Recent estimates suggest that about 8 percent of the working population in the United States has an alcohol problem, but health plans reported that fewer than 1 percent of their members are diagnosed with serious alcohol problems. That means that less than 10 percent of employees with alcohol problems are diagnosed with the disorder.
For depression, the numbers are only slightly better. It's estimated that about 9 percent of the working population has a depressive episode in a 12-month period. Surveyed health plans said that 3.6 percent of their enrollees were found to have depression, which is about 40 percent of the number who would be expected to have depression.
By comparison, 65 percent of those with type II diabetes were properly diagnosed, the plans said, and 70 percent of those with hypertension were identified.
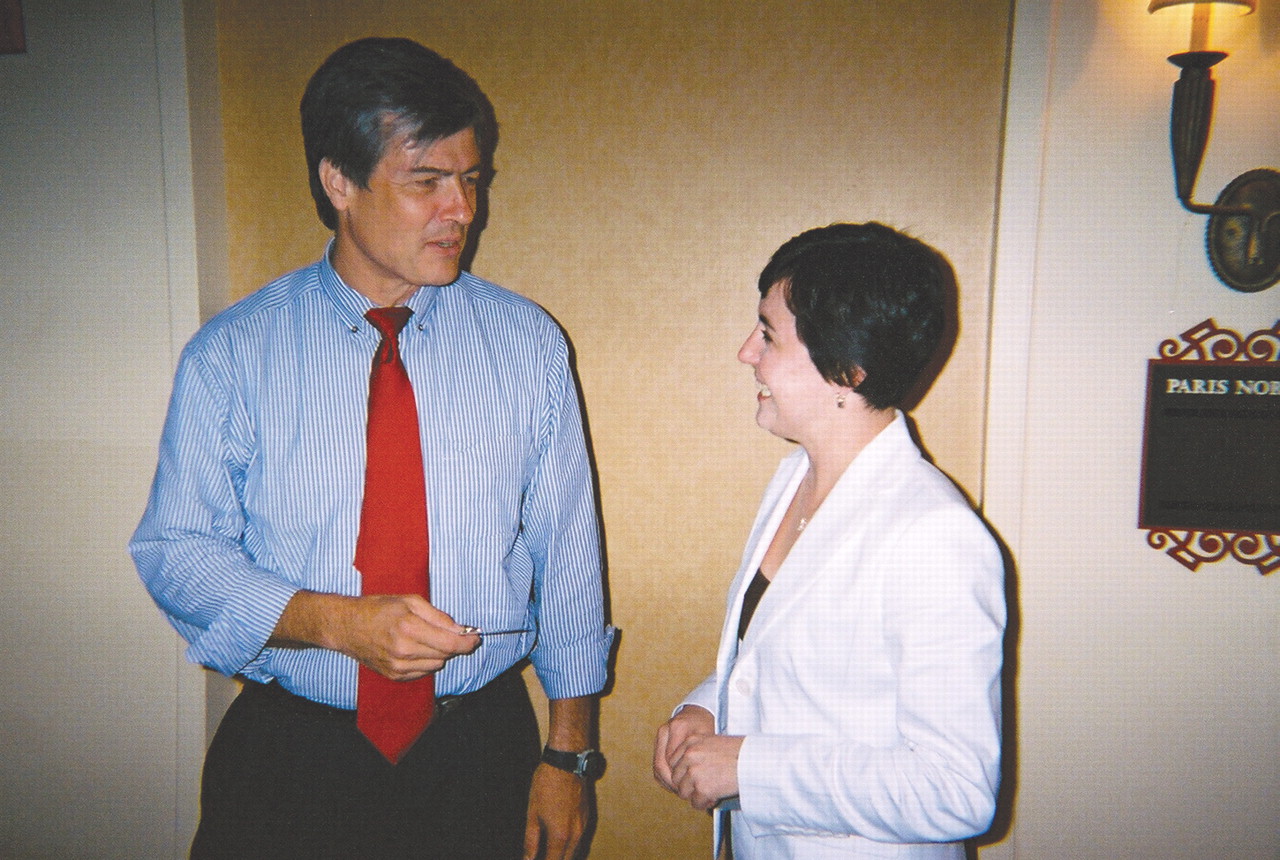
Eric Goplerud, Ph.D., director of the program Ensuring Solutions to Alcohol Problems at George Washington University Medical Center in Washington, D.C., presented these findings to nearly 200 health plan representatives attending an “eValue8” User's Meeting in Chicago in July.
“eValue8” evaluates health plans and is a program of the National Business Coalition on Health (NBCH), which is a membership organization of regional employer coalitions. Its purpose is to improve health care quality. NBCH represents companies that employ more than 3 million people nationwide.
Health plans voluntarily submit their data annually to eValue8 staff, and employers use the results of these surveys to compare health plans and evaluate health plan performance.
Why do health plans go through the trouble of completing these time-consuming surveys? Because employers are demanding it. “It's a way for employers to drive plans toward a higher standard,” Goplerud told Psychiatric News. “Employer expectations are higher than they were five years ago.”
The 2005 survey results included more than 250 health plans in 27 states. Participating companies and organizations included American Express, General Motors, Marriott International, Pacific Business Group on Health, Pitney Bowes, Safeway, Target, Greater Detroit Area Health Council, New York Business Group on Health (NYBGH), and other state and regional business coalitions.
Wide Variability Evident
This year's results showed a wide variability in the services the plans provide. Within 14 days of being diagnosed, only 44 percent of insured plan members identified as alcohol dependent attended even a single alcohol or drug treatment session. Only about 16 percent received the recommended “three chemical dependency health care services” in the month following diagnosis.
“In some cases, only 1 person per 1,000 individuals is getting what we would consider standard evidence-based care for alcohol use disorders,” noted Goplerud. Few plans send educational materials to their plan participants, and only 17 percent make follow-up calls to members who miss appointments.
For depression, about 25 percent of the plans said they were able to follow up with between 66 percent and 90 percent of their patients within seven days of a psychiatric hospitalization; however, 6 percent said they didn't track depression patients.
Although there was wide variability in the management of antidepressant medications, 58 percent of the plans, on average, said that they followed evidence-based guidelines.
On a more optimistic note, 75 percent of plans responding to the survey expect primary care physicians and behavioral health care practitioners to screen patients for alcohol problems. Although employers have routinely recommended that health plans screen for depression, only 64 percent of the plans do so.
“Even though it's clear that the diagnosis and treatment of depression are coming along,” said Goplerud, “you'd think we'd be doing better given the impact of alcohol and depression in the workplace.”
He noted that the health plans' improved diabetes care and follow-up show that they know how to improve the diagnosis and treatment of targeted conditions. “They did it for diabetes,” he said.
Employers Take Lead
In response to increased employer scrutiny, such as through the eValue8 program, health plans are taking steps to expand and strengthen their mental health care services.
For instance, some employers are beginning to work with health plans, as well as with clinicians and consumer groups, to improve diagnosis of alcohol abuse and depression and provide follow-up care.
“We find, though, that collaboration is not yet a common occurrence in the behavioral health arena,” said Goplerud. When NYBGH asked Ensuring Solutions to analyze and compare its performance with national plans, researchers found that NYBGH did better than average on general education of plan members and fairly well on outcome measures, but fell way behind on amount of collaboration with other groups.
Clare Miller, director of the American Psychiatric Foundation's Partnership for Workplace Mental Health and APA's business outreach project, attended the users' meeting in Chicago and said that the fact that alcohol use disorders and depression are now being tracked by eValue8 should raise employer awareness and lead to positive changes.
“We're encouraged after hearing the response of health plans to the survey results, and we look forward to working with the NBCH on this important project,” she said.
Information on addressing alcohol problems in the workplace is posted at<www.ensuringsolutions.org>.▪