Terri M. was a “terrific young girl” with a perfectionist personality who developed early symptoms of exercising anorexia nervosa at age 8. Three years later, she had full-blown anorexia, Joel Yager, M.D., a professor of psychiatry at the University of New Mexico and an eating disorder authority, recalled in an interview with Psychiatric News.
“Her mother had also had the disorder in college,” Yager added.“ Both her mother and father are thin, high-achieving compulsive athletes to this day, as are all of their friends.”
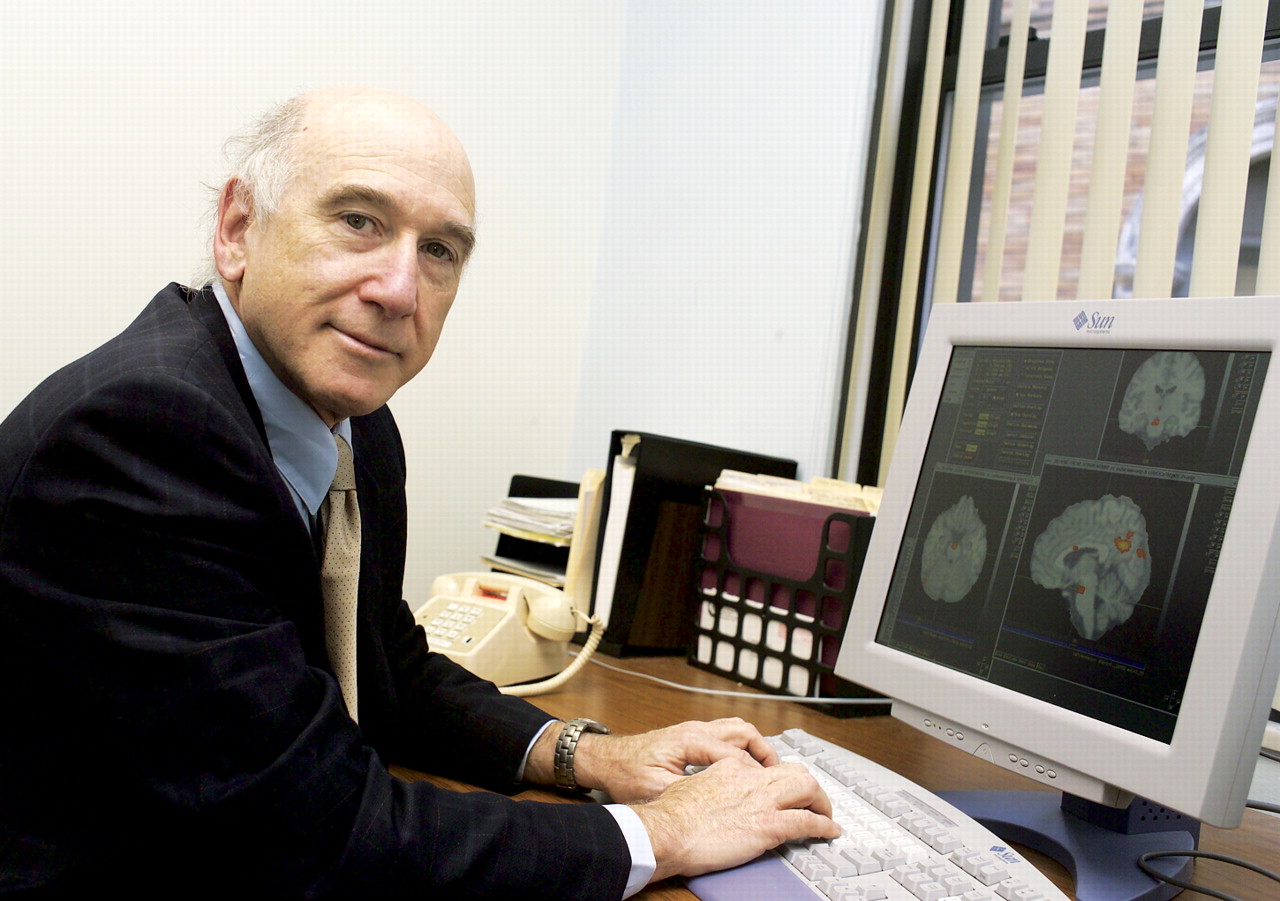
Can Terri's anorexia nervosa be blamed on genes? The influence of her parents? Or other factors? Probably all three, research results suggest,“ although genes play a much stronger role in anorexia nervosa than initially thought,” Walter Kaye, M.D., a professor of psychiatry at the University of Pittsburgh and an anorexia expert, told Psychiatric News.
Nonetheless, there are still a number of puzzling questions about the origins of anorexia nervosa, a condition that has been medically recognized since the late 19th century. In fact, a lot still remains to be learned not just about the sources of anorexia nervosa, but also about those of the two other recognized eating maladies— bulimia nervosa, first identified in 1979 and included in DSM-III, and binge-eating disorder, included in the DSM-IV as a provisional disorder.
For instance, ample evidence has revealed that eating disorders occur predominantly in developed countries, prompting eating-disorder experts to suspect that certain cultural or social factors in developed countries are at least partially responsible for the illnesses. Yet little research has divulged which cultural or social factors might be the culprits.
Moreover, there are no firm data about the prevalence of eating disorders in the United States and thus no way of knowing whether the prevalence of eating disorders has changed in recent years.
“I wish we had such data,” said David Herzog, M.D., a professor of psychiatry at Harvard Medical School and an eating disorder authority.“ It is a limitation in our field.”
In fact, it is not even known whether more Americans are seeking treatment for eating disorders today than five or 10 years ago. “I am not aware of any data to show changing trends in help-seeking behavior,” said Yager.“ This is very complex and has to do with changing awareness—which might increase help-seeking behavior—and issues concerning access to care, both availability of trained specialists and insurance or other means to pay for care.”
Better Treatments Available Today
The good news, however, is that there are more ways to help individuals with eating disorders today than there were 20 years ago.
For instance, there is strong evidence to support the value of family involvement in the treatment of anorexia nervosa patients under the age of 18. It is also now known that after anorexia nervosa patients have regained weight—with the help of families and/or with the help of staff in eating disorders programs—that the risk of relapse can be reduced with psychotherapy, particularly cognitive-behavioral therapy (CBT), and with fluoxetine, and presumably other SSRI antidepressants as well, said Yager.
The treatment of choice for bulimia nervosa is CBT, whose effectiveness is now supported by more than a dozen studies. Scientific evidence has also revealed that if bulimia nervosa patients are treated with both CBT and an SSRI, they do even better than if they get CBT alone, Yager said.
As for binge-eating disorder, CBT is quite successful is halting the binging, but it is not so effective in helping people achieve a healthy weight over the long term, according to James Mitchell, M.D., president of the Neuropsychiatric Research Institute at the University of North Dakota.
Other Therapies in Offing
Still other effective therapies for eating disorders may become available soon as scientists make inroads in understanding the illnesses.
A case in point: Kaye and his coworkers recently found that two types of dopamine receptors—D2 and D3—are more active in the basal ganglia area of the brains of anorexia nervosa subjects than in the basal ganglia area of the brains of subjects who don't have the illness. The researchers also found that the gene that makes the D2 receptors is abnormal in some anorexia nervosa subjects. Kaye and his group thus suspect that dopamine overactivity may underlie anorexia nervosa and that medications that block dopamine receptors in the brain—say, second-generation antipsychotics—might be of some benefit to persons with the illness. The second-generation antipsychotics are also known to promote weight gain, which patients with anorexia nervosa desperately need.
However, “there have not been any double-blind, placebo-controlled trials of atypical antipsychotic medications in anorexia nervosa subjects,” Kaye said. “That is one thing that really needs to be done.”
Yager agreed. “We know that some clinicians are starting to use atypical antipsychotic medications to help facilitate weight gain in malnourished anorexia nervosa patients, but we still lack both controlled trials and long-term studies to show whether these have any true added value and/or sustaining power that may outweigh potential adverse reactions to taking these medications. Thus, during the next five or 10 years, we can anticipate trials of atypical antipsychotics for acute anorexia nervosa.”
Regarding promising new treatments for bulimia nervosa, Mitchell and colleagues conducted a study of 117 subjects with the disorder to see whether conducting CBT via telepsychiatry is as effective, and as acceptable, as when it is conducted face to face. The answer was yes on both counts, Mitchell reported at APA's 2005 annual meeting in May.
Regarding propitious new therapies for binge-eating disorder, Susan McElroy, M.D., a professor of psychiatry at the University of Cincinnati, and coworkers enrolled 61 obese subjects with binge-eating disorder in a 14-week randomized, double-blind, placebo-controlled study in which subjects received either the anticonvulsant topiramate or a placebo. Those who completed the study were also offered participation in a 42-week, open-label extension trial of topiramate.
Forty-three subjects from both the double-blind study and the open-label trial provided outcome measures. The average duration of topiramate treatment was 21 weeks. From baseline to outcome, all of them experienced a significant decrease in binge eating and in weight, McElroy and her team reported in the November 2004 Journal of Clinical Psychiatry.
Nonetheless, the researchers admitted, a fairly large number of subjects dropped out of their study and trial, either because of protocol nonadherence or because of adverse side effects from topiramate.
Noncompliance can also pose a dilemma in anorexia nervosa trials. For example, Katherine Halmi, M.D., a professor of psychiatry at Weill Cornell Medical College, and colleagues enrolled 122 patients with the illness in a study in which subjects received CBT, an SSRI antidepressant, or both for a year. The dropout rate was 56 out of 122, or 46 percent, they reported in the July Archives of General Psychiatry.
Sometimes it is difficult to get eating-disorder patients to enter treatment trials in the first place. For instance, several years ago Michael Devlin, M.D., clinical codirector of eating disorders research at New York State Psychiatric Institute, and coworkers attempted to recruit obese individuals with a binge-eating problem into a treatment trial in which CBT or an SSRI would be tested as add-on therapy to a more traditional weight-loss program. The program emphasized mostly healthy eating, a healthy lifestyle, self-acceptance, and, to a lesser degree, weight loss.
“Often they would call up, express interest, make an appointment for intake, but then wouldn't show up,” Devlin said in an interview. The reason why, he suspected, is that “many obese people have had so many disappointing experiences with dieting that they feel very discouraged.”
Often individuals with eating disorders do not want treatment at all. This is especially true for persons with anorexia nervosa who are over 18 years of age, Halmi told Psychiatric News. That is why treating them before they turn 18 is so crucial, she explained, and why family involvement in treatment before they turn 18—the age of majority—is also so vital.
Thus, finding some way to motivate eating-disorder patients both to seek treatment and to stick with it would surely constitute a“ breakthrough” in the conquest of eating disorders. And when all is said and done, motivation may be as crucial as treatment per se.
Take the case of 35-year-old “Cindy T.,” who had anorexia nervosa since age 13. She had osteoporosis, had lost most of her teeth, and had been close to dying on several occasions. “A lot of people had given up on her,” Mitchell said. “But she eventually recovered and is doing very well now.”
“Part of the reason why she did recover,” Mitchell observed,“ was her own motivation to change. She was tired of living her life that way and made a commitment to do things differently.” ▪