Researchers at the Mayo Clinic in Rochester, Minn., have developed a brain-imaging technique that could prove to be a potential diagnostic tool for bipolar disorder. Preliminary data, presented last month at the annual meeting of the Radiological Society of North America in Chicago, identified differences in the brains of patients with bipolar disorder, compared with those of control subjects.
The research team, led by John Port, M.D., Ph.D., an assistant professor of radiology at Mayo, used magnetic resonance spectroscopic imaging (MRSI), a form of magnetic resonance imaging that allows clinicians to image not only anatomical structures, but also physiologic functions.
Funded by the Research and Education Foundation, Port has submitted the work to a peer-reviewed radiology journal.
“Anatomical imaging has truly failed to help out psychiatry,” Port told Psychiatric News. “Structurally, the brains of psychiatric patients and `normal' patients are largely indistinguishable—you simply cannot reliably image the differences.” Port noted that several studies have found small differences, but there has been no consistent trend that has pointed to a future diagnostic tool.
“People have often said over the years that psychiatric illness is a `chemical imbalance,' and while maybe not the best description, the phrase does point out the problem—mental illness isn't something you see on a scan.”
Previous MRSI studies of patients with mental illness have been plagued by two “fatal flaws,” Port said, which made the search for reliable findings analogous to looking for the proverbial needle in a haystack. First, earlier studies used metabolite ratios comparing two different physiological byproducts in the brain. However, Port pointed out, if the ratio is different in a patient with mental illness, what exactly is different—did the top half of the ratio change, or did the bottom? Using ratios simply doesn't answer that question.
Second, most earlier studies were limited to images of a relatively small amount of brain tissue.
“In previous studies they would look at areas [within the brain] that were thought to be involved in bipolar disorder, for example, yet what if the abnormality they were looking for actually occurs somewhere else—somewhere they didn't look? The studies were subject to sampling error,” Port said.
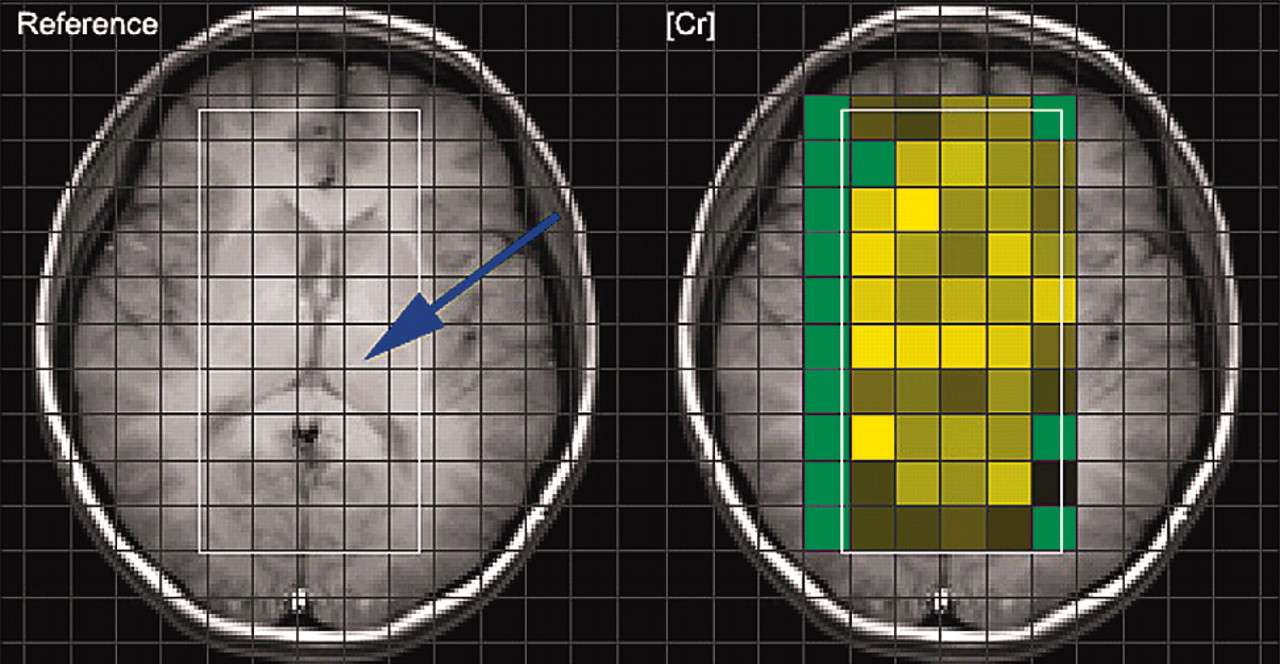
Port and his team set out to avoid these “fatal flaws.” His group measured actual brain metabolite concentrations, not just ratios of metabolites, and they did so using a technique developed by researchers at King's College in London that allows the collection of hundreds of voxels at a time, rather than the one or two voxels commonly imaged in previous studies. (A voxel is a unit of volume of tissue imaged during a scan.) In addition, the Mayo group used a “three tesla machine,” a magnetic resonance scanner with the strongest magnet currently available and nearly twice as strong as that used in previous studies.
“That allowed us to get the information we needed in about half the time,” Port explained, adding that minimizing the time that patients with bipolar disorder were required to spend in the scanner was a “real plus.”
“The fourth piece that makes our study really unique is that we recruited only drugnaïve
“Anatomical imaging has truly failed to help out psychiatry.”
patients,” Port added, “many of the previous studies were done with patients on a wide array of medications, which of course is a serious potential confounding variable.”
Port and his team scanned the brains of 21 adults with bipolar disorder who had either never been on medication (having been newly diagnosed, for example) or had not taken any psychiatric medication for at least the eight weeks prior to the scans. They also scanned the brains of 21 volunteer adults who had no psychiatric history. The control subjects were matched by age, sex, and handedness. Study participants ranged in age from 18 to 54; there were 26 women and 16 men.
The researchers scanned between 60 and 70 regions of the brain at a time, gathering thousands of data points. That allowed them to analyze 14 areas of the brain for differences in four major brain metabolites: myoinositol, creatine, choline, and N-acetylaspartate (NAA).
“What we found was that in patients with bipolar—whether it was bipolar I, II, or NOS—and in any mood state... two specific brain regions and four metabolites were statistically significantly different between the normal control subjects and the bipolar patients.”
Specifically, myoinositol concentrations were significantly higher in the right frontal white matter of bipolar patients, compared with control subjects. In addition, both creatine and NAA were significantly lower in the right lentiform of bipolar patients, compared with normal control subjects.
“But after the initial differences were seen, we wanted to know whether the subtype of the disorder—bipolar I, II, or NOS—made any difference,” Port explained. “Would we be able to distinguish between them?”
The team's analysis revealed that bipolar I patients had significant differences in brain metabolites, compared with bipolar II or NOS patients.
“What that tells us is that bipolar I seems to indeed be a different disease than bipolar II or NOS,” Port said. “We looked at left caudate choline levels, right parietal white-matter choline, and NAA levels, and the bipolar I patients had the largest differences in metabolite concentrations compared with the control subjects. It makes sense—it fits with the clinical picture. Bipolar I is clinically the more severe form of the disorder.”
Finally, Port said, the team looked for differences in metabolite concentrations tied to the patients' mood state when they were scanned.
“The most significant differences were seen between bipolar patients in a mood state—manic or depressed—and those who were euthymic,” Port said. “Again we found different concentrations of different metabolites, which reinforces that these abnormalities correspond to mood states—a fingerprint for mood state, if you will.”
Intriguingly, he noted, they found little difference between patients who were depressed and those who were manic, but both polar states were different from those in subjects who were in a normal mood state.
The team is continuing to refine the technique, and Port plans to submit a grant proposal to the National Institute of Mental Health for funding to study the technique in a larger, well-controlled population.
“What I'd really like to look at is patients who have bipolar disorder and compare those with both a normal, healthy control population and a group of patients with major depression,” Port said. “That way, we could see if we can tease apart bipolar from major depression.”
“Most diseases you can diagnose with a blood test, a scan, something tangible,” he noted. “That has been elusive in psychiatry. Hopefully this represents progress on that front.”
More information on Port's work is posted online at<www.rsna.org/rsna/media/pr2004/pr_bipolar.html>.▪