New positron emission tomography (PET) images of brain activity in patients in acute withdrawal from methamphetamine use show changes strikingly similar to those of patients with depressive and anxiety disorders. Researchers believe the new images offer biological evidence that mood symptoms must be assessed—and adequately treated—to treat methamphetamine abuse effectively.
“This is graphic biological evidence that mood disorder is a very important problem in acutely abstaining methamphetamine users,” lead author Edythe London, Ph.D., told Psychiatric News. London is a senior research scientist at the University of California at Los Angeles (UCLA) Neuropsychiatric Institute and a professor of psychiatry and pharmacology at the David Geffen School of Medicine at UCLA.
The research, funded by the National Institute on Drug Abuse (NIDA), appeared in the January Archives of General Psychiatry.
Should Depression Be Targeted?
“Treating methamphetamine addicts typically focuses on addressing drug craving,” London said. “These PET images pinpoint, for the first time, abnormal brain activity that is closely linked to symptoms of depression and anxiety. Targeting these complicating conditions as part of a more comprehensive treatment program may improve success rates for methamphetamine addiction therapy.”
London and her team used PET to examine glucose metabolism in seven brain areas known to regulate emotion, motivation, and behavior: the brain’s orbitofrontal, cingulate, lateral prefrontal, and insular cortices, as well as in the amygdala, striatum, and cerebellum. Each patient participating in the study underwent imaging and completed the Beck Depression Inventory to measure self-reported symptoms of depression and the State-Trait Anxiety Inventory to measure self-reported symptoms of anxiety. Seventeen methamphetamine abusers in an inpatient detoxification program were compared with 18 control subjects.
Mood Symptoms Reported
London found that the patients who were four to seven days out from their last use of methamphetamine gave significantly higher ratings of their symptoms of depression and anxiety compared with the control group. None of the patients met full diagnostic criteria for major depressive disorder, yet the depressive symptoms of the methamphetamine users were not minimal. The average BDI score for methamphetamine users was 9.5, compared with 1.1 for control subjects.
Anxiety scores were intriguing as well, London noted, showing significant increases for both state and trait anxiety in methamphetamine users compared with control subjects.
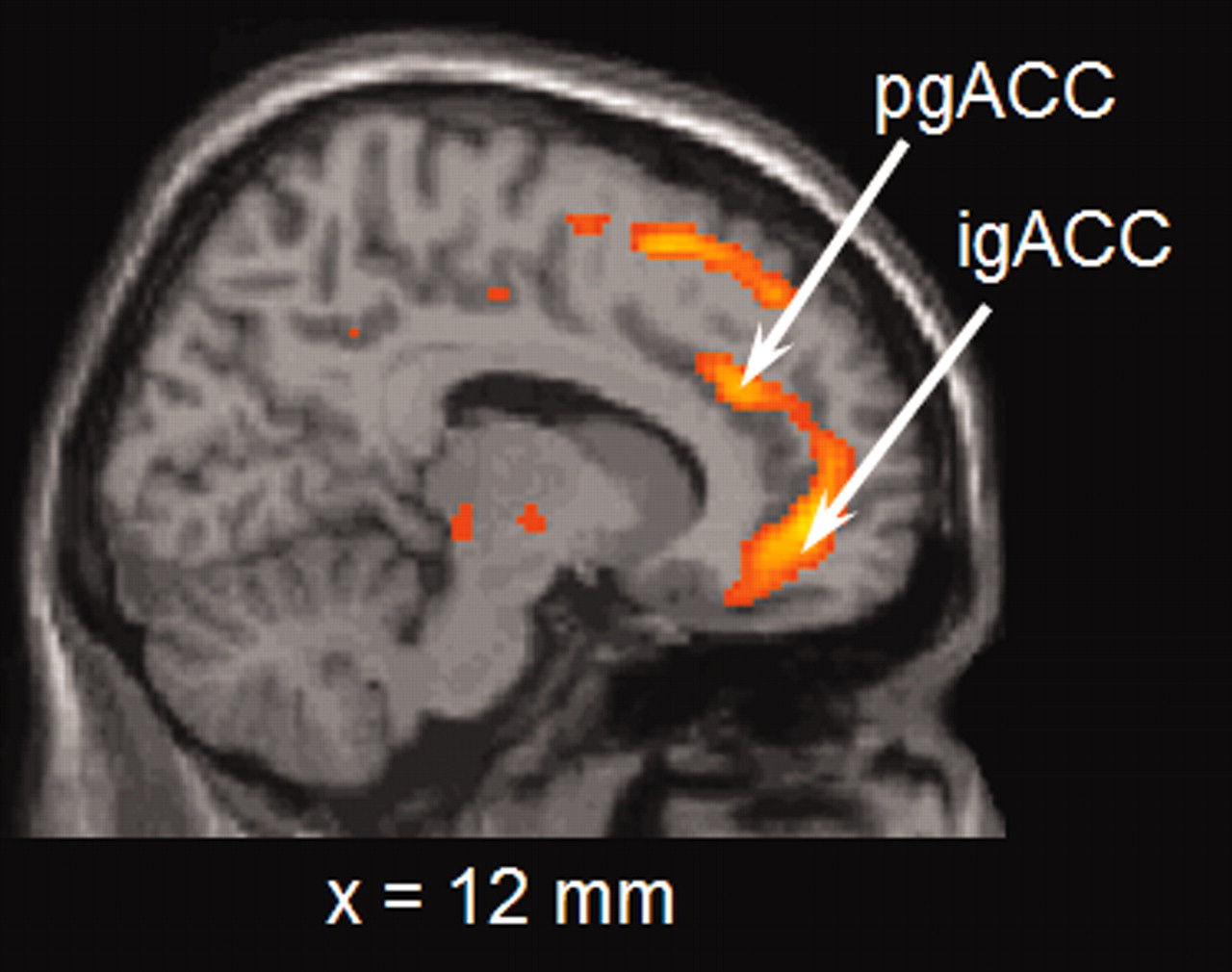
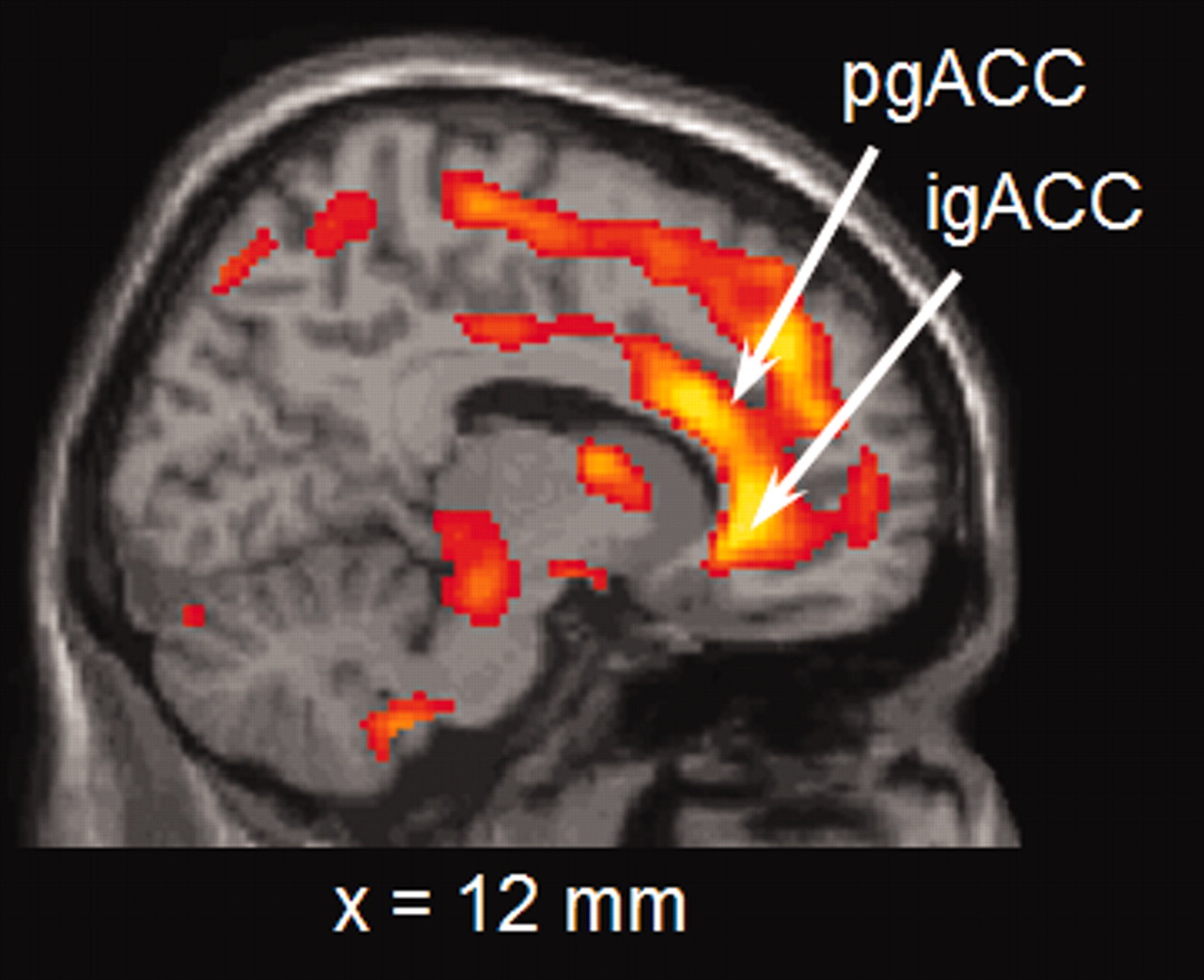
PET imaging of brain metabolism patterns clearly demonstrated differences between methamphetamine users and control subjects, particularly in the anterior cingulate gyrus and the insula (see images above).
Interestingly, London said, there was enough variation in brain metabolism of particular areas between the individuals who were in acute withdrawal from amphetamine to plot the relationship between activity of an individual brain region and self-reported symptoms of depression and anxiety.
“In fact, there were very strong relationships with activity in the limbic regions, such as the anterior cingulate and amygdala, and symptoms of depression, such that the higher the activity, the higher the depression score,” London said, “and there were also strong relationships between activity in the insula and anxiety, such that the lower the activity in the insula, the higher the state and trait anxiety measures.”
London described treatment of methamphetamine abusers as “kind of a moving target.” When a patient first comes into a treatment center or program, London said, “it is when they just ran out of money and cannot pay for their next hit. So they feel awful. But those mood and anxiety feelings will be different in three weeks, two months, one year than they are at intake. So one of the messages of this study is that when the methamphetamine user first presents for treatment, the mood disorder is a big, big problem that must be addressed.”
The mainstay of treatment for methamphetamine abuse has been cognitive-behavioral therapy, which London said is difficult if not impossible to begin at intake, because of the mood-disorder symptoms.
NIDA Director Nora Volkow, M.D., noted in a press release, “Currently, no medication exists to treat abuse or addiction to amphetamines or amphetamine-like compounds; however, drug counselors and other health professionals have successfully used behavioral interventions to treat addiction. Treatment outcomes may improve if associated mental conditions are addressed concurrently with addiction.”
The mood-disorder symptoms create an acute barrier to treatment, London told Psychiatric News. “CBT requires focused attention, learning, understanding, and self-control,” she explained, “all of which are difficult to accomplish if the mood disorder is not taken care of. [Patients] need to be told that. That acknowledgement [by treating clinicians] could be therapeutic in and of itself.”
London hopes to follow up the study with a look at how mood symptoms and brain activity change over time, as methamphetamine users go through a treatment program.
“Then we could define a therapeutic regimen that takes into consideration where the patient is at different stages of withdrawal.”