From the outside, 309 North Charles Street in downtown Baltimore looks like a conventional office building. However, its second and fourth floors contain something not at all commonplace—the Institute for Mental Health Ministry.
There is nothing else like it in the United States, its creator, Michael Torres, M.D., believes, although some churches do offer mental health counseling.
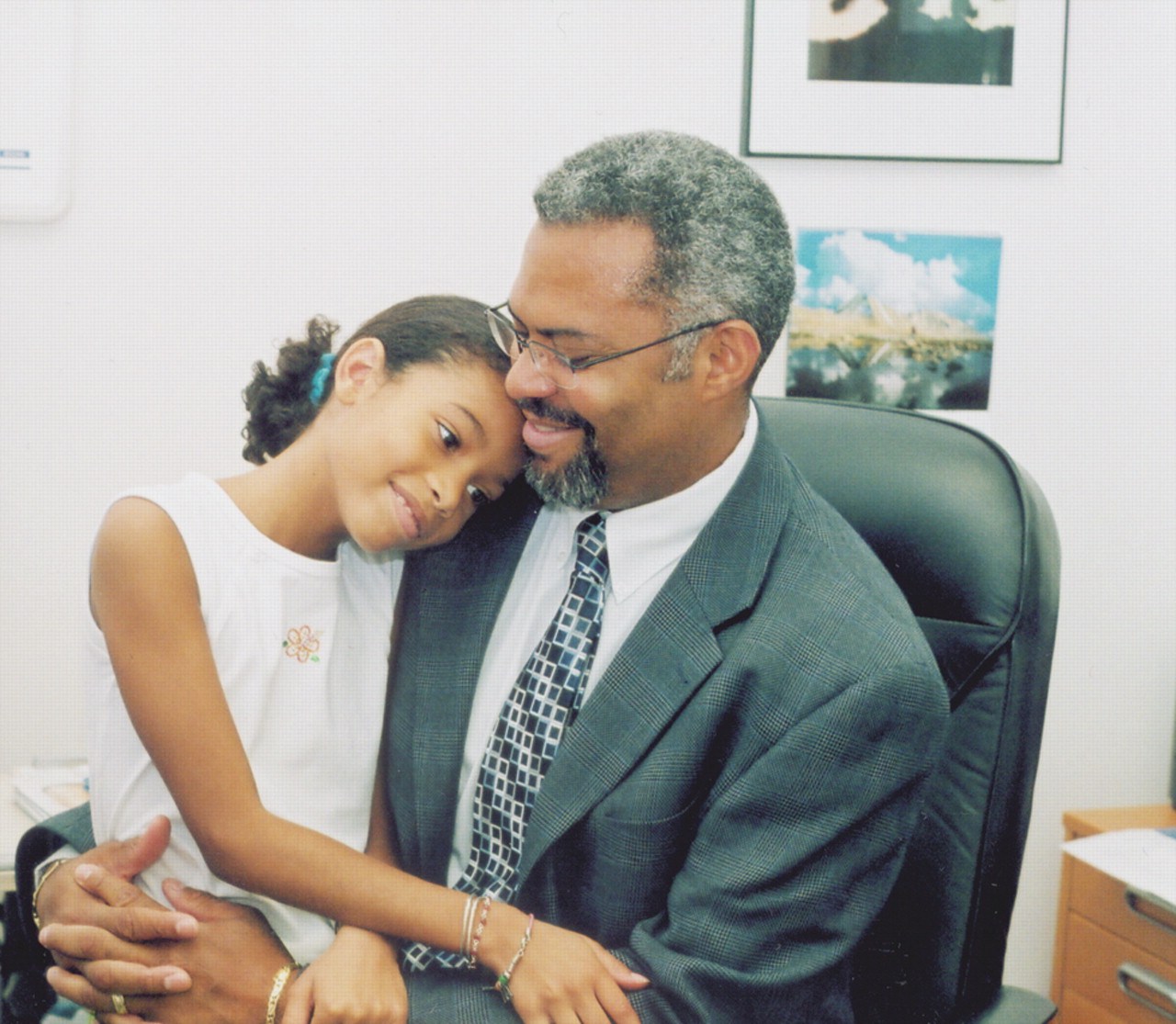
Torres himself is also unusual—both a psychiatrist and an ordained Protestant minister. He has heard of other psychiatrists who are also“ men of the cloth,” but has never met any of them.
Torres, whom psychiatrist colleagues describe as “organized, calm spirited, and very effective when it comes to putting things together to achieve a goal,” launched the institute in November 2001, with the help of various mental health professionals and church pastors. Its goal is to help people integrate mental and spiritual health.
For example, the institute offers conferences and lectures to the public on how to deal with mental health issues from both a mental health and spiritual perspective. It educates clergy about mental illness. It reaches out to church members to destigmatize mental illness and increase awareness of mental health resources. And it offers people mental health care not only at rates they find affordable but within a spiritual and religious context if they so desire.
The institute has served some 240 patients not only from various racial and ethnic backgrounds, but from different religious ones as well.
Currently Torres is the sole provider of mental health services at the institute, although it has used contracted clinical social workers in the past.
Torres calls the model he uses in providing such services—in fact, the model that guides all institute services—the“ bio-psycho-spiritual model.” It means that each person has three dimensions—mind, body, and spirit—and that if there is an imbalance in any one of those dimensions, it is going to affect the other two. It also means that for a person with mental illness to achieve optimal recovery, all three dimensions need to be addressed.
Challenges Must Be Faced
Yet putting the model into practice can be fraught with challenges, Torres admitted. For example, some religious individuals have sought help reluctantly because they believe that if they are healthy from a spiritual perspective, they should not be subject to mental illness. Others who accept psychotropic medications may wish to stop them once they feel better because they believe personal and spiritual strengths are able to take over; their stance reflects a limited understanding of the role of the biological dimension of their illness, he noted.
But Torres's hard efforts to practice the bio-psycho-spiritual model have also led to some heartening clinical successes.
Twenty-six-year-old “Bob,” for instance, came to Torres for help. “It was clear to me in that initial session that he was dealing with severe major depression and obsessive-compulsive disorder,” said Torres. “And what was fascinating was that the obsessive-compulsive disorder had taken on religious undertones, such that he spent an enormous amount of time praying and reading the Bible. And he experienced it as a real burden, as something that no matter what he did, he couldn't escape. So at that point he was very angry with God and wanted nothing more to do with religion.
“So we began a journey of addressing the symptoms, which resolved very nicely with standard medication and therapy,” Torres said.“ And he came to understand that his obsession with praying and reading the Bible, which he found so burdensome, was due to chemical imbalances in his brain and that these imbalances could be corrected. We were then able to help him reconcile with the positive aspects of his sense of spirituality.”
Then there was 35-year-old “Teresa.” “She created a lot of anxiety for me,” Torres admitted, “because she had major depression, panic disorder, and anorexia nervosa and was really at death's door. For three years, I provided her with psychotherapy and psychotropic medications, but also positively reaffirmed the positive aspects of her religious beliefs. Finally she came to believe that suicide was not the only option for her. Today she is doing much better and has returned to work as a school guidance counselor.”
Colleagues Cite Contributions
“The institute's greatest contribution so far,” said Annelle Primm, M.D., director of the APA Office of Minority and National Affairs,“ is the creation of a dynamic partnership that is breaking new ground in engaging hard-to-reach communities with a mental health message. This message has been made relevant and palatable for two reasons: Spirituality is an active ingredient, and the faith community has endorsed it.”
“I think the institute provides wonderful educational programs that are available to the community,” Ann Hackman, M.D., said. Hackman is an assistant professor of psychiatry at the University of Maryland and an acquaintance of Torres since their psychiatry residency days at the University of Maryland. “The institute,” she added, “also puts mental health care in a context in which it becomes accessible to some individuals who might not otherwise have considered the possible benefits of treatment. Further, the institute helps the mental health system to better understand spiritual issues and concerns of the faith community.”
“In my opinion,” said Melva Green, M.D., a Reisterstown, Md., psychiatrist who has known Torres since 2003, “the greatest contribution the Institute for Mental Health Ministry has made has been to educate many faith leaders. With the sustained stigma around mental disorders, faith leaders can potentially be prohibitive toward their congregations' needing and/or seeking mental health services.”
“The demand for our services has been constant,” Torres said.“ It has really been our own limitations of time and availability that have prevented further growth. We hope to build a consortium of providers who are able to negotiate the interface between spirituality and health. We are also working on a name change that better reflects our mission—the Center for the Integration of Spirituality and Mental Health.”
“If money were no object,” Primm suggested, “the institute could develop branches or satellites around the country where mental health professionals and religious leaders of all faiths could come together, share their concepts of mental health, develop services and programs to address unmet needs, and open doors to the mental and spiritual health of communities across the nation.”
More information about the institute is posted at<www.imhm.com>.▪