Medicaid grew to be the largest payer of mental health care during the period 1991-2001, with prescription drugs the fastest growing spending component.
That's what a team of public- and private-sector researchers reported in a study published on the Web site of the journal Health Affairs on March 29.
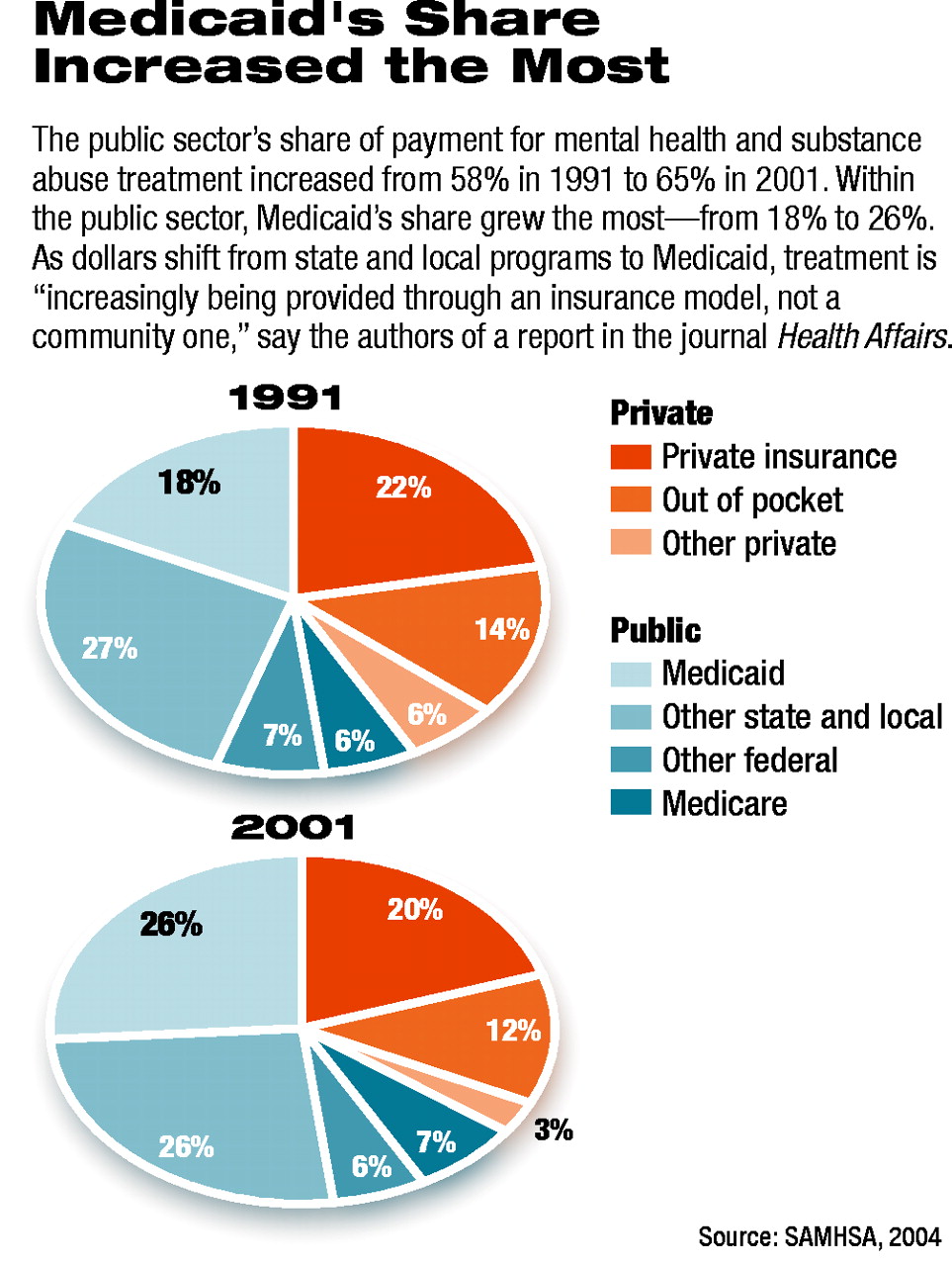
Public payers accounted for 63 percent of total spending on mental health treatment and 76 percent of substance abuse treatment in 2001. This compares with 57 percent of mental health treatment spending and 62 percent of substance abuse treatment spending in 1991, according to Tami Mark, Ph.D., associate director for outcomes research and econometrics at Medstat, and colleagues.
Medstat, headquartered in Ann Arbor, Mich., provides market intelligence and research services for managing health care costs and quality. The co-authors of the Health Affairs study included Rita Vandivort-Warren, Ph.D., a senior policy analyst at the Center for Substance Abuse Treatment of the Substance Abuse and Mental Health Services Administration (SAMHSA).
In 2001 personal health care expenditures in the United States were more than $1.3 trillion, of which mental health and substance abuse (MHSA) accounted for about 7.6 percent, or roughly $104 billion. Of total MHSA spending, $85 billion (82 percent) was for mental health, and $18 billion (18 percent) was for substance abuse.
Private payers accounted for 35 percent of total MHSA spending in 2001, while public payers accounted for 65 percent. Among public payers, Medicaid paid for 26 percent of total MHSA spending, other state and local governments paid for 26 percent, Medicare accounted for 7 percent, and other federal government payers such as block grants and Veterans Affairs accounted for 6 percent.
“As dollars shift toward Medicaid and away from state and local programs, care for disabled and low-income mentally ill is increasingly being provided through an insurance model, not a community model,” the authors wrote. “More attention needs to be paid to this trend and its consequences, including efforts on areas such as the organization of state government agencies, data systems and performance measurement, and coordination across programs and providers.”
In the study, Mark and colleagues used two methods to estimate MHSA treatment spending. The first method relied on SAMHSA's national surveys of specialty MHSA organizations: the Survey of Mental Health Organizations and the National Survey of Substance Abuse Treatment Services. The second method relied on data from the Centers for Medicaid and Medicare Services.
Data from the two methods were integrated by adding spending by provider and payer after accounting for duplication across data sources.
“Mental disorders” were defined according to diagnostic codes in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).
The study also documents a remarkable shift in spending away from inpatient hospital care to retail prescription drugs. Between 1991 and 2001, inpatient spending on all types of providers reporting inpatient services declined from 40 percent to just 24 percent of MHSA spending. Spending on retail prescription drugs increased from 6 percent of total MHSA spending in 1991 to 17 percent in 2001, according to the report.
The researchers found that the largest category of prescription medications was antidepressants, which accounted for more than half of MHSA drug spending in the study period. Antipsychotics accounted for 22 percent of MHSA drug spending, antianxiety drugs accounted for 13 percent, and other MHSA drugs accounted for 12 percent.
“This period was the Decade of the Brain, but also coincidentally the decade of managed care,” commented Steven Sharfstein, M.D., APA president-elect and president and chief executive officer of the Sheppard Pratt Health System in Maryland.
“It's very clear from this report what a profound impact the mental and behavioral health carveout industry has had on inpatient psychiatric care and on the shift of patients who are seriously ill from private payers to public payers. These national data demonstrate fairly dramatically what we knew was happening locally.”
He added that psychiatry is especially vulnerable to the persistent fiscal pressures that are exerted on publicly funded, tax-supported programs such as Medicaid.
“As those programs are cut, our patients are disproportionately hurt,” he said. “This means that for kids with serious emotional disturbances who are difficult to manage and for adults who have treatment-resistant psychotic illness, it is much more difficult to find funding for what is more and more widely acknowledged as effective treatment.”
Sharfstein said the shift to spending on pharmaceuticals is a broad trend that has affected all of medicine, but has been especially noteworthy in the field of mental health and substance abuse.
“This trend has been reinforced by managed care, where there has been an effort to use pills at the expense of time-intensive psychotherapy,” he said.
Sharfstein added that the trends described in the Health Affairs report demand continued monitoring, noting that there is some evidence that the shift from private to public funding for MHSA may be slowing or reversing. He also emphasized the importance of APA's business initiative, an effort begun by the Association in 1999 to increase awareness among businesses about their role in providing effective treatment for workers with mental illness and substance abuse.