Hoping for the best, but preparing for the worst, mental health advocates are bracing for the start of Medicare's new Part D prescription drug benefit in January like islanders awaiting a momentous change in the weather with only vague forecasts—it could be really good, or it could be really, really bad.
When the new program begins January 1, 2006, some 40 million Medicare beneficiaries, including “dual eligibles” who receive both Medicare and Medicaid benefits—as many as 2.5 million of whom have mental illness—will be eligible for prescription drug coverage.
A component of the Medicare Modernization Act of 2003, the new program is hailed by the Bush administration as an historic opportunity for millions of Americans to receive government-subsidized coverage of prescription drugs. A report by the Medicare Today coalition found that the amount of money low-income seniors spend on prescription drugs will fall nearly 90 percent under the new program. The approximately 8 million beneficiaries who earn 150 percent of the federal poverty level or less—approximately $14,500 annually—will see their out-of-pocket costs for prescription medications drop from $1,657 to $180 a year, according to the analysis.
Medicare Today is a broad-based partnership of organizations representing seniors, patients, health care groups, employers, and others.
Preparing for Worst-Case Scenarios
So much for the good news.
APA has taken the lead in preparing for—and trying to head off—countless worstcase scenarios and potential problems in the new program identified by mental health advocacy groups. In collaboration with the National Alliance for the Mentally Ill and the National Mental Health Association, APA is sponsoring a Web site at<www.mentalhealthpartd.org> intended to be an all-purpose site for resources related to the Part D program for psychiatrists, mental health professionals, and the public.
Among the most prominent concerns with the new program are communicating with and educating beneficiaries who may be only vaguely aware of the existence of the program, never mind its specific benefits; potential problems with plan enrollment; possible formulary exclusions and restrictions; continuity of care issues; and issues with premium payments and deductibles that may be severe financial hardships for the poorest and most severely ill individuals.
Also of great uncertainty is the status of medications used to treat substance abuse (see story at bottom of facing page).
Moreover, Part D is unusually complex—even by Washington bureaucratic standards—in part because of the complicated financing mechanisms by which the entire act was made to come in under the budget expectations of the Republican majority who approved it.
For instance, imbedded in the formula for financing the program is a provision requiring states to pay a portion of the costs they will no longer incur for drug coverage under their Medicaid programs—the so-called“ clawback formula,” an unintended consequence of which could be to cause states to drop patients from their Medicaid rolls (see story at top of facing page).
Transition May Be Rocky
The focus of APA and other advocates has been most keenly on that special category of beneficiaries who qualify for both Medicare and Medicaid by virtue of age and/or poverty and disability, many of whom have mental illness. Their drug coverage under the Medicaid program will cease on January 1, 2006, when the new Medicare Part D program begins.
Mental health advocates say the new benefit could prove tricky to navigate for a population that may be cognitively impaired or may not read its mail. Many are predicting a rocky transition from a Medicaid program that had been providing reasonable access to prescription drugs, including psychiatric medications, to a new program in which the drug plan formularies are unknown at press time.
APA has been active in negotiating with the federal Centers for Medicare and Medicaid Services (CMS) to ensure that psychiatric drugs are included in the formularies of the prescription drug plans (PDPs). Marketing of those plans begins this month.
“We are talking about moving people from 50 state programs, which for the most part have had relatively unrestricted access to psychiatric drugs, to a new program in which we don't yet know what the formularies will look like,” said Irvin Muszynski, J.D., director of APA's Office of Healthcare Systems and Financing. “We know for certain that for the dual eligibles it's going to be a major change. Whether it's good or bad depends on a number of things that we don't know yet. Most important is what the final prescription drug formularies will actually look like with regard to the relevant psychiatric medications and what kind of access restrictions may apply.”
“Cautiously optimistic” is how Jennifer Bright, senior vice president of state policy for the National Mental Health Association, characterized expectations about the new program. “For dual eligibles, it's a question mark because we don't know what the plans look like. CMS has told us that all our concerns are going to be met, but we won't know that until the middle of October.
“At that point, we will essentially have six to eight weeks to evaluate how good the plans are and communicate it to a couple of million people,” Bright told Psychiatric News. “It's a waiting game.”
By statute, benzodiazepines will not be on drug plan formularies, though Bright noted that legislation has been introduced in Congress to include that class of drugs (Psychiatric News, August 5).
Marc Steinberg of Families USA said that many state Medicaid plans have opted to provide benzodiazepine coverage. “They can continue to cover them if they wish to, and in fact CMS is urging states to continue to cover these drugs,” Steinberg told Psychiatric News. “After January 1, dual eligibles could then have two sources of drug coverage—Part D for most medications and Medicaid as secondary coverage for nonPart D drugs, like benzodiazepines.
“Not so easy for anyone to understand, especially someone with mental illness, but workable in theory,” Steinberg said.
What to Watch For
Yet it is just such convolutions that seem to characterize many aspects of the new program, especially for the dual eligibles. Following are just a few of the most crucial issues and potential problems for both the dual eligibles and the regular Medicare beneficiaries that APA and other mental health advocates are following:
•
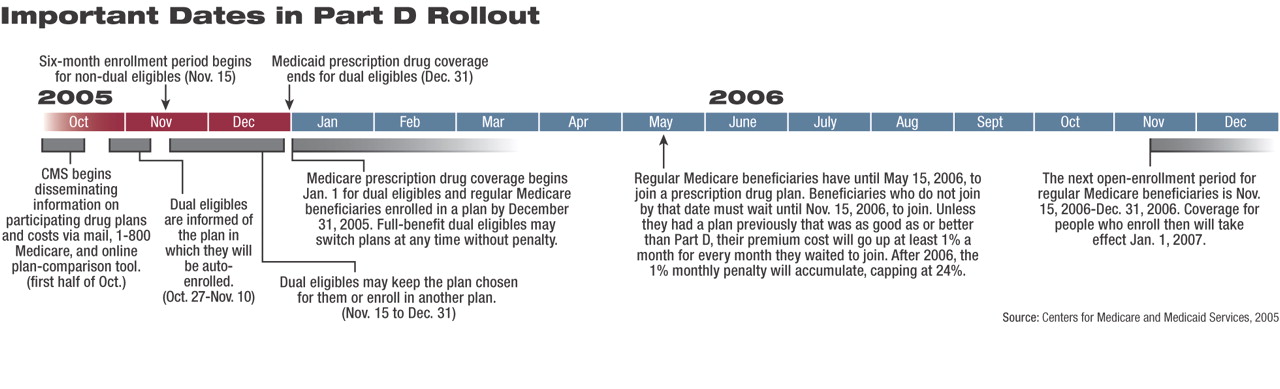
Enrollment: Starting October 27, CMS will notify dual eligibles of the plan into which they will be auto-enrolled if they do not enroll themselves in a plan before January 1, 2006. They will also receive a low-income subsidy to cover their premium, but if they choose their own plan and it has a premium greater than the subsidy, they will be responsible for paying the difference.
“That difference can be a substantial burden to someone on a small fixed income,” Muszynski noted.
For most beneficiaries who are only in the Medicare program, there is a somewhat convoluted system of deadlines (and penalties for missing deadlines) that appears designed to provide a powerful incentive to join a PDP so that a large enough pool of enrollees will be created to support the program. According to CMS, those beneficiaries have until May 15, 2006, to enroll in a PDP; if they do not enroll by then, they will not be able to enroll again until November 15, 2006, and they will be charged a penalty of 1 percent of the PDP premium for each month during which they were not enrolled. After 2006 there will be an annual enrollment period beginning November 15, and the 1 percent per month penalty will accumulate, capping at 24 percent.
•
Formularies, Access Restrictions, and Continuity of Care: Muszynski said that CMS has assured APA and other advocacy groups that “all or substantially all” of six classes of drugs (antidepressants, antipsychotics, anticonvulsants, antineoplastics, immunosuppressive drugs, and HIV drugs) will be on PDP formularies.
But Muszynski noted that “the fact that a drug is on a formulary doesn't mean it won't be subject to some hurdle.” These can include requirements for “step therapy”—proving that prior usage of another medication was unsuccessful—and for preauthorization. Indeed, CMS has stated that step therapy may be an acceptable management technique for beneficiaries starting on a prescription drug plan (“new starts”).
In an August 12 letter to CMS Administrator Mark McClellan, M.D., APA Medical Director James H. Scully Jr., M.D., protested the use of such strategies and the administrative burden they would place on clinicians.
“Medications for mental illness have a latency period [between administration of the drug and achievement of therapeutic value] that is markedly longer than [that of] the other classes,” wrote Scully.“ Therefore, we are highly concerned with the implication that management techniques such as step therapy are acceptable for new starts.... Given the long latency period, step therapy places psychiatric patients in a disproportionately unjust position compared to other patients.”
Meanwhile, Muszynski said, CMS has stated that it wants to ensure that patients who are “stabilized” on a particular medication have ready access to that medication during the transition period. But how PDPs will know who the affected patients are remains a question.
In the same August 12 letter, APA recommended the use of an identity code for dual eligibles that would be assigned to their prescription drug card so that preauthorization or step requirements would be overridden.
Finally, Muszynski urges psychiatrists who are treating dual eligibles to refill prescriptions for patients prior to December 31, 2005, to the extent allowable under the state Medicaid program.
•
Copayments: Under the Medicaid program, many states do not charge copayments for drugs, and when they exist, they must be waived if the patient cannot make the copayment. But the new Part D program will charge noninstitutionalized dual eligibles with income under 100 percent of the federal poverty level a $1 copayment for generic drugs and a $3 copayment for nongeneric drugs. Those with incomes over 100 percent will have $2 and $5 copayments, respectively.
“These are higher than in most states in Medicaid now,” said Families USA's Steinberg. “Plus these copays are indexed to inflation, so they will increase over time. This could be a real hardship for very-low-income people.”
Muszynski remarked that many of the most troubling glitches in the transition to the new program will be, so to speak, “on the ground”—when a cognitively impaired patient who does not routinely open and read mail misses a vital communication about eligibility for a low-income subsidy or enrollment in a plan that may or may not cover the individual's medications.
“My greatest concern is that even if the formularies are perfect, it's the little logistical things that could go wrong,” he said. He cited the example of a patient who does not have the cash to make a copayment at the point of sale. “What happens to the patient then?” he asked. “Is he just told to go away?
“Ultimately, the Part D program is essentially a capitated model to pay for drugs,” Muszynski said. “That may work actuarially, but we are dealing with populations that have chronic and enduring illness. They don't fit the average, and the program creates incentives to stint on care.”
Medicare Today's report, “Medicare Tomorrow: Future Savings for Beneficiaries,” can be accessed at<www.medicaretoday.org/index.php?src=gendocs&link=toolbox>.▪