More than three-quarters (76 percent) of the U.S. population in 1999 had mental health benefits as a component of their health insurance plan, according to a report prepared by Mathematica Policy Research Inc. for the Substance Abuse and Mental Health Services Administration.
But that relatively positive finding is complicated by other factors, according to researchers Myles Maxfield, Lori Achman, and Anna Cook.
The generosity of mental health benefits, for example, is affected by whether their source is private or public insurance and by the laws in the state in which they are offered. In the case of employer-sponsored insurance, the generosity of benefits is related to the size of the firm offering them.
In “National Estimates of Mental Health Insurance Benefits,” researchers offer answers to such basic questions as these:
•
What is the source of mental health benefits? How generous are the mental health benefits for those who have them? How do the limits on benefits vary by source of insurance?
•
What proportion of the population falls under the jurisdiction of federal and state parity laws?
What Is Source of MH Benefits?
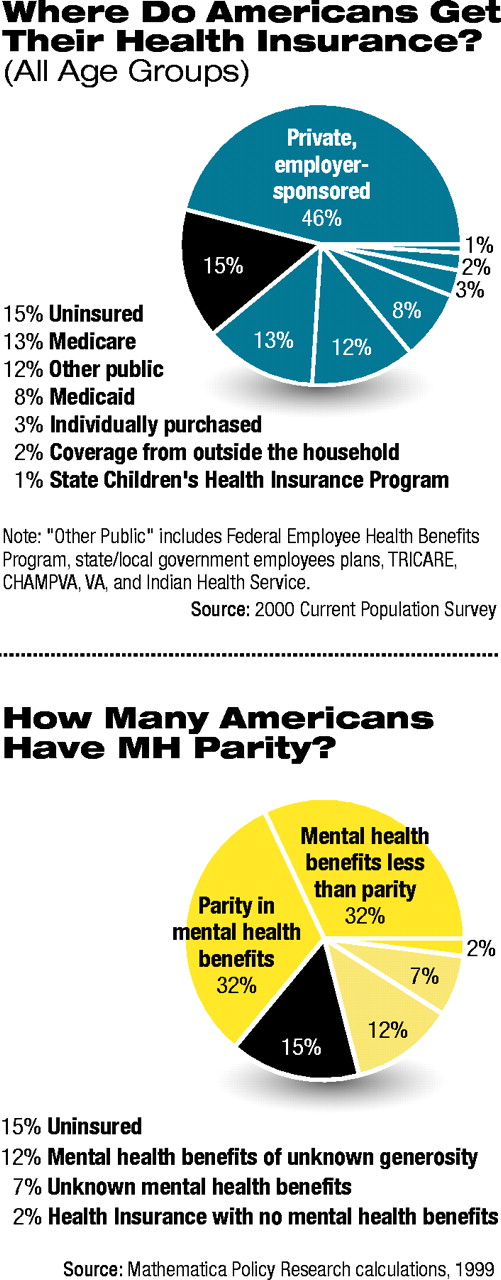
Mental health care benefits are offered through private and public insurance programs with varying degrees of generosity. The authors offered estimates of the source of primary health insurance in 1999 for those aged 0-17 years and 18-65 years.
Forty-six percent of those in the group aged 17 or younger had private, employer-sponsored health insurance. Other sources of coverage for that group and the percentage of those who had them were Medicaid, 17 percent; State Children's Health Insurance Program (SCHIP), 3 percent; Medicare, 1 percent; and other public insurance, 13 percent. Coverage from outside the household and individually purchased insurance each accounted for 3 percent. Eleven percent of individuals up to age 17 were uninsured.
For those 18 to 65, the figures are private, employer-sponsored health insurance, 53 percent; Medicaid, 5 percent; Medicare, 3 percent; and other public insurance, 14 percent. Individually purchased insurance was 4 percent, and coverage from outside the household was 2 percent. Nineteen percent of these people were uninsured.
The authors estimated that at least 90 percent of the U.S. population who had health insurance had mental health benefits as a component of that insurance, after comparing benefits offered through each type of insurance program with the number of individuals covered by it.
When the number of uninsured people was considered, the percentage of the U.S. population with mental health benefits dropped to 76 percent.
How Generous Are MH Benefits?
The authors defined “benchmark level of generosity” for mental health insurance benefits as coverage for 30 inpatient days, 20 outpatient visits, and prescription drugs.
Lawrence Lurie, M.D., chair of APA's Managed Care Committee, pointed out,“ We have to remember that these figures represent a maximum of what a person can receive. When these benefits are managed on the basis of `medical necessity,' the actual benefits available to patients might be much smaller.”
The authors noted that the level of benchmark coverage represents a level“ typical of many health plans” and not a “measure of plan adequacy.”
In 1999 approximately 59 percent of individuals with private, employer-sponsored health insurance provided through a firm with 10 or more employees had mental health coverage that met the benchmark. The authors do not have benchmark data on smaller firms, but noted that the likelihood of meeting the benchmark increased with firm size.
The authors categorized the traditional Medicare benefit as not meeting the benchmark because at the time of the study, Medicare did not provide prescription drug benefits. However, they estimated that 62 percent of Medicare beneficiaries had some prescription drug coverage through another source and, therefore, met the benchmark.
Children covered by Medicaid are eligible for services meeting the benchmark. Six states did not meet the benchmark because of utilization limits for adults, according to the authors. The authors noted that although payment for inpatient care in psychiatric hospitals is excluded by federal law, states provide inpatient psychiatric care in general hospitals.
Federal programs including the Federal Employees Health Benefits Program (FEHBP), TRICARE, Veterans Affairs (VA) health services, and the Civilian Health and Medical Program of the VA (CHAMPVA) met the benchmark.
Approximately 52 percent of individuals with health insurance had mental health benefits that met or exceeded the benchmark.
When the uninsured are included, that figure dropped to 44 percent of the U.S. population who had mental health benefits that met the benchmark.
What Is Extent of Parity?
The authors stipulated that full financial parity requires mental health benefits to be the same as medical and surgical benefits in terms of dollar limits, utilization limits, and cost-sharing requirements.
In 1999 approximately 14 percent of individuals with private, employer-sponsored health insurance provided through a firm with 10 or more employees had full parity in their mental health benefits.
As firm size increased, firms were less likely to provide parity in mental health benefits. The authors speculated that larger firms are more likely to be self-insured and thus not subject to state mental health parity laws because of the Employment Retirement Income Security Act (ERISA).
ERISA exempts self-insured employer-sponsored health plans from state regulations, thereby precluding the application of state parity laws. The authors estimated that nearly 49 million individuals—approximately 39 percent of the employer-sponsored health insurance market—were in self-insured plans.
In terms of public programs, Medicare does not provide parity. It requires 50 percent cost sharing by beneficiaries on essentially all outpatient mental health services as opposed to 20 percent for other outpatient services.
Medicaid meets parity requirements for children and adults, if one assumes that inpatient psychiatric care is provided in general hospitals.
In 1999 the FEHBP did not require that its participating plans meet standards for parity, but as of 2001 it did. VA and CHAMPVA health services met parity standards.
Federal Plan Changes
In 1999, 32 percent of individuals in the United States had parity in mental health benefits. An equal percentage had mental health benefits without parity. Twelve percent had benefits of unknown generosity, 7 percent had a plan whose mental health benefits were unknown, and 2 percent had health insurance with no mental health benefits. Fifteen percent of the population was uninsured (see chart on page 23).
Lurie said, “Questions of actual access for patients remain even if parity in benefits technically is provided. Strategies to manage care very frequently have followed the provision of parity in mental health benefits. Introduction of managed care means that psychiatrists receive low fees and are subjected to administrative hassles and late payments. As result, they are reluctant to accept patients whose benefits are managed.”
According to the 2002 National Survey of Psychiatric Patients conducted by the American Psychiatric Institute for Research and Education's Practice Research Network, 52 percent of responding psychiatrists were not on any managed care panels (Psychiatric News, March 19, 2003).
Study Being Conducted
The Department of Health and Human Services and the Office of Personnel Management have funded a study to evaluate the implementation and impact of the policy directive that required participating plans of the FEHBP, as of January 2001, to provide parity in mental health and substance abuse benefits.
Research study director Howard Goldman, M.D., Ph.D., said that final results are expected this fall.
Goldman is the editor of the APA journal Psychiatric Services and director of mental health policy studies and a professor of psychiatry at the University of Maryland School of Medicine.
The data sources for the study included the March 2000 Current Population Survey, the 1999 Medical Expenditure Survey-Insurance Component, and the Mercer Worldwide National Survey of Employer-Sponsored Health Plans. Each survey uses a nationally representative probability sample, with 1999 serving as the reference period for each survey.
“National Estimates of Mental Health Insurance Benefits” will be posted at<www.samhsa.gov> soon. ▪