Further efforts to contain the growing costs of Medicaid appear likely, according to an annual survey released in October by the Kaiser Commission on Medicaid and the Uninsured (KCMU).
“The Continuing Medicaid Budget Challenge: State Medicaid Spending Growth and Cost Containment in Fiscal Years 2004 and 2005” reported survey results showing that all 50 states and the District of Columbia implemented Medicaid cost-control strategies in Fiscal 2004, and all plan new actions for Fiscal 2005.
Health Management Associates conducted the survey for the KCMU in July and August 2004, at the end of most states' 2004 fiscal year.
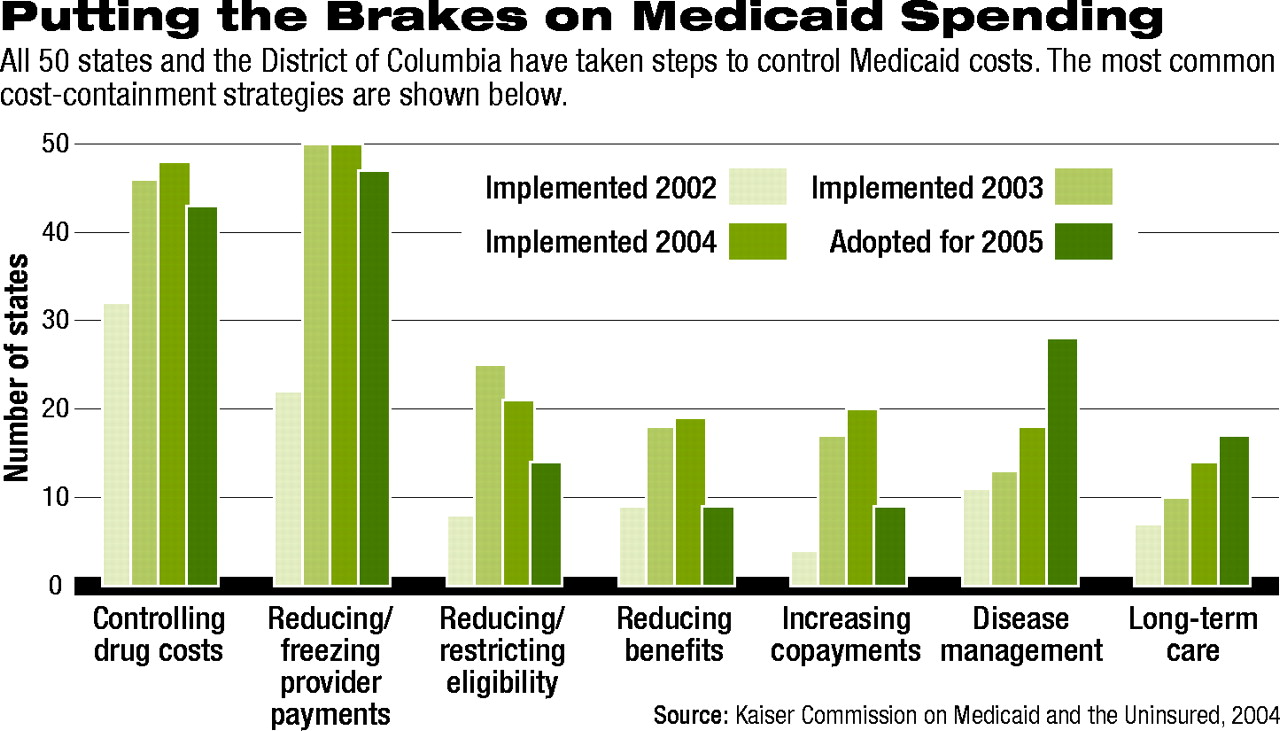
The most popular actions continue to be efforts aimed at controlling the costs of prescription drugs and freezing or reducing payments to those who provide medical services (see chart).
The KCMU hosted a briefing last month about that survey and a related report, “Beneath the Surface: Barriers Threaten to Slow Progress on Expanding Health Coverage of Children and Families.”
Diane Rowland, the KCMU's executive director, reminded the audience of key factors that have put pressure on states' Medicaid budgets.
“[There has been] a great increase in the number of people who are below the poverty level since 2000,” she said.
That increase is 5.6 million Americans, according to Rowland, with an increase of 2.1 million Americans in the “near poor” category.
Percentages of people who are uninsured are increasing, and those with employer-sponsored insurance are decreasing.
The report's lead author, Vernon Smith, Ph.D., emphasized the increasing importance of Medicaid in terms of health care delivery. He said it is the“ largest, single public health program in America today” and accounts for about 17 percent of all health care spending in the country.
“Medicaid [accounts for] a significant part of hospital spending and overall spending for physicians [and] plays a special role in long-term care, constituting about half of all spending for nursing home [care] and about 18 percent of all spending for prescription drugs.”
He added that Medicaid is the “largest single purchaser of prescription drugs in the country.”
Selby Jacobs, M.D., chair of APA's Committee on Public Financing of Psychiatric Services, told Psychiatric News that Medicaid appears to be of increasing importance to psychiatrists, as well as to the public mental health system.
He cited information from the New Freedom Commission on Mental Health that Medicaid is the largest payer of mental health services in the country.
Jacobs said that data analyzed by his committee for the period 1996-2002 showed a “slow, overall growth” of 14 percent to 17 percent in the percentage of psychiatrists' caseload paid for by Medicaid. Although that change is not statistically significant, subgroups of psychiatrists report Medicaid as a “substantial payer” of their caseload.
Perhaps even more important, said Jacobs, is the fact that Medicaid is of growing importance to psychiatrists who are out of residency less than a decade. That group showed an increase in the percentage of their caseload attributable to Medicaid from 17.7 percent to 24.7 percent during the years analyzed.
Medicaid is also an important payer for child psychiatrists and for those who work in clinics.
A report issued on October 13, after the KCMU briefing, by the National Association of State Budget Officers found that Medicaid costs increased more than any other area of state spending in Fiscal 2003 and are expected to consume a greater proportion of states' total spending than elementary and secondary education in Fiscal 2004.
The factors that account for the growth in expenditures suggest that this scenario is likely.
Smith said that Medicaid officials reported that spending growth was driven by “three key things:” enrollment growth, increasing costs of prescription drugs, and increasing costs of medical services in general. Costs related to each of those factors are increasing.
A new factor will be the impact on states' spending of the implementation of the new prescription drug benefit under Medicare. Under the new law, states will be required to pay the federal government for the drug costs associated with over six million low-income seniors who quality for both Medicaid and Medicare (dual eligibles). Their prescription drug coverage will be shifted from Medicaid to Medicare in 2006.
According to the KCMU-commissioned survey, more than three-quarters of states were concerned about the costs of this payment and the administrative burdens and other net costs they may occur due to the implementation of this benefit.
Health care advocates have challenged the most controversial methods to contain Medicaid costs.
At the end of September, Tennessee Gov. Phil Bredesen (D) sent the Centers for Medicare and Medicaid Services (CMS) his plan, which requires federal approval, to restrain costs by limiting doctor visits and other medical treatment and increasing copayments and premiums.
The plan also includes a definition of “medical necessity” that would require doctors to use “the least costly alternative” for a treatment that is “adequate” to the medical problem (Psychiatric News, August 20).
Jacobs said, “That definition is particularly troubling because it could undermine existing statutory protections for Medicaid patients. The weakening of those protections coupled with states' budgetary problems could result in real harm to them.”
Since the plan was first proposed, Bredesen has exempted children from some of the proposed restrictions, but not from the definition of medical necessity.
Forty-six national advocacy organizations, including the National Mental Health Association, the National Council for Community Behavioral Healthcare, and the American College of Obstetricians and Gynecologists, sent a letter to Bredesen in September pointing out dangers of his proposal, and they plan a letter to CMS.
In late September, the Mississippi Center for Justice, AARP Foundation Litigation, National Senior Citizens Law Center, and National Health Law Program filed a lawsuit challenging the state's elimination of Medicaid benefits for about 50,000 beneficiaries. In mid-October, a Mississippi judge granted a temporary injunction prohibiting the change until January 31, 2005.
“The Continuing Medicaid Budget Challenge” is posted at<www.kff.org/medicaid/kcmu100404nr.cfm>.▪