Antidepressant medications are associated with increased incidence of suicide attempts among youth because they are more likely to be prescribed to more severely ill patients—not because of the medications themselves, an innovative new analysis has determined. The analysis also found that other factors are associated with an increased risk of suicide.
The study analyzed claims data from a cohort of more than 24,000 adolescents diagnosed with major depressive disorder and tracked patients' treatment patterns and numerous factors that could influence patients to attempt suicide.
The analysis found an increased incidence of suicide attempts in adolescents treated with any antidepressnt medication, not just the serotonin reuptake inhibitors. However, the association was not statistically significant, and once the researchers controlled for other potentially confounding variables, the association disappeared.
“People tend to look at that initial crude association [between suicide and antidepressant medication] and say, `Well, it's higher for kids on medication, and therefore the drug made them do it,'” said Robert Valuck, Pharm.D., R.P.H., director of pharmaceutical outcomes research and an associate professor of pharmacy at the University of Colorado Health Sciences Center (UCHSC) in Denver. “But we tried to tease out as much as we could, controlling for as much as we could, and when we did, that initial relationship went away. The trend might still have been leaning [toward an association], but if anything, I think we were stepping on severity-of-illness markers.”
Valuck was first author on the report, which was published in the December CNS Drugs. The research was investigator initiated and funded.
“We had no outside funding for this, so no one was constraining us in any way as to how we had to look at the question,” Valuck noted.
“This is a very creative and methodologically rigorous analysis,” commented Darrel Regier, M.D., M.P.H., executive director of the American Psychiatric Institute for Research and Education and director of APA's Division of Research. “It goes beyond the observation that suicide attempts appeared to be higher among those on antidepressants by demonstrating that these same patients happen to have more severe disorders—a major reason why they were more likely to receive medication.”
Pursuing Novel Approach
Valuck and his team already had contracted for access to medical claims records from the PharMetrics Integrated Outcomes Database, a proprietary database of paid claims from 74 managed care plans nationwide, representing some 58 million covered individuals.
“We already had the database put together for some other depression-related research, and we had an open license to study whatever we wanted to study,” Valuck explained. The team had followed the U.K government's initial concerns regarding the use of antidepressants and suicide in teens in 2003 and began looking at a number of studies that used largely case-control approaches.
“We thought those studies had some limitations,” Valuck said.“ Those studies were informative, in their own way, but did not really get to the real question—which was, Do the drugs themselves increase the risk of suicide attempt?”
Rather than taking a case-control approach to the question, Valuck's group decided to use an incidence approach to look for any association between diagnosis, subsequent treatment patterns, and suicide attempt.
The group knew they would have to adjust for the lack of random assignment of the patients they were studying and the resulting potential bias. To address that inherent bias, the team created propensity or likelihood scores for each of the 24,119 adolescents identified in the database who had an index ICD-9 or -10 diagnosis of major depressive disorder or a prescription for antidepressant medication (or both) between January 1997 and March 2003. The availability of follow-up data ranged from at least six months to as long as six years, three months. Guidelines from the Centers for Disease Control and Prevention were used to identify individuals with a claim for a suicide attempt.
“We determined that, once diagnosed, each individual had a certain likelihood or not for being treated with an antidepressant. If a person was prescribed a drug, he or she had a certain likelihood for being prescribed a specific class of medication—an SSRI, a tricyclic, or multiple medications,” Valuck explained.
“The use of propensity analysis is quite sophisticated and state of the art for this kind of dataset,” noted Peter Jensen, M.D., the Ruane Professor of Child Psychiatry and director of the Center for the Advancement of Children's Mental Health at Columbia University and the New York State Psychiatric Institute.
Antidepressant treatment was coded only if there was a claim for a prescription filled within 30 days of the index diagnosis. Cases for which no antidepressant claims were found at any time after diagnosis served as the control group. Cases with claims for prescriptions filled more than 30 days after the index diagnosis were excluded.
The researchers also tracked separate measures of duration of medication therapy and patient compliance with therapy. Compliance was measured using a medication-possession ratio, equal to the total days of medication supplied divided by the time elapsed between the initial prescription and subsequent refills.
Of the 24,119 adolescents identified with an index diagnosis of major depression, 17,313 (71.8 percent) had no antidepressant prescription filled within six months of their diagnosis.
“We thought we'd see very much the opposite,” Anne Libby, Ph.D., an assistant professor of psychiatry at UCHSC, noted. “The data suggest the possibility of undertreatment in this cohort.”
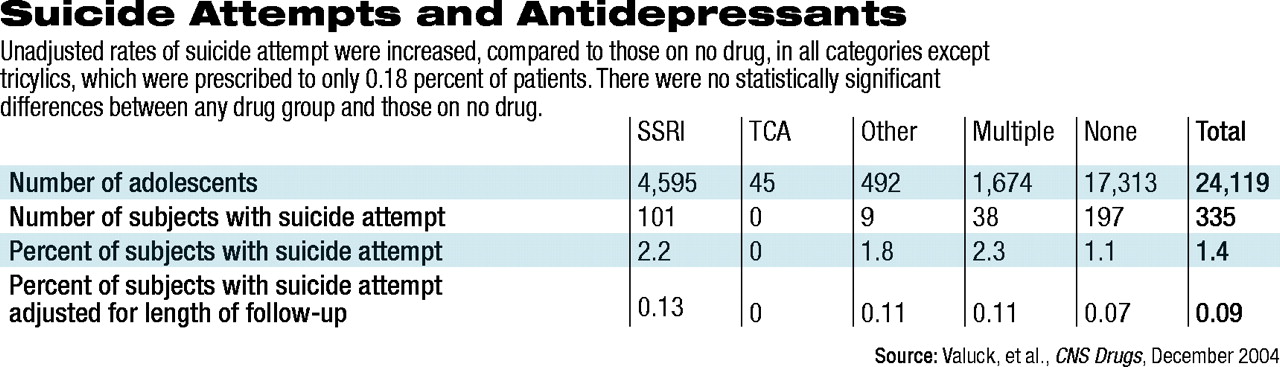
Of those on medication, the majority were on SSRIs, followed by multiple antidepressants, “other “antidepressants, and tricyclics (see table at top of page).
“It's important to note,” Valuck pointed out, “that this is not ideation, it's not contemplation. And it is not a measure of completion. These are events coded as suicide attempts.” The majority of these events were coded in emergency rooms.
Strikingly, rates of suicide attempt did not significantly differ between those on SSRIs, tricyclics, other, or multiple antidepressants. Particularly interesting, Valuck said, “was the association of suicide attempt with duration of medication therapy.
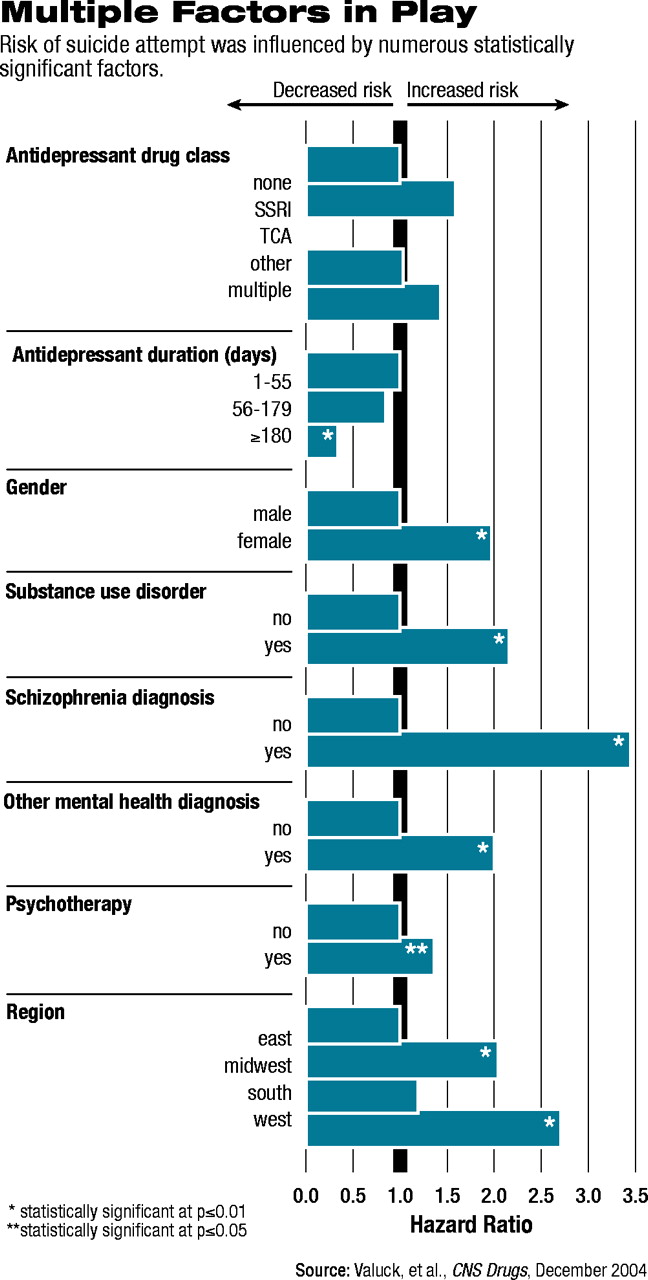
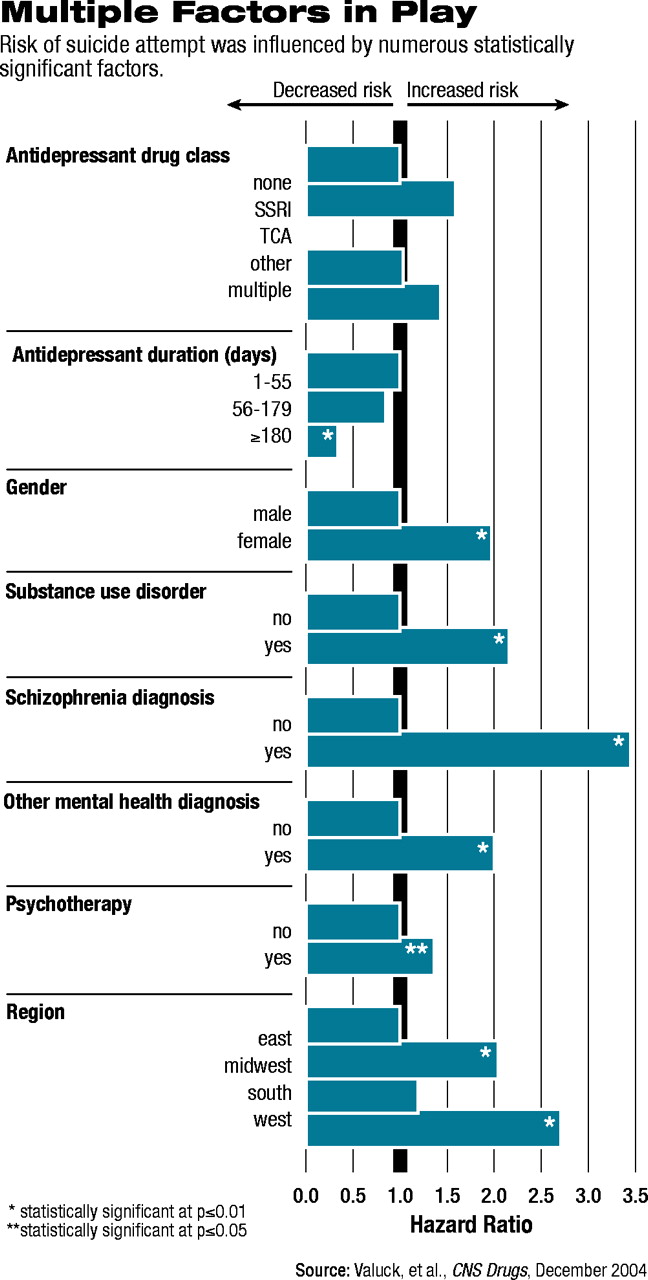
“[Suicide risk] was elevated during that initial short period, then the longer an individual stayed on medication, the lower the risk became, and it actually became, statistically significantly, a protective effect when you got out to the guideline-based marker of 180 days.”
Even after adjusting the dataset with the individually calculated propensity scores, several variables increased an adolescent's likelihood to attempt suicide (see table at left). Most notably, adolescents who had a comorbid diagnosis of schizophrenia had a 3.5 higher risk of attempting suicide; having any other psychiatric disorder, including substance abuse, doubled the risk.
Taking an SSRI increased the risk of attempting suicide by 59 percent, and taking multiple antidepressant medications raised the risk 43 percent; however, neither was statistically significant. Intriguingly, the presence of a claim for at least one psychotherapy session raised the risk by a statistically significant 36 percent.
Echoing earlier studies, the study found that, compared with adolescents living in the Eastern United States, adolescents living in the West were 2.7 times more likely to attempt suicide, while those in the Midwest were just over two times more likely.
Added Libby, “Simply put, those who were more severely ill were the ones who were most likely to attempt suicide. And they were the ones who were more likely to be on medication—or psychotherapy for that matter.”
Thus, Valuck summed up, if people believe that the medications themselves cause suicide, then logic dictates that “we should be out there advocating for pulling the licenses of all those therapists.”
Finding the Bottom Line
“We know that this is a very complicated issue, and there's lots of emotion along with political and financial influences,” said Libby.“ We wanted to go after a question like this because policy is being driven by it—but policy should never be based on one study or one point of view. We simply sought to contribute to the debate and provide whatever evidence we could to help narrow the focus.”
Valuck and his team have submitted grant applications to look at the data in more detail. “It would be very interesting to look at to what extent provider type mattered, or what insurance plan type, copayment type, and so on mattered,” he said, “and how each of those affect a youth's ability to initiate treatment and then stay in treatment.”
The team has also submitted research proposals to track the effects of the black-box warnings and whether and how the warnings are changing treatment patterns and outcomes in adolescent depression.
“It's a critical issue,” said Valuck. If the drugs' use in youth is restricted unnecessarily, “we could end up inducing problems over the long run.”
APA's Regier concluded, “This type of analysis is much more compelling than the FDA's analysis of self-reported suicidal ideation or attempts, which ignored the more systematic assessment data that showed a reduction of symptoms with treatment. Media reports of the FDA hearings have left the public with the impression that antidepressants cause suicidal symptoms and missed the big picture that depression causes these symptoms, as well as the finding, as supported by this study, that these medications need to be part of a careful treatment and monitoring plan that will reduce the overall risk of suicide.”
An abstract of “Antidepressant Treatment and Risk of Suicide Attempt by Adolescents With Major Depressive Disorder: A Propensity Adjusted Retrospective Cohort Study,” is posted online at<www.ingentaconnect.com/content/adis/cns/2004/00000018/00000015/art00006>.▪