over the proposals, cited contributions such as DSM and psychiatry’s decades-long exemption from Medicare’s diagnosis-related group payment system as examples of APA efforts that have benefited all psychiatrists, as well as their patients.
Area 4 Trustee Sidney Weissman, M.D., stressed that the most important issue at stake if APA and district branch membership are delinked is “the cohesion of organized psychiatry and the seamless link” between APA and its district branches—a link necessary if APA is to “effectively survive.”
Michael Hughes, M.D., of the Florida Psychiatric Society, encapsulated the views of many Assembly members when he stated that while there is empathy in Area 5 for the Texas and Washington state plans, he hoped they would come up with another solution to their membership concerns. Implementing these plans, he stated, would amount to “radical surgery” on APA.
APA leaders continue to talk with officers in both district branches about postponing or modifying their affiliate-membership plans.
The Assembly also reviewed more than a dozen action papers, voting to
• have APA request that members voluntarily indicate their sexual orientation any time it surveys members about demographic characteristics. APA already collects voluntary information on the demographics of its other categories of minority/underrepresented members. Several Area 7 representatives objected, maintaining that APA should not be collecting such private information and warning of “unintended consequences” regarding privacy violations. Marjorie Sved, M.D., representative of the Caucus of Lesbian, Gay, and Bisexual Psychiatrists, emphasized, however, that the members she represents are the ones who asked for such data to be gathered, and that APA does not release lists of any of its members according to demographic characteristics and this would be no exception.
• ask several APA components, including those concerned with ethics and education, to address the relationship between APA, individual psychiatrists, and the pharmaceutical industry, particularly its impact on the ethical practice of psychiatry, and to draft guidelines “for the psychiatrist-pharmaceutical [industry] interface within APA.”
• have APA “advocate for an industry-wide requirement that managed care organizations will collect and publish data reflecting actual access to psychiatric care” and develop model legislation legislatures can use “to ensure compliance with acceptable standards regarding access to care.” The estimated cost of the proposal is $197,000.
• defeat a proposal to explore whether APA should retire the term “seriously and persistently mentally ill” and replace it with “people with mental disability.” One of the authors, Roger Peele, M.D., of the Washington (D.C.) Psychiatric Society, maintained that use of the former term implies the existence of a population of psychiatric patients who aren’t seriously ill. Most Assembly members, however, appeared to agree with Michael Gales, M.D., of Southern California, who argued that “disability is a very general term that has a specific medical context and that changing [terminology] to disability could cause confusion” and even be “stigmatizing.”
• have APA consider supporting a change in the U.S. health care system based on the Combined Comprehensive Health Care Model, which is a “citizen/patient-owned and -directed health care system” that gives higher priority to the quality of health care services than to cost-containment.
• ask APA to establish a new corresponding committee composed of members from every state who have expertise in Medicaid issues. The committee would be able to facilitate and expedite information sharing between APA and district branches on the impact of budget cuts on the ability of Medicaid beneficiaries to access psychiatric care.
• urge APA to join the AMA and other groups in forcefully advocating for major changes in the way the federal government determines how much it will reimburse physicians for providing Medicare services.
• have the APA Task Force to Update Ethics Annotations revisit its blanket admonition about the ethics of psychiatrists discussing political advocacy with or soliciting research or clinical funds from patients, former patients, and patients’ families. The task force suggested that such practices by psychiatrists are unethical, but the Assembly unanimously agreed that “ethics are not immutable, but evolve with the changing spirit and needs of the times, place, and world views of a particular culture and prevailing socioeconomic factors.” The paper’s author, New York County representative Herbert Peyser, M.D., said that in the current economic and political climate in the United States, “it might be reasonable” for psychiatrists to, for example, urge patients to advocate for quality-care issues or for or against health-related budget proposals. The paper also noted that “it would not seem unethical to solicit a contribution to fund research from a patient who benefited from sophisticated specialty care based on the work of a particular investigator or clinician.”
• have the APA Committee on Psychiatric Diagnosis and Assessment discuss whether a criteria set should be developed for DSM that describes attention-deficit/hyperactivity disorder in adults.
The draft summary of the Assembly’s actions is posted in the “Members Corner” section of APA’s Web site at www.psych.org/members/index.cfm under “Assembly.” ▪